Case Report
Volume 1 Issue 2 - 2017
Spontaneous Pneumomediastinum and Subcutaneous Emphysema Postpartum in Primipara
1Department of gynecology and obstetrics the hospital of Kolding, Denmark
2Department of gynecology and obstetrics the hospital of Kolding, Denmark
2Department of gynecology and obstetrics the hospital of Kolding, Denmark
*Corresponding Author: Laerke Kamstrup Moser, Department of gynecology and obstetrics the hospital of Kolding, Denmark Skovbrynet 22, st tv, 6000 Kolding, Denmark.
Received: December 09, 2017; Published: December 18, 2017
Abstract
We would like to present a case where a Primipara develops Pneumomediastinum and subcutaneous emphysema following childbirth. The condition is known as Hamman’s syndrome with only 200 reported cases and an estimated incidence of 1 in 100,000 deliveries. It is a benign condition where most recover spontaneously but it is very important to have dangerous differential diagnoses in mind.
Keywords: Hamman’s syndrome; Subcutaneous emphysema; Primipara; Pneumomediastinum
Abbreviations: Hamman’s syndrome: HS
Introduction
Spontaneous pneumomediastinum was first described by Hamman in 1945 (Hamman’s syndrome) [1], but the first documented case appeared in 1618 when the queen of France was giving birth [2]. Since then, there have been reported 200 cases, with an estimated incidence of 1 in 100,000 deliveries [3-5]. Hamman’s syndrome (HS) is described as a rare benign condition presenting after giving birth, consisting of the following symptoms: chest pain, dyspnea, dysphagia, swelling and neck pain [3-5]. HS usually resolves spontaneously without serious consequences. It has been observed most often in Primipara with a long second stage of labor [3-5]. Cho., et al. showed that pushing, difficult labor, and use of inhalation drugs were independent risk factors in young Primiparas [3].
Case
We present a case of a fit 27-year-old woman primipara, non-smoker, admitted to the hospital in labor at 41 weeks´ gestation. She had no previous history of surgery, and took no medication. It had been a normal pregnancy with a 1st stage of labor without any complications. During the 2nd stage of labor she was actively pushing for one hour. Total bleeding was measured to 200 mL and a vaginal tear of 1st degree was observed. The birth weight was 3115g. Two hours postpartum, the woman developed bloodshot eyes and swelling of neck and cheeks. Six hours postpartum, the patient complained of chest pains, especially in deep inspiration. Finally, subcutaneous emphysema developed from around the mammae up to the cheekbones and with a nasal voice. No inhalation drugs were used during birth.
Investigations
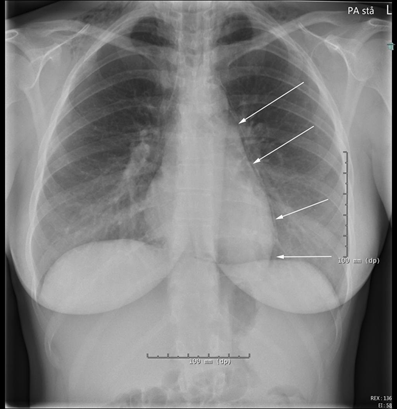
Blood pressure 2 hours postpartum was 105/74 with a heart rate of 105. Electrocardiogram and blood samples were normal, while x-ray showed pneumomediastinum left and distal to the heart and extending up in the mediastinum with bilateral subcutaneous emphysema (Image A and B).
Blood pressure 2 hours postpartum was 105/74 with a heart rate of 105. Electrocardiogram and blood samples were normal, while x-ray showed pneumomediastinum left and distal to the heart and extending up in the mediastinum with bilateral subcutaneous emphysema (Image A and B).
Figure 1A: Frontal x-ray. Arrows indicate pneumomediastinum left and distal to the
heart and extending up in the mediastinum with bilateral subcutaneous emphysema.
Outcome and follow up
The patient received no treatment, but spontaneously recovered after 24 hours postpartum. There was no further development in the Pneumomediastinum and the patient remained stable. The only symptoms that remained were chest pain during full inspiration. The subcutaneous emphysema slowly regressed, and the patient was discharged 3 days later.
