Case Report
Volume 3 Issue 1 - 2019
Disc Herniation at T1-2 Level Causing Radiculopathy
Department of Orthopedic, First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
*Corresponding Author: Dr. Lipeng Yu, Department of Orthopedic, First Affiliated Hospital of Nanjing Medical University, 300 Guangzhou Road, Nanjing, Jiangsu 210000, and P.R. China.
Received: July 18, 2019; Published: July 24, 2019
Abstract
Thoracic disc herniation (TDH) is rare, especially at the upper thoracic level. Here we report a case of disc herniation at T1-2 level with radiculopathy. It is not difficulty to be diagnosed on the magnetic resonance imaging (MRI). The clinical manifestation, diagnosis and treatment of disc herniation at T1-2 level were discussed.
Introduction
Intervertebral disc herniation is a common spinal disease, and cervical and lumbar spine are prone to be affected. With the support of thoracic cage consisting of ribs and sternum, the mobility of thoracic spine is limited, so that intervertebral disc herniation rarely occurs in thoracic area, especially at the upper thoracic level [1-2]. The first case was reported by Svien and Karavitis [3] in 1954. To the best of our knowledge, 40 cases of T1-2 disc herniation, up to date, have been reported [4-5]. Here we add a new case with an intervertebral disc herniation at T1-2 level presenting with radiculopathy.
Case Report
A 75-year-old female came to outpatient and complained about upper back pain and numbness in right arm for more than 2 months accompanied by aggravation for 2 weeks, without any history of trauma. Physical examination revealed hypoesthesia in right ring and little fingers and inside of the right forearm. The muscle strength, tension and physical reflexes were normal. No Horner syndrome, or pathological reflexes were detected. On the cervical-thoracic MRI, compression of the right T1 nerve root by foraminal disc herniation at the T1-2 level was observed (Figure 1).
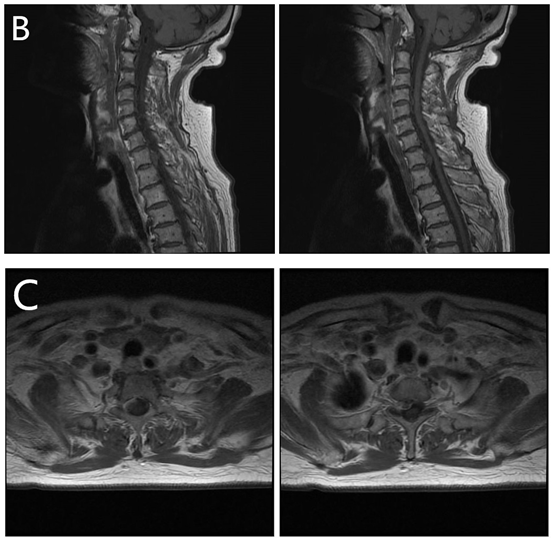
Figure 1: The cervical-thoracic MRI revealed that right T1 root
was compressed by foraminal disc herniation at the T1-2 level.
After admission, the patient was comprehensively evaluated and no surgical contraindications were found. Under general anesthesia, the patient was put on a Jackson table with prone position and T1 was located under fluoroscopy. A longitudinal incision was made from C7 to T3. After a right hemi-laminectomy at T1 –2 level with high-speed drill, bulge of dura was observed. We detected a disc fragment under the right T1 nerve root (Figure 2A) and clamped it out (Figure 2B).
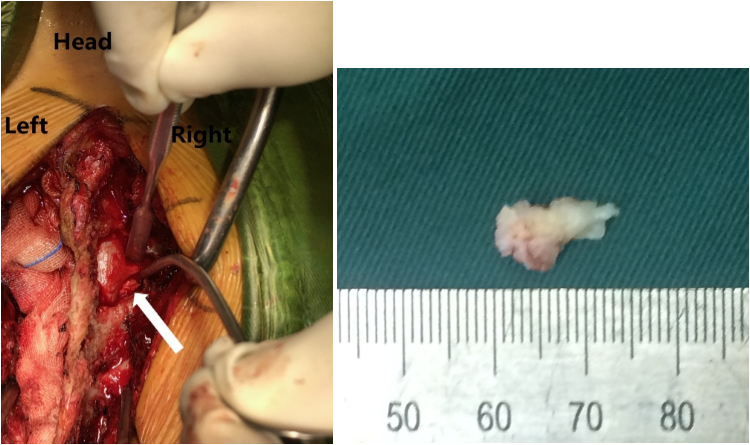
Figure 2: A disc fragment below the right T1 root was detected during the
operation. (White arrow) The length of the fragment was about 1.4 cm.
