Review Article
Volume 2 Issue 3 - 2018
Phytomedicines: far Beyond Cytotoxicity in Cancer therapy. Sole Multitarget-Polypharmacology, Chemopreventive and Safety Profiles: Combinatorial Synergy, Chemosensitization and Mitigation of Chemotherapy Adverse-Reactions.
PhD, Mansoura University, Egypt & The Medical College of Georgia, Augusta, USA- Clinical Biochemist, Eg. MOH, Egypt
*Corresponding Author: Abdalla M El-Mowafy, PhD, Mansoura University, Egypt & The Medical College of Georgia, Augusta, USA- Clinical Biochemist, Eg. MOH, Egypt.
Received: December 26, 2017; Published: January 09, 2018
Abstract
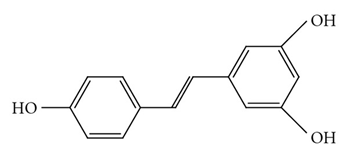
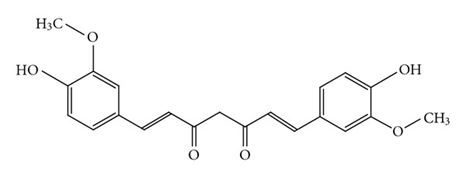
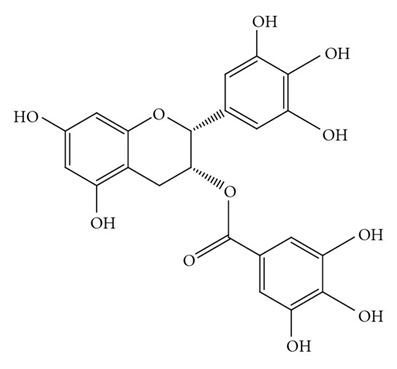
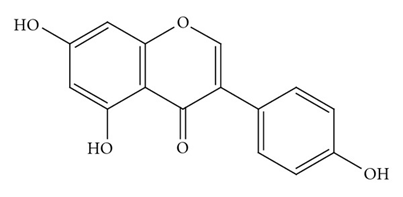
Phytomedicines (PMs) are bioactive phytochemicals with established health benefits. Because of their unique structure, they can bind to and modulate the activity of cellular bioactive proteins, thereby conferring numerous, mostly favorable, pharmacological effects; including anti-inflammatory, antioxidative, antidiabetic, immunostimulant, and cellular protective effects. Such multitarget-“polypharmacology”, along with well-tolerability of PMs, prompted their use as sole and/or combinatorial drugs for management of “complex” and refractory “drug-resistant” diseases like cancer. Common PMs include curcumin, resveratrol, EGCG, genistein, gingerol, quercetin, lycopene, and baicalein.
Unlike chemotherapeutic drugs, PMs have been a mainstay in protection against cancer (chemoprevention) by interfering with all 3-stages of carcinogenesis; namely: initiation, promotion, or progression. They also enhance host’s immune response against eruption of carcinogenesis. When concurrently used with chemotherapy, they are intended to accentuate their cytotoxic effects (synergy), reduce their doses, minimize their noxious adverse-reactions or overcome resistance to their anticancer effects (chemoresistance). Thus, chemosensitization by PMs is meant to abate, bypass, or silence the molecular machinery underlying chemoresistance, which include drug-transporters, cell cycle effectors, signaling cascades and nuclear transcription factors. In this vein, all cellular and molecular rationale and underpinnings are described and their therapeutic relevance is highlighted. The advanced recent technology (as with Omics and Nanotechnology), has helped improve PM-kinetic profiles, bioavailability, and rationalized their therapeutic utility and networking. Therefore, PMs are now gaining more ground from the bench-side to the clinic”.
Keywords: Cancer treatment; Phytomedicine; Polypharmacology; Chemotherapy; Drug Safety; Chemoprevention; Synergistic combinations; Resistance to chemotherapy; Adverse drug reactions; Chemosensitization
Introduction
Phytomedicines (PMs) are bioactive phytochemicals (of plant origin) with established profiles of beneficial health effects, pharmacological activity, and recognized safety spectrum [1,2]. Many such chemicals have been sold originally for nutritional and supplemental OTC use; thereby also belonging to the broader-term “nutraceuticals”. PMs often have such a unique chemical structures with many key functional groups (e.g polyphenols, thiol-compounds) that mimic (and complement) those of the mammalian cell aminoacids, thereby permitting them to easily bind to cellular bioactive-proteins, such as enzymes, adaptors and receptors and modulate their activity [3,4]. Not surprisingly, PMs turned out to exhibit a broad-range of, mostly favorable, pharmacological activities including anti-inflammatory, antioxidative, antidiabetic, and cellular protective effects. Such multifaceted pharmacological effects, along with well-tolerability, spur their application as sole and/or adjunct drugs for management of diseases, especially the “complex” and “refractory” ones like cancer, heart-disease, and neurological diseases, which often mandate the use of multiple-drug regimens, rather than monotherapy, to accentuate the therapeutic efficacy and clinical outcomes [5]. With the advent of recent Omics and nanotechnology studies, existing obstacles against comprehensive clinical use of some PMs, such as limited bioavailability and absorption, have been reasonably defused [6].
