Case Report
Volume 5 Issue 1 - 2023
Large Morel-Lavallee Lesions of the Knee and Lower Leg Case Series and Their Subsequent Effective Surgical Management
Department of Orthopedics, Herlev and Gentofte Hospital, University of Copenhagen, Denmark
*Corresponding Author: Anton N Peterlin. Herlev and Gentofte Hospital, Borgmester Ib Juuls Vej 1, 2730 Herlev, Denmark.
Abstract
Background: Morel-Lavallée lesion (MLL) is a post traumatic soft tissue degloving injury, resulting from direct or tangential shearing forces separating skin and subcutaneous tissues from the underlying fascia. A cavity develops, which characteristically contains hemolymphatic and serosanguinous fluid. Over time, it consolidates with an organized pseudocapsule. In contrast to the frequency of traumatic injuries, MLLs are uncommon, difficult to diagnose, and complicated to treat. Current literature around MLL management is based on lesions around the hip and the trochanter.
Materials and Methods: Our case series consists of two females and one male with lower leg MLL. All presented with similar trauma of a direct and shearing force to the knee and/or the lower leg with painful and persistent lesions. Magnetic resonance imaging and ultrasound represented the critical diagnostic studies. Operative treatment included uniform surgical debridement with the preservation of dermal vascularity, followed by capsulectomy, and partial wound closure using black foam NPWT, which was retracted over two revisions in the outpatient clinic.
Results: All patients underwent a single and effective operative debridement, were hospitalized for less than 5 days, had two NPWT changes, and their treatment ended within two to three weeks. At their 12 month follow up, all patients were symptom free apart from decreased cutaneous sensation which was already present prior to surgery in two of the three cases.
Conclusions: MLLs of the lower leg and knee are sparsely reported in the literature, making the disease difficult to diagnose and treat. In our case series, we reported an easy-to-follow diagnostic routine as well as a novel surgical treatment management which included debridement, capsulectomy and secondary management with NPWT in an outpatient setting. The operative methods resulted in excellent healing results with pain free motion.
Keywords: Closed degloving injury; Morel-Lavallée Lesion (MLL); Posttraumatic pseudocyst; Lower leg; Surgical management; Negative pressure wound therapy (NPWT)
Introduction
Morel-Lavallée lesion (MLL) is a posttraumatic soft tissue degloving injury, resulting from direct or tangential shearing forces hereby separating skin and subcutaneous tissues from the underlying fascia [1-3]. A cavity characteristically containing hemolymphatic and serosanguinous fluid develops, and over time consolidates with an organized pseudocapsule [4-6]. In contrast to the frequency of traumatic injuries, MLLs are uncommon, difficult to diagnose, and difficulty to treat [6-9]. Radiological investigations, particularly magnetic resonance imaging (MRI) and ultrasound (US) represent the best modalities for the diagnosis and for following treatment [3-10].
First described in 1853, the most common location of MLL is the lateral aspect of the proximal thigh and the trochanter. MLLs of the lower leg [11,12] and knee [1-5] are only reported in a handful of cases. Furthermore, the only literature regarding MLL treatment deals with the trochanteric region [2,13]. It describes compressive bandaging and cryotherapy as the first line of treatment. However, these bandages vary in effectiveness and depend on patient compliance [13,14]. A minimally invasive aspiration coupled with sclerosing agents has also proven to be effective for lesions under 400 mL. In contrast, isolated aspirations alone, without sclerosing agents are associated with high rates of failure [7-9,14,15]. Surgical management, subsequent capsulectomy and dead space management are reserved for larger lesions of over 400 mL [7,9].
This case series presents three knee and lower leg MLLs, all of which were misdiagnosed, improperly treated, and required innovative surgical management. All were treated uniformly with optimal resolution of the lesions. To our knowledge, this is the first case series in the literature, which describes the surgical management of large MLLs of the knee and lower leg.
