Research Article
Volume 2 Issue 3 - 2018
Epidemiology of Neonatal Sepsis in Pediatric Department of Hadramout University Hospital, Mukalla, 2015
1Professor of community medicine, Hadramout University College of Medicine (HUCOM)
2A group of 4th medical student, Hadramout University College of Medicine (HUCOM), 2015/2016
2A group of 4th medical student, Hadramout University College of Medicine (HUCOM), 2015/2016
*Corresponding Author: Abdulla Salem Bin Ghouth, Hadramout University College of Medicine (HUCOM), Department of Community
Medicine, Fluk, Mukalla, Hadramout, Yemen.
Received: May 24, 2018; Published: August 07, 2018
Abstract
Background: Neonatal sepsis is a clinical syndrome characterized by systemic signs of infection. Sepsis occurring in the first 7 days of life is defined as early-onset sepsis (EOS) and that occurring beyond 8-28 days of neonate age as late-onset sepsis (LOS). This study was done to determine the clinical epidemiology of neonatal sepsis among neonates admitted to the Pediatric Department of Hadramout University Hospital in Al-Mukalla during the year 2015.
Methods: The study was a retrospective descriptive study relied through medical records in the Pediatric Department of University Hospital in Al-Mukalla, all neonatal sepsis cases registered during Year 2015.
Findings: The incidence rate of Neonatal Sepsis in the Hadramout University Hospital in 2015 was 12.8%; male neonate are more exposed than females (64.5%) having early neonatal sepsis (73%) and coming from urban areas of Mukalla (65%). Although numbers of neonates (54.8%) were born in hospital and developed sepsis compared to the neonates born at home but the difference is not significant. The most common antibiotics prescribed by pediatricians in the hospital were single antibiotic (53.8%) and the frequently prescribed single antibiotic was ampicillin (46%) followed by mixed antibiotics prescribed (46.2%) and mostly in the form of ampicillin with cefotaxime (53.49).
Conclusion: Early neonatal sepsis is the common period of the disease with male neonates more effected than females. The neonatal sepsis occurred despite the place of and/or type delivery raising the questions about the contributing factors to neonatal sepsis.
Keywords: Neonate; Sepsis; Mukalla
Introduction
Sepsis is the commonest cause of neonatal mortality (death in the first 28 days of life); it is responsible for about 30-50% of the total neonatal deaths in developing countries. It is estimated that up to 20% of neonates develop sepsis and approximately 1% die of sepsis related causes. Sepsis related mortality is largely preventable with prevention of sepsis itself, timely recognition, rational antimicrobial therapy and aggressive supportive care [1,2].
The incidence of neonatal sepsis depends on geographic area and may vary from country to country as well as within the same country. In developing countries, neonatal mortality resulting from all cases of neonatal sepsis is about 34 per 1000 live births, occurring mainly in the first week of life, whilst it is 5 per 1000 live births in developed countries [3]. Neonatal sepsis is defined as a clinical syndrome in an infant 28 days of life or younger, manifested by systemic signs of infection and isolation of a bacterial pathogen from the bloodstream [4].
Neonatal sepsis can be classified into two major categories terms early-onset infection and late-onset infection. The terms early-onset infection and late-onset infection refer to the different ages at onset of infection in the neonatal period. These disorders were originally divided arbitrarily into infections occurring before and after 1 week of life. It is more useful to separate early- and late-onset infections according to peripartum pathogens. Early-onset infections are acquired before or during delivery (vertical mother-to-child transmission). Late-onset infections develop after delivery from organisms acquired in the hospital or the community. The age at onset depends on the timing of exposure and virulence of the infecting organism [5]. The organisms associated with neonatal infection vary significantly in different geographical areas.
Group B streptococcus (GBS) continues to be the most important bacterial pathogen associated with early-onset sepsis in many developed countries, for reasons which remain unclear, neonates in some developing nations are rarely infected with GBS, which only accounts for 14% of neonatal infection. Neonatal infections in the developing nations are dominated by Gram-negative (e.g. Klebsiella species) and Gram-positive organisms (e.g. Staphylococcus aureus). It is therefore essential that antibiotic therapy be tailored to the specific microbial needs of a particular geographical region [6]. The risk factors of neonatal sepsis include the following: Prematurity, low birth weight, rupture of membrane (ROM) ≥ 18 hours , maternal puerperal fever or infection, resuscitation and male sex [7]. The earliest signs of sepsis are often subtle and nonspecific; indeed, a high index of suspicion is needed for early diagnosis.