Cancer, after cardiovascular disease (CVD), ranks as the second leading cause of death allover the globe. However, unlike CVD, cancer management poses more challenging, cumbersome and grieving aspects of throughout its therapy. Thus, conventional chemotherapies evoke widespread and life-threatening systemic toxicity and adverse reactions, which have mandated prohibition of their long-term use. Furthermore, resistance to chemotherapy, tumor recurrence and remote-invasion (metastasis) are coherent criteria that entail vicious and pain-stacking sequelae to cancer [7,8]. Therefore, there has been a tremendous and persisting need to identify superior anticancer therapies that can be either preventive, or rather more specific and safer than chemotherapy. In developing countries, approximately 35% of the prescribed drugs are derived from natural products, and over 60% of the anticancer drugs in clinical use originated from natural products [9-11], including plants, marine organisms, and microbes. Many investigations are being carried out worldwide to discover naturally occurring compounds that can suppress or prevent the progress of carcinogenesis, or alternatively improve their quality and efficacy against cancer, and limit their adverse reactions. Whereas some natural compounds displayed superior cytotoxic effects but limited molecular targets and safety/specificity (like vinblastine and taxel), others (PMs) showed rather multitarget molecular effects and bigger safety profiles, as demonstrated by “polypharmacology” studies.
1. Polypharmacology of PMs: Molecular-multitargeting and its significance
Cancer is a complex, devastating disease that erupts and thrives via disruption of host cellular and biological targets, thereby mandating meticulous and extensive therapeutic manipulations [12,13]. Accordingly, finding drugs that act in multiple pathways, or electing a promising drug-combination represents a major challenge, because signaling networks of human cells are often inconsistently altered in different cancers [14]. Tumors frequently develop resistance to single-target drugs, as mutations in that target protein may easily render the tumor refractory to cytotoxicity of this drug.
Cancer is a complex, devastating disease that erupts and thrives via disruption of host cellular and biological targets, thereby mandating meticulous and extensive therapeutic manipulations [12,13]. Accordingly, finding drugs that act in multiple pathways, or electing a promising drug-combination represents a major challenge, because signaling networks of human cells are often inconsistently altered in different cancers [14]. Tumors frequently develop resistance to single-target drugs, as mutations in that target protein may easily render the tumor refractory to cytotoxicity of this drug.
In treating such complex systemic diseases, as with cancer, single-target drugs (as with chemotherapy) were documented to be inferior to “the versatile multiple-target regimens” that will likely evoke maximal efficacy and minimal toxicity [15-18]. As a result, a new concept is emerging that is designated “polypharmacology”, which focuses on drugs attacking multiple instead of single targets to maximally restore disease-associated pathways to a near-physiologic pace and manner [19,20]. This approach ultimately offers the potential for higher efficacy and may limit drawbacks generally arising from the chemotherapy multiple drugs, such as tumor resistance and adverse reactions.
By contrast, drugs addressing multiple targets are not compromised in their activity, if mutations in one of the targets appear. Most natural products exert their bioactivity by attacking multiple rather than single targets [21]. Not surprisingly, therefore, PMs invoke a variety of favorable responses with host cells, such as anti-inflammatory, antioxidative, antiproliferative, immunostimulant, cellular and neuroprotective effects.
At the cellular and molecular level, PMs can trigger a plethora of scenarios and events to invoke its beneficial effects. For instance: upon entering cells, these phytochemicals can directly capture free radicals and can also generate “chemical or electrophilic-stress signals” that recruit receptors/enzymes/adaptors related to various cellular signaling pathways. One such cascade is the activation of the nuclear factor erythroid-2 (NF-E2)-related factor-2 (Nrf2)-Kelch-like ECH associated protein 1 (Keap1) complex. Recruitment of the Nrf2-Keap1 complex induces many cellular defense mechanisms; including phase-II detoxifying enzymes, phase-III transporters, anti-oxidative stress proteins that protect normal cells from reactive oxygen and nitrogen species (RONS) and their serial-reactive metabolites of carcinogenic species [22,23].