Case Report
Case A:
A comorbid 73-year-old female with COPD, diabetes, ischemic heart disease and on anticoagulants, presented to the emergency department (ER) with right knee and deep calf pain with the suspicion of deep vein thrombosis (DVT) (Table 1). 11 days prior, the patient had fallen off an electric bicycle at low speed directly onto her right knee. DVT was ruled out by ultrasound (US). Subsequent plain radiographs and computer tomography (CT) scans demonstrated a non-displaced lateral tibial plateau fracture. These injuries were treated conservatively and over weeks failed and a painful hematoma developed that threatened skin viability. The hematoma was surgically drained, and a total of 1300 mL serosanguinous fluid was removed. Compression and immobilization were implemented, but the lesion reemerged (Figure 1 a,b).
| Patient | Age | Sex | Mechanism of Injury | BMI (kg/m2) | Anatomical Location | Associated Injuries | Open/ closed | Time to diagnosis (days) | Time to treatment (days) | Comorbidities | Medication |
| 1 | 74 | F | Direct and blunt. Electric bike. | 33,1 | Right knee | Nondisplaced tibia plateau fracture | Closed | 160 | 167 | Diabetes, ischemic heart disease, hypertension | Acetylsalicylsyre, metformin, Enalapril |
| 2 | 41 | M | Bicyclist, direct and blunt. | 23,4 | Left lower leg | None | Closed | 14 | 21 | No | None |
| 3 | 76 | F | MVA. Shearing <5km/h | 26,1 | Left knee and lower leg | None | Close | 106 | 120 | Diabetes | Metformin and Forxiga |
| M: Male; F: Female; Y: Yes; N: No, BMI: Body mass index. MVA: Motor vehicle accident. Km/h: Kilometers per hour | |||||||||||
Table 1: Patients’ characteristics with Morel-Lavallée Lesions Treated
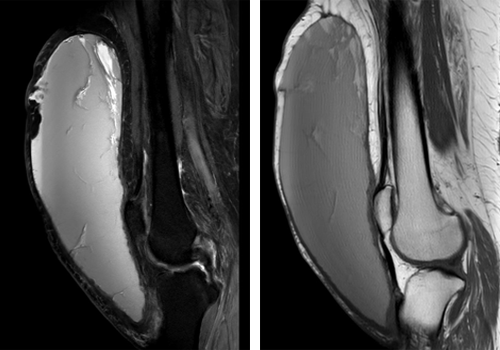
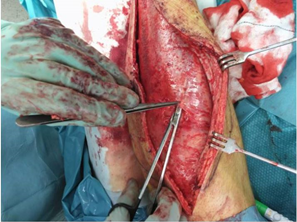
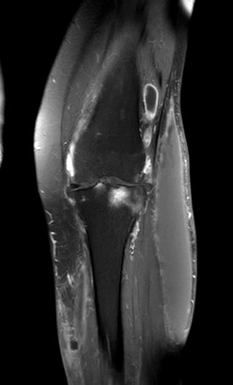
An MRI visualized a 23 x 12 x 7 cm (1932 mL) inhomogeneous fluid filled cavity, with fat necrosis, pseudo-cyst walls, low T1 signal and increased short T1 inversion recovery (STIR) signaling (Figure 1 c,d). Due to the size and anatomical location, open debridement, capsulectomy, partial wound closure and NPWT were advised. Following two outpatient changes of the NPWT, the cavity and wound were closed less than three weeks after the surgery (Figure 1 e,f). After discharge the patient was free of swelling and pain. She recovered nearly full range of motion. At the 18 months follow up, she is fully recovered and mobile.
Figure 1: a,b Before open debridement and capsulotomy. c,d) MRI sagitall STIR and T1 weighted images of the knee
and lower leg, with fat necrosis, as well as apseudocapsule arrow.
e) opendebridement with capsule. f) NPWT treatment in outpatient setting
and lower leg, with fat necrosis, as well as apseudocapsule arrow.