Neonates with sepsis may present with one or more of the following symptoms and signs:
- Hypothermia or fever (former is more common in preterm low birth weight infants)
- Lethargy, poor cry, refusal to suck
- Poor perfusion, prolonged capillary refill time
- Hypotonia, absent neonatal reflexes
- Brady/tachycardia
- Respiratory distress, apnea and gasping respiration
- Hypo/hyperglycemia
- Metabolic acidosis.
Specific features related to various systems: Central nervous system (CNS): Bulging anterior fontanelle, high-pitched cry, excess irritability, stupor/coma, seizures, neck retraction. Presence of these features should raise a clinical suspicion of meningitis. Cardiac: Hypotension, poor perfusion, shock. Gastrointestinal: Feed intolerance, vomiting, diarrhea, abdominal distension, paralytic ileus, necrotizing enterocolitis (NEC). Hepatic: Hepatomegaly, direct hyperbilirubinemia (especially with urinary tract infections). Renal: Acute renal failure. Hematological: Bleeding, petechiae, purpura. Skin changes: Multiple pustules, abscess, sclerema, mottling, umbilical redness and discharge [8,9].
The typical complete sepsis workup in a neonate consists of obtaining complete white blood cell count with differential, single blood culture, urine culture, and lumber puncture for cell count and culture. In addition, there may a role for culture and gram staining of tracheal aspirates from intubated neonates shortly after breath. Acute phase reactants are also frequently used in predicting neonatal sepsis. The most widely used is C - reactive protein, which has a high degree of sensitivity for neonatal sepsis [10].
Clinical diagnosis of presentation is difficult due to nonspecific signs and symptoms. In addition laboratory diagnosis is time consuming. This matter necessitates the initiation of empirical antibiotic therapy till the suspected sepsis is ruled out. Empirical antibiotic therapy should be unit-specific and determined by the prevalent spectrum of etiological agents and their antibiotic sensitivity pattern. The most commonly used antibiotics include penicillin or ampicillin, cefotaxime, ciprofloxacin, gentamicin and amikacin [11,12].
Knowledge of local and regional health problems is a prerequisite for establishing an effective health care delivery system, epidemiological and statistical information regarding neonatal sepsis is the basis for establishing a sound intervention [13]. This information also has significant influence on treatment assessment and subsequent outcome. Therefore the study is designed to describe the clinical epidemiology of neonatal sepsis at Hadramout University hospital in Mukalla, Yemen, during a 12 month period from 1st January to 31st December 2015, and specifically through determining: a) the incidence of neonatal sepsis among cases admitted to university hospital b) the most common clinical presentation of neonatal sepsis as well as c) identifying the commonly prescribed anti-microbial drugs for treatment of neonatal sepsis in Hadramout University hospital.
Materials and Methods
Study design: This study was retrospective descriptive study carried out by a group of fourth year medical students of Hadhramout University in a period between January 1st 2015 to December 31st 2015.
The setting: The study was conducted among neonates in Hadramout University Hospital in Al Mukalla district the capital of Hadhramout governorate which located in Arabian Sea in Yemen.
Study population: Study population was all neonates with neonatal sepsis who admitted for treatment in Hadramout University hospital during the period from January 1st 2015 to December 31st 2015.
Data collection tool: The data was collected through medical records and the only tool was used was the check list.
This includes:Personal data: (sex - age - area- date of admission-date of discharge-Hospitalization period -site of admission). The most common risk factors related to neonatal sepsis: (gestational age, birth weight, mode of delivery, and risk factors for sepsis: premature rupture of membranes (PROM), maternal with fever and Urinary Tract Infection UIT). The most common clinical picture of neonatal sepsis: (poor reflexes, lethargy, respiratory distress, bradycardia, apnea, convulsions, abdominal distension, and diarrhea). The most common antimicrobial therapy prescribed to neonatal sepsis. The prognosis of discharge.
Data Analysis:The data was checked for completeness, coded then was entered in to the computer and was analyzed by using statistical package for social science (SPSS V 20). The obtained data were analyzed using descriptive statistical tables (frequencies percentages). Data was presented in tables and graphs by using computer applications Microsoft office word and Microsoft excel.
Ethical Consideration: Approval of project was obtained from Hadhramout University College of medicine (HUCOM) department of community medicine. We ensure that the information which will be involved in the study will be used for the benefits of the community.