By contrast, after cancer had developed, PMs (at tumor microenvironment) can abate oxidative stress, or additionally trigger pro-apoptotic and anti-proliferative effects, alter cell-cycle and growth-factor signaling, and perturb tumor gene transcription [24]. Among enzyme pathways that are downregulated in cancer cells by PMs are the mitotic/pro-inflammatory mitogen-activated protein kinase isoforms (MAPKs) and their downstream (dependent) signaling cascades. Likewise, Big mitogen-activated protein kinase-1 (BMK-1), also known as Erk5 has been shown to be activated various extracellular stimuli such as epidermal growth factor, IL-6, and hypoxia. As a member of MAPK family, BMK-1 has also been implicated in stress-cellular events coherent with cancer, like proliferation, migration, and apoptosis [25].
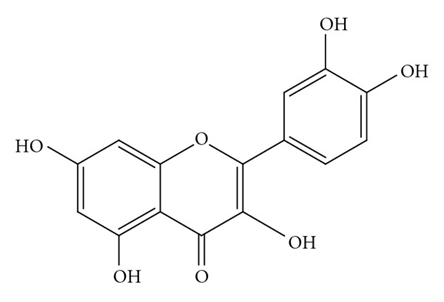
The signal transducer and activator of transcription-3 (STAT3) is a transcription factor constituent of the STAT family, known primary antecedents in carcinogenesis and cancer growth, whose activity was also proven to be regulated by numerous PMs. Thus, curcumin, resveratrol, cucurbitacin, flavopiridol, Epigallocatechin gallate (EGCG), and genistein (Figure 1) have demonstrated anticancer effects by inhibiting the growth of cancer cell through blocking of STAT3 activation [26-29].
Before neoplastic transformation (cancer cell development) occurs, the PM-driven cellular protective mechanisms unequivocally help in blocking the initiation of carcinogenesis and, therefore, contribute to “chemoprevention”, a concept that was originally pioneered and introduced by Wattenberg (1966) [30].
2. Chemoprevention by PMs: Significance and molecular mechanisms.
In virtue of constraints in early detection and effective treatment of cancer, preventive interventions have caught growing attention and accumulated paramount research efforts. Several such approaches and practice have shown promising outcomes in epidemiological and clinical trials allover the earth [31,32]. Chemoprevention is one of the strategies by which we can block or delay the malignant response to carcinogens or even prevent carcinogenesis via the use of natural (PMs) or synthetic chemical agents.
In virtue of constraints in early detection and effective treatment of cancer, preventive interventions have caught growing attention and accumulated paramount research efforts. Several such approaches and practice have shown promising outcomes in epidemiological and clinical trials allover the earth [31,32]. Chemoprevention is one of the strategies by which we can block or delay the malignant response to carcinogens or even prevent carcinogenesis via the use of natural (PMs) or synthetic chemical agents.
Exposure of normal cells to environmental carcinogens results in a series of genetic mutations. Induction of at least 1-2 mutations, in key-genes involved in cell-division such as proto-oncogenes and/or tumor suppressor genes, triggers tumor development. Activation of proto-oncogenes by qualitative or quantitative genetic changes results in promotion of proliferative/mitotic signals. An alternative scenario is when environmental carcinogen-mediated loss or attenuation of tumor suppressor genes leads to tumor development [33,34]. Genetic mutations, along with genomic instability and a series of epigenetic events, such as persistent inflammation or oxidative-stress, catalyze the transformation from normal- to malignant-cells. All transformed cells display common unusual criteria, such as prolonged proliferation, ever-lasting replication (immortality), resistance to cell death (apoptosis), and capacity to provoke new-vessel formation (angiogenesis) and translocation (invasion and metastasis) [35].
Cancer chemopreventive agents can reduce the incidence of tumorigenesis by interfering with stages of carcinogenesis; namely initiation, promotion, or progression. Many chemopreventive agents are derived from natural products, and phytochemicals (PMs) [36-38]. Natural edible products are nontoxic natural extracts or isolated individual-compounds (PMs) that, compared with synthetic chemotherapy, usually produce fewer untoward effects. Therefore, they potentially present a paramount target in achieving protection against cancer. Unlike chemotherapy, PMs also have a great deal of preference to influence rapidly-dividing cells than normal host cells [39].
Chemotherapeutic agents cannot be used for chemoprevention as they have a narrow-scoped molecular targeting and a broad-range of serious adverse reactions. Besides, they commonly lack reasonably lasting cytotoxic efficacy, specificity against tumors, and suffer resistance to its cytotoxicity in cancer patients. Conversely, PMs have remained as a precious edible and nutraceutical resource that bears fruitful prospects in the area of chemoprevention. Underpinnings are that PMs, on top of their potential safety, can exclusively enhance host’s immune response against carcinogenesis, and most importantly, they possess such a molecular versatility that mimics and complements mammalian cell components, thereby achieving polypharmacologic effects, consonant with efficacious multi-targeting chemoprevention. Commonly used PMs, which are widely marketed as nutraceuticals as well, include EGCG, curcumin, resveratrol, genistein, gingerol, quercetin, lycopene, and baicalein [40-41].