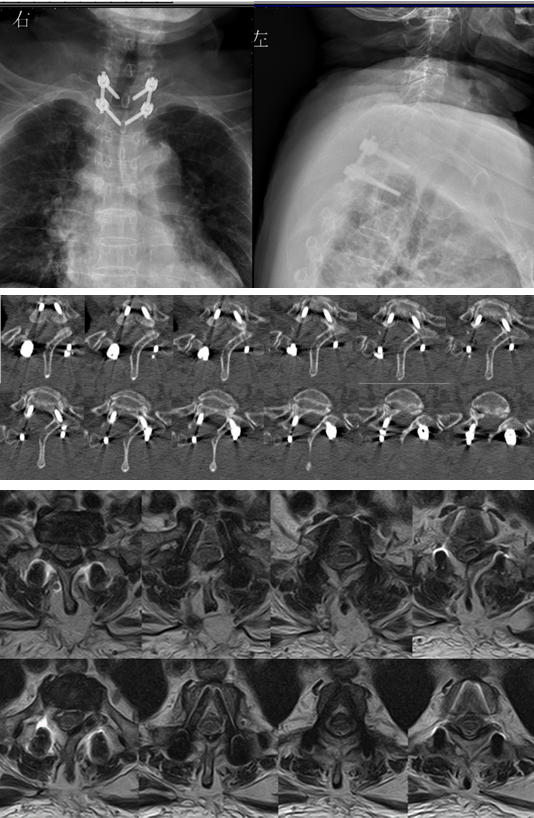
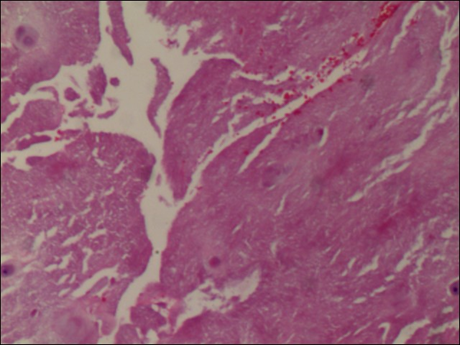
Four pedicle screws were inserted into T1 and T2 vertebra and connected with rods bilaterally. The patient’s symptoms relieved immediately after operation, without complaint of right upper limb pain and numbness. Postoperative X-ray, CT scans and MRI showed no residual disc fragment (Figure 3). Histological analysis confirmed degenerated nucleus pulposus (Figure 4). Three months later, the patient came back to outpatient without any complaint. She had a CT scans of thoracic vertebra and it seemed like that 3 months ago (Figure 5).
Discussion
Compared with cervical or lumbar spine, T1-2 disc herniation is very rare. The causes mainly include degeneration and trauma. The clinical manifestation varies depending on the location of the disc herniation. Son [4] summarized 21 cases that had been reported up to 2012, 18 cases (86%) presenting with radiating pain (on the medial aspect of the arm and 4th, 5th fingers), 17 (81%) with axial pain (on the neck and scapular area), 15 (71%) with sensory deficit (T1 dermatome), 14 (67%) with motor deficit (intrinsic muscles of hand), 7 (33%) with Horner’s syndrome (HS), 5 (24%) with chest pain and 3 (14%) with myelopathy. Spacey [5] also reported a case presenting with radiating pain, sensory and motor deficit and HS in 2014.
In our case, the patient merely suffered from C8 radiculopathy, while T1 root was compressed. We analyzed that T1 root was part of the brachial plexus, and constituted the ulnar nerve along with C8 root. Thus, T1 radiculopathy may manifested as numbness of the fourth and fifth fingers, or weakness of intrinsic muscle of hand as similar as C8 radiculopathy [6]. In this case, the right T1 root had been compressed for less than 3 months and sensory fiber function was impaired, while motor fiber was normal. It is not difficult to make a diagnosis on computed tomography (CT) scans and MRI before surgery. Obviously, laboratory investigations and electromyography (EMG) are needed to differentiate from other diseases, such as neoplasm and peripheral neuropathy.
Once TDH is diagnosed and conservative treatment is invalid, surgery is the first choice. The choice of surgical approach depends on the location, size and surgeon’s preference. Posterior approaches include laminectomy, costotransversectomy, and transpedicular and transfacet pedicle–sparing approach. Anterior approaches include thoracotomy and transmanubrial approach. Lateral approaches include lateral extracavitary approach and video-assisted thoracoscopic surgery (VATS).
Arce and Dohrmann [6] accumulated 135 cases of thoracic disc herniation who accepted simple laminectomy alone and concluded that only about 50% patients achieved functional improvement. Therefore, simple laminectomy had been abandoned gradually. Compared with mere laminectomy, costotransversectomy and transpedicular approach are relatively more effective options. In 1960, Hulme [7] first described a costotransversectomy to treat 6 patients with TDH and 4 gained improvements. Levis [8] performed discectomies by transpedicular approach to treat 35 patients, of which 23 cases presenting with myelopathy and 12 with radiculopathy, and 26 (74.3%) cases achieved improvements. Stiller man [9] reported a transfacet pedicle–sparing approach for TDH in 15 patients and also gained good results. Thus, most of the patients who had only radiculopathy and subsequently underwent posterior approach operations achieved good outcomes [10-12].
Previous literatures [13-14] showed that an anterior approach was applied in patients presenting with myelopathy. Advantages of transthoracic approaches include a better visualization of the disc space and a direct decompression of the spinal cord [15]. But Patterson and Arbit [16] performed a facectectomy and laminectomy to treat a patient presenting with myelopathy due to a central disc herniation. Meanwhile, Caner [17] carried out an anterior discectomy (manubrium split) in a patient presenting with radiculopathy due to a left disc herniation. Some studies reported that successful treatments were achieved using Southwick-Robinson approach without sternotomy, but others reported that partial sternotomy was required [14, 17, 18].