Results
This study is conducted in the pediatric department of the Hadramout University hospital in Mukalla city where there are 252 admitted neonates out of the total 1975 admitted children in the hospital during the study period giving the proportion of neonatal admissions among the total pediatric admission in the hospital to 12.8%. The study focused on the cases of neonatal sepsis; out of the admitted 252 neonates there were 93 neonates diagnosed clinically as having neonatal sepsis that means the proportion of neonatal sepsis among all admitted neonates in the University hospital of Mukalla was 37%. Most of the neonatal sepsis cases were males (64.5%) having early neonatal sepsis (73%) and coming from urban areas of Mukalla (65%) (Table1).
| Characteristics | No of Neonates | % |
| Sex | ||
| Male | 60 | 64.5% |
| Female | 33 | 35.5% |
| Total | 100 | 100% |
| Residence | ||
| Urban | 61 | 65.6% |
| Rural | 32 | 34.4% |
| Total | 93 | 100% |
| Gestational age at birth | ||
| Full term | 78 | 83.9% |
| Preterm | 15 | 16.1% |
| - Total | 93 | 100% |
| Birth weight | ||
| Low birth weight | 34 | 36.6% |
| Norma birth weight | 59 | 63.4% |
| Total | 93 | 100% |
| Place of birth Home | 42 | 45.2% |
| Hospital | 51 | 54.8% |
| Total | 93 | 100% |
| Word ICU | 31 | 31.3% |
| Pediatric | 62 | 68.7% |
| Total | 93 | 100% |
| Age at onset of sepsis | ||
| Early | 68 | 73% |
| Late | 25 | 27% |
| Total | 93 | 100% |
Table 1: Description of the studied neonates with neonatal sepsis, University Hospital, Mukalla, 2016.
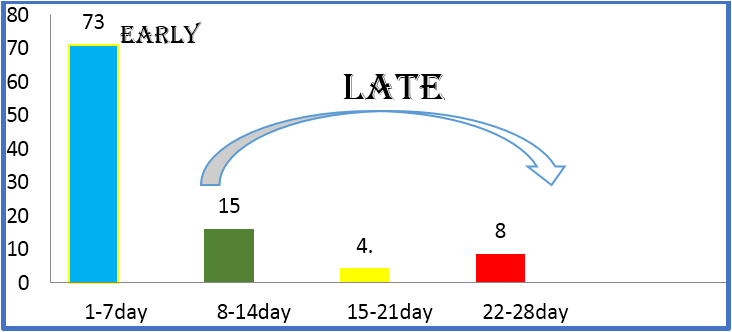
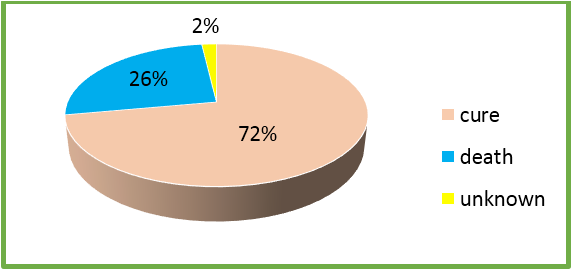
The study showed that, most common clinical manifestations suggestive of sepsis were fever (57%), Poor of feeding (57%), difficulty of breathing (29%), jaundice (22.6%), cyanosis (12.6%), hypotonia (20%), diarrhea and Abnormal movement (Table2). Neonatal sepsis is classified by the age at onset of sepsis into two categories: early onset disease (EOD) and late onset disease (LOD). The EOD is the onset of neonatal sepsis during the first 7 days of life, The LOD is the onset of neonatal sepsis during the period of 8-28 days of neonate age. EOD in this study represented in 71% of the studied neonates while LOD is present in 29% of them (Figure1). Case fatality rate due to neonatal sepsis is high in Hadramout University hospital (26%), (Figure 2) with significant difference according to the period of onset of sepsis (P-value < 0.05) (Table 4).
| Clinical signs/accompanied diagnoses | No.% |
| Fever | 53 57 |
| Vomiting | 7 7.5 |
| Poor of feeding | 53 57 |
| Difficulty of breathing | 27 29 |
| Jaundice | 21 22.6 |
| Cyanosis | 12 12.9 |
| Abnormal movement | 13 14 |
| Hypotonia | 19 20 |
| Diarrhea | 6 6.5 |
| bulging of anterior fontanel | 8 8.5 |
| Other* | 26 28 |
Table 2: Clinical manifestations reported in the total 93 neonates diagnosed clinically as having neonatal sepsis, The University Hospital, Mukalla 2016.