The molecular mechanisms whereby PMs trigger their chemopreventive effects involve changes in redox-potential, altering of enzyme activity, modulating signaling cascades and cell cycle rhythm as well as modification of transcription-factor activities and gene expression. Evidence for such profiles was mostly derived from cellular and animal model of cancer, because of the inability to reproduce the exposure/prevention conditions on human hosts, as well as lack/difficulty of learning about the mechanisms of action and toxicity in the living human beings [24].
Nevertheless, chemoprevention is mandated for individuals who are already at high risk to cancer, those with established primary tumors in order to prevent eruption of secondary tumors, or those who had been cured; for prevention of the recurrence of cancer. Thus recent efforts with clinical trials have targeted optimization of PM therapy and minimization of relevant caveats and concerns. Thus, to enhance absorption, bioavailability, or site-specific delivery and uptake of PMs, several approaches have been concertedly deployed. In this vein, nanotechnology and nano-medicine utilize minute-sized (nano) drugs via bridging the parent drug with specific carriers, polymers, proteins or lipids. Likewise, liposomes are intended for delivery of dietary PMs. Lastly, the use of PMs synthetic-analogs has been an immense realm of pharmaceutical research to improve dynamic and kinetic profiles of PMs [42-44].
3. Synergy of PMs with chemotherapy, and mitigation of its noxious adverse reactions (ADRs)
The word synergy is derived from the Greek words sunergia, which means ‘cooperation’, and sunergos, which means ‘working together’. PMs may well elicit sole cytotoxic effects on their own in cell- and animal-based cancer models. Such envisions have been promoted and become widely accepted, in clinical trials and Chinese-herbal-medicine, especially with PM-optimization via recent omics- and nanotechnology-based studies [2]. The complexity of cancer formation and development hinders effective cancer treatment using chemotherapy alone. Thence, seeking synergistic combinations of chemotherapeutic drugs and other drugs can be a promising way to enhance prognosis, quality of therapy and overall responsiveness to chemotherapy. Synergic combinations of chemotherapy with PMs or Chinese-herbal formulae that are known for anticancer potential are designed and intended for enhancing efficacy, reducing untoward/toxic effects, optimizing anti-tumor immune response, or minimizing cancer resistance to chemotherapy [45,46].
The word synergy is derived from the Greek words sunergia, which means ‘cooperation’, and sunergos, which means ‘working together’. PMs may well elicit sole cytotoxic effects on their own in cell- and animal-based cancer models. Such envisions have been promoted and become widely accepted, in clinical trials and Chinese-herbal-medicine, especially with PM-optimization via recent omics- and nanotechnology-based studies [2]. The complexity of cancer formation and development hinders effective cancer treatment using chemotherapy alone. Thence, seeking synergistic combinations of chemotherapeutic drugs and other drugs can be a promising way to enhance prognosis, quality of therapy and overall responsiveness to chemotherapy. Synergic combinations of chemotherapy with PMs or Chinese-herbal formulae that are known for anticancer potential are designed and intended for enhancing efficacy, reducing untoward/toxic effects, optimizing anti-tumor immune response, or minimizing cancer resistance to chemotherapy [45,46].
The principles of selecting drug combinations have been based on drugs acting on the same target but via different mechanisms, drugs acting on different cellular targets via the same mechanism; or drugs working on different molecules via different avenues. Numerous such combinations have been first attempted among Chinese herbs and PMs that were reported in cancer cells, and showed multifaceted promising outcomes. For instance, curcumin has been established as a multitargeting PM that displays anti-inflammatory, antioxidant and chemotherapeutic effects; while shows no or insignificant toxicity in animals, when used even at such elevated doses [47,48]. Furthermore, curcumin modulates the cellular levels of tumor suppressor genes, apoptotic genes, expression of oncogenes, and their respective effectors such as enzymes, receptors signal adaptors [49]. Thus, many Chinese herbs (or other PMs) have been combined with curcumin to seek synergy. When curcumin was used with triptolide, they promoted apoptosis in ovarian cancer cells, effects that were ascribed to deactivation of some heat-shock proteins; HSP27 and HSP70 [50]. In addition, the joint use of curcumin and emodin has substantially reduced growth and migratory/invasive ability of breast cancer cells [51]. On the other hand, resveratrol conferred synergy with the in vitro and in vivo cytotoxic effects of Curcumin in head and neck carcinomas [52].