The relative position between sternum and T1-2 level should be considered before surgery, and an appropriate procedure should be prepared in advance if a sternotomy is required. However, anterior approaches produced a huge injury and put the patient at increased risk of certain cardiothoracic complications, including atelectasis, lung contusion, intercostal neuralgia, pneumothorax, hemothorax and adamkiewicsz artery injury [19-20]. Compared with traditional thoracotomy and manubrium split approach, VATS is an alternative choice. It can avoid sternotomy and the complications mentioned above, which do a favor for postoperative quick recovery. But a long learning curve is required for the surgeon.
Another viewpoint remains controversial is whether fusion is necessary or not. Fusion is recommended in the cases who underwent anterior extensive decompression, resulting in the spinal instability [21]. However, posterior and lateral approaches conserve the spinal stability. Thus, fusion may not be requested.
In conclusion, for central TDH presenting with myelopathy, no matter accompanied by calcification of the ligament or not, the recommendation of anterior approach or a VATS with fusion after extensive decompression is supported. For lateral TDH presenting with radiculopathy, a posterior approach surgery can achieve a good outcome.
References
- Arseni C and Nash F. “Thoracic intervertebral disc protrusion: a clinical study”. J Neurosurg 17 (1960): 418-30.
- Murphey F., et al. “Surgical treatment of laterally ruptured cervical disc: review of 648 cases, 1939 to 1972”. J Neurosurg 38 (1973): 679-83.
- Svien HJ and Karavitis AL. “Multiple protrusions of intervertebral disks in the upper thoracic region: report of case”. Proc Staff Meet Mayo Clin 29 (1954): 375-8.
- Son E S., et al. “Surgical Treatment of T1-2 Disc Herniation with T1 Radiculopathy: A Case Report with Review of the Literature”. Asian Spine Journal 6 (2012): 199-202.
- Spacey K., et al. “Horner's syndrome secondary to intervertebral disc herniation at the level of T1-2”. BMJ Case Rep 5 (2014): 2014.
- Arce CA. “Herniated thoracic disks”. Neurologic clinics 3.2 (1985): 383-392.
- Hulme A. “The surgical approach to thoracic intervertebral disc protrusions”. J Neurol Neurosurg Psychiatry 23 (1960): 133.
- Levi N and Gjerris F. “Thoracic disc herniation Unilateral transpedicular approach in 35 consecutive patients”. Journal of neurosurgical sciences 43.1 (1999): 37-42; discussion 42-3.
- Stillerman CB., et al. “The transfacet pedicle-sparing approach for thoracic disc removal: cadaveric morphometric analysis and preliminary clinical experience”. J Neurosurg 83 (1995): 971-976.
- Lloyd TV., et al. “Horner's syndrome secondary to herniated disc at T1--T2”. AJR. American journal of roentgenology 134.1 (1980): 184-185. DOI:10.2214/ajr.134.1.184
- Morgan H and Abood C. “Disc herniation at T1-2: report of four cases and literature review”. J Neurosurg 88 (1998): 148-50.
- Love JG and Schorn VG. “Thoracic disk protrusions”. JAMA 191 (1965): 627-31.
- Winter RB and Siebert R. “Herniated thoracic disc at T1-T2 with paraparesis: transthoracic excision and fusion, case report with 4-year follow-up”. Spine (Phila Pa 1976) 18 (1993): 782-4.
- Nakahara S and Sato T. “First thoracic disc herniation with myelopathy”. Eur Spine J 4 (1995): 366-7.
- Perot PL and Munro DD. “Transthoracic removal of midline thoracic disc protrusions causing spinal cord compression”. J Neurosurg 31 (1969): 452–458. doi:10.3171/jns.1969.31.4.0452.
- Patterson RH Jr and Arbit E. “A surgical approach through the pedicle to protruded thoracic discs”. J Neurosurg 48 (1978): 768-72.
- Caner H., et al. “Magnetic resonance image findings and surgical considerations in T1-2 disc herniation”. Can J Neurol Sci 30 (2003): 152-4.
- Rossitti S., et al. “The anterior approach to high thoracic (T1-T2) disc herniation”. Br J Neurosurg 7 (1993): 189-92.
- Logue V. “Thoracic intervertebral disc prolapse with spinal cord compression”. J Neurol Neurosurg Psychiatry 15 (1952): 227-241.
- McCormick WE and Will SF. “Surgery for thoracic disc disease Complication avoidance: overview and management”. Neurosurgical focus 9.4 (2000): e13.
- Debnath UK., et al. “Results of hemivertebrectomy and fusion for symptomatic thoracic disc herniation”. Eur Spine J 12.3 (2003): 292–299.
Citation:
Lipeng Yu., et al. “Disc Herniation at T1-2 Level Causing Radiculopathy”. Orthopaedic
Surgery and Traumatology 3.1 (2019): 16-21.
Copyright: © 2019 Lipeng Yu., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.