The patient received no treatment, but spontaneously recovered after 24 hours postpartum. There was no further development in the Pneumomediastinum and the patient remained stable. The only symptoms that remained were chest pain during full inspiration. The subcutaneous emphysema slowly regressed, and the patient was discharged 3 days later.
Differential diagnosis
During acute illness after giving birth, there are numbers of diagnoses in which the clinical symptoms are much alike, and must be considered when the diagnostic approach is planned. Chest pains postpartum can be a result of amniotic embolism, pulmonary embolism, myocardial infarction, pneumothorax, aortic dissection, rupture of the esophageal rupture, also known as Boer haven’s syndrome (extremely rare during labor, especially without a preceding history of vomiting [6], interstitial emphysema, pneumothorax, pneumopericardium, toxic effect of injected drugs, cardiac tamponade or mediastinitis. Most of these differential diagnoses can be ruled out by a CT-Thorax and arterial blood gas analysis, but still, the single most important diagnostic test is chest x-ray [3-5].
During acute illness after giving birth, there are numbers of diagnoses in which the clinical symptoms are much alike, and must be considered when the diagnostic approach is planned. Chest pains postpartum can be a result of amniotic embolism, pulmonary embolism, myocardial infarction, pneumothorax, aortic dissection, rupture of the esophageal rupture, also known as Boer haven’s syndrome (extremely rare during labor, especially without a preceding history of vomiting [6], interstitial emphysema, pneumothorax, pneumopericardium, toxic effect of injected drugs, cardiac tamponade or mediastinitis. Most of these differential diagnoses can be ruled out by a CT-Thorax and arterial blood gas analysis, but still, the single most important diagnostic test is chest x-ray [3-5].
Discussion
Spontaneous pneumomediastinum and subcutaneous emphysema is a benign condition that in most cases regresses without further intervention within days. It is most likely due to a rupture of pulmonary alveoli due to a forceful Valsalva maneuver during 2nd stage of labor. The Valsalva results in a high intra-alveolar pressure and over-inflations of the lungs. Bubbles of interstitial air then dissect along the vascular sheaths and connective tissue planes to the mediastinum.
Ruptured peripheral alveoli can also be provoked by forceful coughing associated with asthmatic bronchospasm, chest infection and illicit inhalational drug use. It is important to take differential diagnosis into consideration. Recurrence is thought to be low, and there is no evidence to support follow-up in later pregnancies. Epidural analgesia has been suggested at future deliveries to prevent active pushing, and avoidance of nitrous oxide, as it can increase the intra-alveolar pressure [3].
Conflict of interest
No financial interest or any conflict of interest exists.
No financial interest or any conflict of interest exists.
References
- Hamman LV. “Mediastinum emphysema”. JAMA 128 (1945): 1.
- Gordon CA. “Respiratory emphysema in labor”. American Journal of Obstetrics & Gynecology 14.5 (1927): 633–646.
- Cho C., et al. “Spontaneous pneumomediastinum (Hamman's syndrome): a rare cause of postpartum chest pain”. BMJ Case Reports (2015):
- Kouki S and Fares AA. “Postpartum spontaneous pneumomediastinum 'Hamman's syndrome'”. BMJ Case Reports (2013):
- Mahboob A and Eckford SD. “Hamman's syndrome: an atypical cause of postpartum chest pain”. Journal of Obstetrics and Gynaecology 28.6 (2008): 652-653.
- Wozniak DR and Blackburn A. “Postpartum pneumomediastinum manifested by surgical emphysema. Should we always worry about underlying oesophageal rupture?” BMJ Case Reports (2011):
Citation:
Laerke Kamstrup Moser and Mohammed Rohi Khalil. “Spontaneous Pneumomediastinum and Subcutaneous Emphysema
Postpartum in Primipara”. Gynaecology and Perinatology 1.2 (2017): 111-114.
Copyright: © 2017 Laerke Kamstrup Moser and Mohammed Rohi Khalil. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.