On the other hand, the joint use of PMs can significantly augment the clinical antitumor effects of chemotherapeutic drugs. In this vein, a meta-analysis on some two thousands of patients showed that the efficiency of platinum-based chemotherapy was enhanced by intravenous infusion of the Chinese formula Shenqi fuzheng [53]. Another randomized and controlled clinical trial proved that the injection also raised the therapeutic effects of “cyclophosphamide, epirubicin and 5-fluorouracil regimen” in local-advanced breast cancer patients [54]. Likewise, an astragalus-based Chinese herb augmented the inhibitory effects of cisplatin in advanced non-small-cell lung cancer [55].
Another aspect is that adverse events, including nausea, vomiting, and anorexia, often develop as secondary/side effects to chemotherapy. Therefore, alleviating these untoward effects is such a worthy objective to improve the quality of chemotherapy. In this context, the concomitant use of astragalus-polysaccharide markedly concealed fatigue, nausea/vomiting, gastric-pain and loss of appetite linked with the application of the chemotherapeutic-drugs, vinorelbine and cisplatin, in patients with advanced NSCLC, thereby greatly enhance the acceptance of therapy and improving patients’ quality of life [56]. Quercetin, crocin and resveratrol were found to effectively lessen the cardiotoxicity evoked by doxorubicin [57]. The additive use of EGCG or resveratrol ameliorated cisplatin-induced renal toxicity, inflammation and oxidative-stress [58]. Overall, while these studies hold some promise, still more adequate, meticulous/reliable studies should be deployed, particularly to Chinese-herbal-medicine combinations, so as to precisely delineate their combinatorial actions and exact clinical utility.
4. Chemosensitization (PM-evoked abrogation of tumor resistance to chemotherapy)
Although marked progress was achieved in understanding triggers, treatments, and prognosis of cancer, its overall death rate has not declined significantly. The management options available encompass surgery, radiotherapy, and chemotherapy. However, chemotherapy is often used as a core regimen in the handling of most cancers. Nevertheless, the development of tumor resistance to chemotherapy (chemoresistance) constitutes a major hurdle in cancer therapy, thereby aggravating the disease prognosis and patient’s quality of life [24,39]. Therefore, there is a compelling demand to reach a strategy that blunts chemoresistance and get cancer cells sensitized to actions of chemotherapeutic drugs. Chemosensitization is an approach to overcome chemoresistance. It targets the use of one drug to enhance the activity of another by combating the mechanisms behind resistance. Prominent and frontier such candidate chemosensitizers have been natural phytochemicals (PMs), for their established safety and merits in chemoprevention.
Although marked progress was achieved in understanding triggers, treatments, and prognosis of cancer, its overall death rate has not declined significantly. The management options available encompass surgery, radiotherapy, and chemotherapy. However, chemotherapy is often used as a core regimen in the handling of most cancers. Nevertheless, the development of tumor resistance to chemotherapy (chemoresistance) constitutes a major hurdle in cancer therapy, thereby aggravating the disease prognosis and patient’s quality of life [24,39]. Therefore, there is a compelling demand to reach a strategy that blunts chemoresistance and get cancer cells sensitized to actions of chemotherapeutic drugs. Chemosensitization is an approach to overcome chemoresistance. It targets the use of one drug to enhance the activity of another by combating the mechanisms behind resistance. Prominent and frontier such candidate chemosensitizers have been natural phytochemicals (PMs), for their established safety and merits in chemoprevention.