e) opendebridement with capsule. f) NPWT treatment in outpatient setting
Case B:
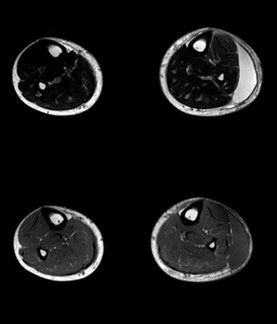
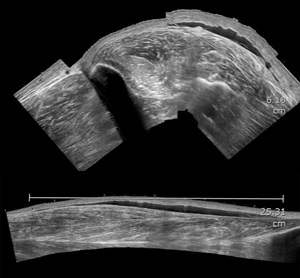
A 41-year-old healthy male was hit below his left knee while bicycling by a low speed right turning car. A hematoma and shallow skin abrasion of the anterior lateral aspect of the lower left leg were the only apparent injuries (Figure 2 a). Two weeks later, he presented to the ER again due to a painful, large hematoma with granulated scabs on his lower leg. There was no sign of infection. US was performed, showing a fusiform homogenic hypoechoic fluid between the fascia and dermis. The hypermobile seroma measured 25 x 7 cm with a central eschar. Five days later, the patient underwent an MRI confirming the MLL. The fluid filled mass measured 28 x 6.6 x 2.2 cm (407 mL) (Figure 2 b-d). Soon after the patient underwent open debridement and capsulectomy with vascular preservation (Figure 2 e). NPWT was once again used together with partial wound closure. After two NPWT changes, the patient was discharged 7 days after the first operation. Only local wound treatment followed. At one year follow up there has been no reemergence of the lesion. He complained of decreased cutaneous sensation around the scar, which was present before surgery. The patient was already fully mobilized after being discharged and at 18 months follow up has resumed his usual physical activity.
A 41-year-old healthy male was hit below his left knee while bicycling by a low speed right turning car. A hematoma and shallow skin abrasion of the anterior lateral aspect of the lower left leg were the only apparent injuries (Figure 2 a). Two weeks later, he presented to the ER again due to a painful, large hematoma with granulated scabs on his lower leg. There was no sign of infection. US was performed, showing a fusiform homogenic hypoechoic fluid between the fascia and dermis. The hypermobile seroma measured 25 x 7 cm with a central eschar. Five days later, the patient underwent an MRI confirming the MLL. The fluid filled mass measured 28 x 6.6 x 2.2 cm (407 mL) (Figure 2 b-d). Soon after the patient underwent open debridement and capsulectomy with vascular preservation (Figure 2 e). NPWT was once again used together with partial wound closure. After two NPWT changes, the patient was discharged 7 days after the first operation. Only local wound treatment followed. At one year follow up there has been no reemergence of the lesion. He complained of decreased cutaneous sensation around the scar, which was present before surgery. The patient was already fully mobilized after being discharged and at 18 months follow up has resumed his usual physical activity.
Figure 2: a) MLL before with eschar. b) Axial MRI scanning with STIR and T1 weighted imagaes,
c) coronal MRI STIR d) Ultrasound hypoekkotic, fusiform, e) Fibrous capsule in open debridement.
c) coronal MRI STIR d) Ultrasound hypoekkotic, fusiform, e) Fibrous capsule in open debridement.
Case C:
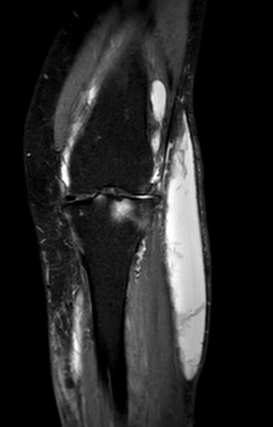
A 76-year-old female with type 2 diabetes (on Metformin and Forxiga) had her lower left leg run over by a taxi resulting in a hematoma on the lateral aspect of the knee and lower leg. Plain radiographs demonstrated no fracture, and her treatment was conservative. 5 days later, she presented to the ER with a possible compartment syndrome, which was ruled out. Four months later, the patient was referred to our hospital for an evaluation of the persistent large swelling on her lower left leg (Figure 3 a). An MRI demonstrated a homogenous 22 x 6,5 x 3 cm (429 mL) fusiform mass suggesting MLL (Figure 3 b,c). Her MLL was on the lateral aspect of the left knee and extended 15 cm. Once again, the same operative techniques were used as in the previous two cases. Two NPWT changes in the outpatient clinic were also administered (Figure 3 d,e). One year after surgery, the patient’s only complaint was decreased cutaneous sensation. She mobilized fully at her previous physical activity levels.