Figure 2: Prognosis of neonatal sepsis among neonates
admitted to Hadramout University Hospital, 2015.
Regarding management of neonatal sepsis in University hospital of Mukalla; the most commonly antibiotics prescribed by pediatricians in the hospital were single antibiotic (50/93, 53.8%) and the frequently prescribed single antibiotic was ampicillin (23/50, 46%) and it found that it is effective. In the case of mixed antibiotics prescribed (43, 46.2%); and mostly in the form of ampicillin with cefotaxime (23/43, 53.49%). Other antibiotics prescribed were: Amikacin, cefotaxime, Cefuroxime and Vancomycin. (Table 3). In this study; we are able to describe the relation of certain neonatal and maternal characteristics on the age at onset of neonatal sepsis but unfortunately no statistical association were exist (Tables 4 & 5).
| Antibiotic | No of neonates | % |
| Ampicillin | 53 | 57% |
| Amikacin | 20 | 21.5% |
| Cefotaxime | 53 | 57% |
| Cefuroxime | 4 | 4.3% |
| Vancomycin | 12 | 12.9% |
Table 3: Types and Frequency of antibiotics prescribed for treatment of neonatal sepsis either as a single or mixed, The University hospital of Mukalla 2016.
| Characteristics | Early neonatal sepsis n=68 (%) |
Late neonatal sepsis n=25 (%) |
Total N=93 |
P-value* |
| Sex | ||||
| - Male | 42 (70%) | 18 (30% | 60 | 0.4 |
| - Female | 26 (78.9%) | 7 (21.1%) | 33 | |
| Residence | ||||
| - Urban | 47 (77%) | 14 (23%) | 61 | 0.2 |
| - Rural | 21 (65.6%) | 11 (34.4%) | 32 | |
| Place of delivery | ||||
| - Home | 28 (66.6%) | 14 (33.4%) | 42 | 0.2 |
| - Hospital | 40 (78.4%) | 11 (21.6%) | 51 | |
| Mode of delivery | ||||
| - Vaginal | 59 (70.2%) | 25 (29.8%) | 84 | 0.1 |
| - LSCS | 9 (100%) | 0 (0%) | 9 | |
| Gestational age at birth | ||||
| - Full-term | 56 (71.8%) | 22 (28.2%) | 78 | 0.5 |
| -Preterm | 12 (80%) | 3 (20%) | 15 | |
| Birth weight | ||||
| - Low birth weight | 27 (79.4%) | 7 (20.6%) | 34 | 0.3 |
| - Normal birth weight | 41 (69.5%) | 18 (30.5%) | 59 | |
| Days of hospital stay | ||||
| 1-7days | 53 (71.6%) | 18 (28.4%) | 74 | 0.7 |
| 8-14 days | 11 (64.7%) | 6 (35.3%) | 17 | |
| 15-21 days | 4 (80%) | 1 (20%) | 5 | |
| Neo (n = 68) † natal outcome | ||||
| - Cured | 34 (68%) | 16 (32%) | 50 | 0.03‡ |
| - Died | 17 (94.4%) | 1 (5.6%) | 18 |
*chi square test was used with 0.05 significance level‡ Fischer exact test is used
†15 cases not included in this analysis because no data documented about the outcome of treatment
Table 4: Relationship between age at onset of the neonatal sepsis and certain neonatal characteristics, University Hospital, Mukalla, 2015.
†15 cases not included in this analysis because no data documented about the outcome of treatment
Table 4: Relationship between age at onset of the neonatal sepsis and certain neonatal characteristics, University Hospital, Mukalla, 2015.
| Maternal factors | Early neonatal sepsis N = 68 (%) |
Late neonatal sepsis N = 25 (%) |
Total N = 93 |
P-value* |
| Place of delivery | ||||
| - Home | 28 (66.6%) | 14 (33.4%) | 42 | 0.2 |
| - Hospital | 40 (78.4%) | 11 (21.6%) | 51 | |
| Mode of delivery | ||||
| - Vaginal | 59 (70.2%) | 25 (29.8%) | 84 | 0.1 |
| - LSCS | 9 (100%) | 0 (0%) | 9 | |
| Premature rupture membrane | ||||
| - Yes | 3 (75%) | 1 (25%) | 4 | 0.9 |
| - No | 65 (73%) | 24 (27%) | 89 | |
| Maternal peurperuium fever or infection | ||||
| -Yes | 18 (78.3%) | 5 (21.7%) | 23 | 0.5 |
| -No | 50 (71.4%) | 20 (28.6%) | 70 |
*chi square test was used with 0.05 significance level
Table 5: Relationship between age at onset of the neonatal sepsis and certain maternal factors, University Hospital, Mukalla, 2015.