PMs and herbs are intended to abate, bypass, or silence the cellular and molecular mechanisms underlying chemoresistance. Cancer cells develop resistance via a variety of pathways and targets, which include: 1) Alterations in cancer-cell “uptake or efflux” of chemotherapeutic drugs to reduce their availability at the site of action. Drug efflux from cells is mediated by the transporter proteins “multidrug transporters”, of which the coherent ones with chemoresistance include multidrug resistance protein (MDR, P-gp), and breast cancer resistance protein (BRCP). Overexpression and enhanced activity of transporter proteins have further been subject to regulation by inflammation and oxidative stress, two prominent and inevitable events that accompany cancer [59-61]. 2) Metabolic inactivation of chemotherapeutic agents also sequestrates their levels available for chemotherapeutic actions. Commonly engaged enzymes in such inactivation include glutathione/glutathione S-transferase (GSH/GST) system and dihydropyrimidine dehydrogenase (DPD). The latter has been implicated in the inactivation of “5-Fluorouracil (5-FU)”, thereby blunting its efficacy, as witnessed in colorectal cancer cells [62-64]. 3) Alterations in chemotherapy-target molecules (e.g. topoisomerase-II), or in signaling molecules (e.g. MAPKs, growth-factors, and apoptotic effectors) [65-68]. 4) Enhanced DNA-repair in cancer cells, which aims to circumvent the damaging effects of chemotherapeutic drugs on tumor DNA. Thus, cancer cells have the means and capacity to elicit direct repair, mismatch repair, base excision repair, and nucleotide excision repair [69,70]. 5) Constitutive or prolonged activation of nuclear transcription factors, as with (NF-κB) and (STAT-3) pathways, with consequent upregulation of their downstream genes. NF-κB regulates hundreds of genes that are involved in immunoregulation, inflammation, carcinogenesis, growth and apoptosis. Thus, constitutive activation of NF-κB delays, opposes, or blocks chemotherapy-induced apoptosis in tumor cells [71-75]. The STAT3 transcription factor is activated by tyrosine phosphorylation downstream from growth factors and cytokines. Recruitment of STAT-3 triggers multiple-gene expressional changes, which eventually mediate tumor resistance to actions of chemotherapeutic drugs [76-80]. 6) The cell cycle machinery is another likely target of resistance at the levels of its proteins and kinases (CDKs) [81]. All of the above mechanisms can be deregulated by PMs at one or more target to overcome drug resistance. Commonly reported such PMs include curcumin, EGCG, proanthocyanidins, genistein, resveratrol, silymarin, β-sitosterol, and quercetin [82]. Resveratrol, for instance, can chemosensitize tumor cells by targeting multiple avenues, including drug transporters, cell proliferative proteins, cell survival proteins, apoptosis, and members of the NF-κB and STAT-3-dependent signaling pathways [83-84].
Perspectives AND Conclusions
The complex biology of cancer development requires relatively multitarget treatment strategies. Thus, the deployment of synergy combinations of conventional chemotherapeutic drugs with PMs has promoted curative effects, reduced adverse events and improved patient immunity, eventually aiming to enhance quality of life and prolong patient lifespan. Abundance and outcomes from cell lines and animal models far exceed those from the clinic. However, thanks to advances in recent technology, as with nanomedicine, genomics, metabolomics [85], high throughput target screening and evidence-based drug and molecular networking, PMs are gaining more ground every day. Their utility in mitigating cancer cell resistance and drug-failure of chemotherapy, and records in the area of chemoprevention, remains such critical and promising enough to mandate intensive future clinical trials in such directions.
The complex biology of cancer development requires relatively multitarget treatment strategies. Thus, the deployment of synergy combinations of conventional chemotherapeutic drugs with PMs has promoted curative effects, reduced adverse events and improved patient immunity, eventually aiming to enhance quality of life and prolong patient lifespan. Abundance and outcomes from cell lines and animal models far exceed those from the clinic. However, thanks to advances in recent technology, as with nanomedicine, genomics, metabolomics [85], high throughput target screening and evidence-based drug and molecular networking, PMs are gaining more ground every day. Their utility in mitigating cancer cell resistance and drug-failure of chemotherapy, and records in the area of chemoprevention, remains such critical and promising enough to mandate intensive future clinical trials in such directions.
References
- Apaya MK., et al. “Phytomedicine polypharmacology: Cancer therapy through modulating the tumor microenvironment and oxylipin dynamics”. Pharmacology & Therapeutics 162 (2016): 58-68.
- El-Mowafy AM. “Herbal Therapy: Can Omics Technology Create Order from Chaos?” Biochemistry & Analytical Biochemistry 1.8 (2012): 1-3.
- El-Mowafy AM., et al. “Evaluation of the renal protective effects of the green-tea (EGCG) and red-grape's resveratrol: role of oxidative stress and inflammatory cytokines”. Natural Product Research 25.8 (2011): 850-856.
- El-Mowafy AM and Alkhalaf M. “Resveratrol activates adenylyl-cyclase in humanbreast cancer cells: a novel, estrogen receptor-independent cytostatic mechanism”. Carcinogenesis 24.5 (2003): 869-873.
- He B., et al. “Combination therapeutics in complex diseases”. Journal of Cellular and Molecular Medicine 20.12 (2016): 2231-2240.
- Giovanni Konat Zorzi., et al. “On the use of nanotechnology-based strategies for association of complex matrices from plant extracts”. Revista Brasileira de Farmacognosia 25.4 (2015): 426-436.
- GLOBOCON 2012. Estimated cancer incidence, mortality and prevalence worldwide in 2012.
- Curado MP., et al. “Cancer Incidence in Five Continents. Vol. X”. IARC Press, Lyon, France, 2013.
- Tacar O., et al. “Doxorubicin: an update on anticancer molecular action, toxicity and novel drug delivery systems”. Journal of Pharmacy and Pharmacology 65.2 (2013): 157-170.
- Kachalaki S., et al. “Cancer chemoresistance; biochemical and molecular aspects: a brief overview”. European Journal of Pharmaceutical Sciences 89 (2016): 20-30.