A 76-year-old female with type 2 diabetes (on Metformin and Forxiga) had her lower left leg run over by a taxi resulting in a hematoma on the lateral aspect of the knee and lower leg. Plain radiographs demonstrated no fracture, and her treatment was conservative. 5 days later, she presented to the ER with a possible compartment syndrome, which was ruled out. Four months later, the patient was referred to our hospital for an evaluation of the persistent large swelling on her lower left leg (Figure 3 a). An MRI demonstrated a homogenous 22 x 6,5 x 3 cm (429 mL) fusiform mass suggesting MLL (Figure 3 b,c). Her MLL was on the lateral aspect of the left knee and extended 15 cm. Once again, the same operative techniques were used as in the previous two cases. Two NPWT changes in the outpatient clinic were also administered (Figure 3 d,e). One year after surgery, the patient’s only complaint was decreased cutaneous sensation. She mobilized fully at her previous physical activity levels.
Figure 3: a) Prior to surgery with mass on lower leg and knee. b,c) MRI T1 and STIR sequences with respectived findings.
d) NPWT treatment in outpatient clinic with partial closure and black foam. e) wound closure at 3 months follow up
d) NPWT treatment in outpatient clinic with partial closure and black foam. e) wound closure at 3 months follow up
Discussion
Morel-Lavallée Lesions are often misdiagnosed or diagnosed late and often improperly treated due to their clinical complexity [16]. They are also uncommon and heterogenous sequelae after trauma. Our cases were no different. In turn, delayed diagnosis can result in suboptimal treatment. This delay allows for the formation of a hemolymphatic lesion, full of hemosiderin, in the fibrous capsule, which is lined by mesothelium that allows for the persistence of the lesion [3]. MRI and US represent the best diagnostic tests. MRI visualizes well-defined oval or fusiform fluid filled cystic structures with low signal intensity on T1 weighted images and high signal mass in T2 weighted images with fat saturation. Ultrasound reveals a heterogeneous or hypoechogenic mass [10,17]. These modalities proved critical for the diagnosis of our three cases. This finding emphasizes their use for the proper diagnosis of MLL.
Current treatment algorithms for MLLs are based around the trochanter region and are stratified by either size or chronicity or a combination [6,7,9]. For example, Singh., et al. uses 400 mL as the size requiring open debridement, while Shen., et al. classifies MLL as chronic condition with the formation of a pseudocapsule [7,18]. Chronicity in our cases ranged from 3 weeks to 5 months. All patients had pseudocapsules with an estimated volume over 400 mL. Although there is no literature for the time of fibrous capsule formation, our shortest interval was three weeks after the trauma. Therefore, this pseudocapsule is both disease specific as well as pivotal for the surgical debridement. This finding complicated Case A, where the hematoma was evacuated without addressing the fibrous capsule and the lesion reemerged shortly thereafter. Current literature supports this conclusion and indicates the need to evacuate not only contents of these lesions but also the capsule [2,13,19].
Thus, both content and capsule must be removed. Treatment algorithms are based on the trochanteric region and employ methods such as quilting sutures, surgical drains, glue, and sclerosing agents [6,7,9]. The use of NPWT in MLL has been described only in one previous case around the gluteus, which resolved successfully [19]. NPWT was used in all our cases, not only due to the anatomical limitations of the lower leg and knee, but also for the proven benefits of NPWT. They include NPWT’s ability to eliminate dead space, promote vascular growth, maintain sterility, remove excess fluid and promotes apposition of the cavity walls [6,8,19]. Finally, the ability to change NPWT in an outpatient setting reduces the length of hospitalization.
Although complications in the form of infection and recurrence are reported in literature, our three cases were free of both [6,8]. Furthermore, chemical sclerodesis, another method described to manage cavity reformation can result in contour deformities [15]. In contrast, our use of NPWT and surgical treatment eliminated these complications. Two of the three cases had decreased cutaneous sensation due to the trauma, which was not resolved after surgical management of the MLL.