Table 5: Relationship between age at onset of the neonatal sepsis and certain maternal factors, University Hospital, Mukalla, 2015.
Sepsis remains one of the most important causes of morbidity and mortality in the newborn. The results of this study showed that the incidence of neonatal sepsis among neonates in the University hospital of Mukalla in 2015 was 37%. This figure is higher than that were reported from Nebal (12.4%) [14] and India (7.6%) [15]. The difference here due to that the diagnosis in Hadramout University hospital is based on clinical diagnosis that may overestimate the true incidence. Eman., et al. (2015) reported a high incidence of neonatal sepsis in three hospitals in Egypt [16], the study focused on admitted neonates in intensive care units in which most of the cases were critically ill and with high probability of sepsis than those admitted to other the general pediatric department as the case of our study.
The disease occurred mostly in the early neonate (EOS) which constitutes 73% of cases while 27% of the disease occurred in the late neonate (LOS). The result indicated that the incidence of EOS septicemia was more common than LOS which is consistent with other reports from Nepal, Iran, Iraq, Bangladesh, and Yemen [14].This result in contrast with study of Egypt where 44% of neonatal sepsis occurred in the early period while most of cases (56%) occurred in the late neonate (LOS) [16].
The result of this study showed that most clinical presentations of neonatal sepsis are fever (57%), poor feeding (57%). Difficulty of breathing (29%), and jaundice (22%) which is consistent with other studies; a study in Sudan showed that the most common clinical pictures were fever (63%), Difficulty of breathing (44%), poor feeding (32.5%), jaundice (31%) [17] While in a study conducted in Sanaa (Yemen) showed that the most common clinical pictures were difficulty of breathing (72.2%), jaundice (62.2%), cyanosis (51.1%), and lethargy (47.8%) [18]. Similar findings were reported in India; lethargy (77.4%), hypothermia (47.5%) and respiratory distress (44%) [19].
This study focused on some neonatal, maternal factors that may precipitate the development of neonatal sepsis like place of delivery, gestational age at birth , birth weight and premature rapture of membrane and maternal fever, unfortunately no association being exist between any of these factors and the neonatal sepsis while a study in south Eastern Mexico at 2012, [20] revealed that, prematurity, premature rupture of membrane and low birth weight are significant contributing factors to the neonatal sepsis. Failure to confirm any association in this study due difference in study designs since this is limited to one year period.
Antibiotic prescription for neonatal sepsis is not based on antimicrobial sensitivity tests. The most prescribed antibiotics are Ampicillin, Cefotaxime and Amikacin in contrast with study conducted in Nepal where the prescriptions are laboratory based with the most pathogens in neonatal sepsis are staphylococcus aureus, Klebsiella, psudoomonas aerogiosa, All the pathogens were sensitive to amikacin and highly resistance to ampicillin. [21] This discrepancy raising the concern about clinical diagnosis and the need for laboratory based management in Hadramout University hospital.
Regarding the outcome of the neonatal sepsis our study show that the case fatality rate of neonatal sepsis was high (26%) with statistically significant difference between early- and late-onset sepsis. In consistence to study that done in southeastern Mexico, which show a marked difference in between early- and late-onset sepsis, as well as case fatality rates are in Mexico (9.5%) [20].
Limitation of the study:This study collected data from hospital archive that were not completely filed because the specialists not requires the blood culture this issue limited our study only on the clinical diagnosis.
Conclusions
Early neonatal sepsis is the common period of the disease with male neonates more effected than females. The Neonatal sepsis occurred despite the place of or type delivery raising the questions about the contributing factors to neonatal sepsis. Neonates with sepsis in early period are prone to risk of death more than those developing sepsis in the late period.
Recommendations
- We recommend the hospital administration to improve the process of data compilation and archiving.