- Cragg GM., et al. “Impact of natural products on developing new anti-cancer agents”. Chemical Reviews 109.7 (2009): 3012-3043.
- Pache RA., et al. “NetAligner-a network alignment server to compare complexes, pathways and whole interactomes”. Nucleic acids research 40(Web Server issue) (2012): W157–161.
- Anighoro A., et al. “Polypharmacology: challenges and opportunities in drug discovery”. Journal of medicinal chemistry 57.19 (2014): 7874-7887.
- Rask-Andersen M., et al. “Advances in kinase targeting: current clinical use and clinical trials”. Trends in pharmacological sciences 35.11 (2014): 604-620.
- Azmi AS and Mohammad RM. “Rectifying cancer drug discovery through network pharmacology”. Future Medicinal Chemistry 6.5 (2014): 529-539.
- Barabasi AL., et al. “Network medicine: a network-based approach to human disease”. Nature reviews genetics 12 (2011): 56-68.
- Espinoza-Fonseca LM. “The benefits of the multi-target approach in drug design and discovery”. Bioorganic & Medicinal Chemistry 14.4 (2006): 896–897.
- Mencher SK and Wang LG. “Promiscuous drugs compared to selective drugs (promiscuity can be a virtue)”. BMC Clinical Pharmacology 5.3 (2005):
- Hopkins AL. “Network pharmacology: the next paradigm in drug discovery”. Nature chemical biology 4.11 (2008): 682–690.
- Xie L., et al. “Novel computational approaches to polypharmacology as a means to define responses to individual drugs”. Annual Review of Pharmacology and Toxicology 52 (2012): 361–379.
- Efferth T and Koch E. “Complex interactions between phytochemicals. The multi-target therapeutic concept of phytotherapy”. Current Drug Targets 12.1 (2011): 122–132.
- Lee JH., et al. “Dietary phytochemicals and cancer prevention: Nrf2 signaling, epigenetics, and cell death mechanisms in blocking cancer initiation and progression”. Pharmacology & Therapeutics 137.2 (2013): 153-171.
- Finley JW., et al. “Antioxidants in foods: state of the science important to the food industry”. Journal of Agricultural and Food Chemistry 59.13 (2011): 6837–6846.
- Liao CY., et al. “Novel Investigations of Flavonoids as Chemopreventive Agents for Hepatocellular Carcinoma”. BioMed Research International 2015 (2015): 840542.
- Nithianandarajah-Jones GN., et al. “ERK5: structure, regulation and function”. Cellular Signalling 24.11 (2012): 2187–2196.
- Jing N and Tweardy DJ. “Targeting Stat3 in cancer therapy”. Anticancer Drugs 16.6 (2005): 601-607.
- Bhardwaj A., et al. “Resveratrol inhibits proliferation, induces apoptosis, and overcomes chemoresistance through down-regulation of STAT3 and nuclear factor-kappaB-regulated antiapoptotic and cell survival gene products in human multiple myeloma cells”. Blood 109.6 (2007): 2293–2302.
- Senggunprai L., et al. “Quercetin, EGCG exhibit chemopreventive effects in cholangiocarcinoma cells via suppression of JAK/STAT signaling pathway”. Phytotherapy research 28.6 (2014): 841–848.
- Rajendran P., et al. “Honokiol inhibits signal transducer and activator of transcription-3 signaling, proliferation, and survival of hepatocellular carcinoma cells via the protein tyrosine phosphatase SHP-1”. Journal of cellular physiology 227.5 (2012): 2184–2195.
- Wattenberg LW. “Chemoprophylaxis of carcinogenesis: a review”. Cancer Research 26.7 (1966): 1520–1526.
- Lippman SM and Hong WK. “Cancer prevention science and practice”. Cancer Research 62.18 (2002): 5119–5125.
- Maru G. “An Update on Cancer Prevention Approaches”. Biomedical Research Journal 1.2 (2014): 146-172.
- Bowden GT., et al. “Oncogene activation and tumor suppressor gene inactivation during multistage mouse skin carcinogenesis”. Cancer Research 54. S7 (1994): 1882s-1885s.
- Solomon H., et al. “Inactivation of the p53 tumor suppressor gene and activation of the Ras oncogene: cooperative events in tumorigenesis”. Discovery Medicine 9.48 (2010): 448-454.
- Hanahan D and Weinberg RA. “Hallmarks of cancer: the next generation”. Cell 144.5 (2011): 646-674.
- Surh YJ. “Cancer chemoprevention with dietary phytochemicals”. Nature Reviews Cancer 3.10 (2003): 768-780.
- Patel R., et al. “Chemopreventive herbal anti-oxidants: current status and future perspectives”. Journal of Clinical Biochemistry and Nutrition 40.2 (2007): 82-91.