Conclusion
MLL of the lower leg and knee are sparsely reported in the literature, making these conditions difficult to diagnose and treat. In our case series, we reported an easy to manage diagnostic routine as well as a comprehensive surgical treatment, which included debridement, capsulectomy, and secondary management with NPWT in an outpatient setting. The operative methods resulted in excellent healing results with pain free motion. We recommend our treatment strategy for large MLL of the lower leg and knee as it is simple, complication free, and yielding excellent results.
References
- Van Gennip S., et al. “Pain at the knee: the Morel-Lavallée lesion, a case series”. Clinical Journal of Sport Medicine 22.2 (2012): 163-166.
- Carlson DWA., et al. “Morel-lavalée lesions treated with debridement and meticulous dead space closure: surgical technique”. Journal of Orthopaedic Trauma 21.2 (2007): 140-144.
- Mellado JM and Bencardino JT. “Morel-Lavallée lesion: review with emphasis on MR imaging”. Magnetic Resonance Imaging Clinics of North America 13.4 (2005): 775-782.
- Garner A., et al. “Morel-Lavallée lesions of the knee: a closed degloving injury: a report of two cases”. ANZ Journal of Surgery 84.10 (2014): 789-791.
- Kininy WEL., et al. “Unusual Morel-Lavallee lesion of the knee region in an elderly patient”. BMJ Case Reports (2017): 10-13.
- Molina BJ., et al. “Practical Review of the Comprehensive Management of Morel-Lavallée Lesions”. Plastic and Reconstructive Surgery 9.10 (2021):e3850.
- Singh R., et al. “The Morel-Lavallée lesion and its management: A review of the literature”. Journal of Orthopaedics 15.4 (2018): 917-921.
- Nickerson TP., et al. “The Mayo Clinic experience with Morel-Lavallée lesions: establishment of a practice management guideline”. Journal of Trauma and Acute Care Surgery 76.2 (2014): 493-497.
- Dawre S., et al. “The Morel-Lavallee lesion: A review and a proposed algorithmic approach”. European Journal of Plastic Surgery 35.7 (2012): 489-494.
- De Coninck T., et al. “Imaging Features of Morel-Lavallée Lesions”. Journal of the Belgian Society of Radiology 101 (2017): 15.
- Falconi A., et al. “A Rare Presentation of a Morel-Lavallee Lesion of the Lower Leg Successfully Treated With Ultrasound-Guided Aspiration”. Clinical Journal of Sport Medicine 28.4 (2018): E87-E88.
- Moriarty JM., et al. “A rare cause of calf swelling: the Morel-Lavallee lesion”. Irish Journal of Medical Science 180.1 (2011): 265-268.
- Hak, David, Olson Steven, Matt J. “Diagnosis and Management of Close... Fractures_ The Morel-Lavallee Lesion..pdf”. Published online (1997).
- Tejwani SG., et al. “Management of Morel-Lavallee lesion of the knee: twenty-seven cases in the national football league”. The American Journal of Sports Medicine 35.7 (2007): 1162-1167.
- Bansal A., et al. “Doxycycline sclerodesis as a treatment option for persistent Morel-Lavallée lesions”. Injury 44.1 (2013): 66-69.
- Hudson DA. “Missed closed degloving injuries: late presentation as a contour deformity”. Plastic and Reconstructive Surgery 98.2 (1996): 334-337.
- Spain JA., et al. “Morel-Lavallée Injuries: A Multimodality Approach to Imaging Characteristics”. Academic Radiology 24.2 (2017): 220-225.
- Shen C., et al. “Efficacy of treatment in peri-pelvic Morel-Lavallee lesion: a systematic review of the literature”. Archives of Orthopaedic and Trauma Surgery 133.5 (2013): 635-640.
- Morris M., et al. “Novel management of closed degloving injuries”. The Journal of Trauma 67.4 (2009): 121-123.
Citation: Anton N Peterlin., et al. “Large Morel-Lavallee Lesions of the Knee and Lower Leg Case Series and Their Subsequent Effective Surgical Management”. Orthopaedic Surgery and Traumatology 5.1 (2023): 01-07.
Copyright: © 2023 Anton N Peterlin., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.













































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.