- Antimicrobial culture and sensitivity test must be performed to develop an evidence based practice for management of neonatal sepsis in the University hospital.
References
- Bang AT., et al. “Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India”. Lancet 354.9194 (1999):1955-1961.
- Stoll BJ. “The global impact of neonatal infection”. Clinics in Perinatology 24.1(1997): 1-21.
- Edwards M. S. and Baker C. J. Sepsis in the newborn. In:A. A. Gershon, P. J. Hotez, and S. L. Katz Krugman's. Infectious Diseases of Children, Eds, Mosby, Philadelphia, Pa, USA. (2004): 545.
- Patel S J and Saiman L. “Antibiotic resistance in neonatal intensive care unit pathogens: mechanisms, clinical impact, and prevention including antibiotic stewardship”. Clinics in Perinatology 37.3 (2010): 547–563.
- Klinger G., et al. “Epidemiology and risk factors for early onset sepsis among very-low-birth weight infants”. American Journal of Obstetrics & Gynecology 201.1(2009): 38.e1-6.
- Van den Hoogen A., et al. “Long-term trends in the epidemiology of neonatal sepsis and antibiotic susceptibility of causative agents”. Neonatology 97.1 (2010): 22-28.
- Deorari Ashok K. For the Investigators of the National Neonatal Perinatal Database (NNPD). Changing pattern of bacteriologic profile in Neonatal Sepsis among intramural babies. Journal of Neonatology 20 (2006): 8-15.
- Lin FY., et al. “Assessment of Intrapartum Antibiotic Prophylaxis for the Prevention of Early-onset Group B Streptococcal Disease”. The Pediatric Infectious Disease Journal 30.9 (2011): 759-763.
- Bizzarro MJ., et al. “Seventy-five years of neonatal sepsis at Yale: 1928-2003”. Pediatrics 116.3 (2005): 595–602.
- Haque KN., et al. “Pattern of culture-proven neonatal sepsis in a district general hospital in the United Kingdom”. Infection Control & Hospital Epidemiology 25.9 (2004): 759−764.
- Singh M., et al. “Predictive perinatal score in the diagnosis of neonatal sepsis”. Journal of Tropical Pediatrics 40.6 (1994): 365-368.
- Takkar VP., et al. “Scoring system for prediction of early neonatal infections”. Indian Pediatrics 11 (1974): 597-600.
- Anah MV., et al. “Neonatalsepticaemia in Calabar Nigeria”. Tropical Doctor 38 (2008): 126-128.
- Ansari S., et al. “Neonatal Septicemia in Nepal: Early-Onset versus Late-Onset”. International Journal of Pediatrics. 2015 (2015).
- Verma., et al. “Neonatal sepsis: Epidemiology, clinical spectrum, recent antimicrobial agents and their antibiotic susceptibility pattern”. International Journal of Contemporary Pediatrics 2.3(2015): 176-180.
- Eman M. RabieShehab El-Din., et al. “Epidemiology of Neonatal Sepsis and Implicated Pathogens: A Study from Egypt”. BioMed Research International (2015): 1-11.
- Magzoub O., et al. “Clinical presentation of neonatal sepsis”. Journal of Medicine and Clinical Science 4.4 (2015): 116-120.
- Al-Shamahy H., et al. “Types of Bacteria associated with Neonatal Sepsis in Al-Thawra University Hospital, Sana’a, Yemen, and their Antimicrobial Profile”. Clinical &Basic Research 12.1 (2012): 48-54.
- Jajoo M., et al. “To Study the Incidence and Risk Factors of Early Onset Neonatal Sepsis in an Out born Neonatal Intensive Care Unit of India”. The journal of Clinical Neonatology 4.2 (2015): 91-95.
- Leal Y., et al. “Risk factors and prognosis for neonatal sepsis in southeastern Mexico: analysis of a four-year historic cohort follow-up”. BMC Pregnancy and Childbirth (2012)
- Shrestha R., et al. “Bacteriological study of neonatal sepsis and antibiotic susceptibility pattern of isolates in Kathmandu, Nepal”. Nepal Medical College Journal 15.1 (2013): 71-73.
Citation:
Abdulla Salem Bin Ghouth., et al. “Epidemiology of Neonatal Sepsis in Pediatric Department of Hadramout University Hospital,
Mukalla, 2015”. Gynaecology and Perinatology 2.3 (2018): 285-293.
Copyright: © 2018 Abdulla Salem Bin Ghouth., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.