- Crowell JA. “The chemopreventive agent development research program in the Division of Cancer Prevention of the US National Cancer Institute: an overview”. European Journal of Cancer 41.13 (2005): 1889-1910.
- Maru GB., et al. “Understanding the molecular mechanisms of cancer prevention by dietary phytochemicals: From experimental models to clinical trials”. World Journal of Biological Chemistry 7.1 (2016): 88-99.
- Sharma RA., et al. “Pharmacodynamic and pharmacokinetic study of oral Curcuma extract in patients with colorectal cancer”. Clinical Cancer Research 7.7 (2001): 1894-1900.
- Vásquez-Garzón VR., et al. “The chemopreventive capacity of quercetin to induce programmed cell death in hepatocarcinogenesis”. Toxicologic Pathology 41.6 (2013): 857-865.
- Wang CZ., et al. “Cancer Chemoprevention Effects of Ginger and its Active Constituents: Potential for New Drug Discovery”. The American Journal of Chinese Medicine 43.7 (2015): 1351-1363.
- Patel KR., et al. “Clinical pharmacology of resveratrol and its metabolites in colorectal cancer patients”. Cancer Research 70.19 (2010): 7392-7399.
- Aqil F., et al. “Bioavailability of phytochemicals and its enhancement by drug delivery systems”. Cancer Letters 334.1 (2013): 133-141.
- Torre LA., et al. “Global cancer statistics, 2012”. CA: A Cancer Journal for Clinicians 65.2 (2015): 87-108.
- El-Mowafy AM., et al. "Prominent chemopreventive and chemoenhancing effects for resveratrol: unraveling molecular targets and the role of C-reactive protein". Chemotherapy 56.1 (2010): 60-65.
- Yu LL., et al. “Curcumin reverses chemoresistance of human gastric cancer cells by downregulating the NF-kappa B transcription factor”. Oncology Reports 26.5 (2011): 1197-1203.
- Thangapazham RL., et al. “Multiple molecular targets in cancer chemoprevention by curcumin”. American Association of Pharmaceutical Scientists 8.3 (2006): E443-E449.
- Rahmani AH., et al. “Curcumin: a potential candidate in prevention of cancer via modulation of molecular pathways”. BioMed Research International (2014).
- Cai YY., et al. “Combined effects of curcumin and triptolide on an ovarian cancer cell line”. Asian Pacific Journal of Cancer Prevention 14.7 (2013): 4267-4271.
- Guo J., et al. “Synergistic effects of curcumin with emodin against the proliferation and invasion of breast cancer cells through upregulation of miR-34a”. Molecular and Cellular Biochemistry 382. 1-2 (2013): 103-111.
- Masuelli L., et al. “Resveratrol potentiates the in vitro and in vivo anti-tumoral effects of curcumin in head and neck carcinomas”. Oncotarget 5.21 (2014): 10745-10762.
- Dong J., et al. “Shenqi fuzheng, an injection concocted from Chinese medicinal herbs, combined with platinum-based chemotherapy for advanced non-small cell lung cancer: a systematic review”. Journal of Experimental & Clinical Cancer Research 29.1 (2010):137.
- Dai Z., et al. “Clinical effects of shenqi fuzheng injection in the neoadjuvant chemotherapy for local advanced breast cancer and the effects on T-lymphocyte subsets”. Journal of Traditional Chinese Medicine 28.1 (2008): 34-38.
- McCulloch M., et al. “Astragalus-based Chinese herbs and platinum-based chemotherapy for advanced non-small-cell lung cancer: meta-analysis of randomized trials”. Journal of Clinical Oncology 24.3 (2006): 419-430.
- Guo L., et al. Astragalus polysaccharide injection integrated with vinorelbine and cisplatin for patients with advanced non-small cell lung cancer: effects on quality of life and survival. Medical Oncology 29.3 (2012): 1656-1662.
- Sin TK., et al. “Resveratrol protects against doxorubicin-induced cardiotoxicity in aged hearts through the SIRT1-USP7 axis”. The Journal of Physiology 593.8 (2015): 1887-1899.
- El-Mowafy AM., et al. “Novel chemotherapeutic and renal protective effects for the green tea (EGCG): role of oxidative stress and inflammatory-cytokine signaling”. Phytomedicine 17.14 (2010): 1067-1075.
- Huang Y., et al. “Membrane transporters and channels: role of the transportome in cancer chemosensitivity and chemoresistance”. Cancer Research 64.12 (2004): 4294-4301.
- Endicott JA and Ling V. “The biochemistry of P-glycoprotein-mediated multidrug resistance”. Annual Review of Biochemistry 58 (1989):137-171.
- Lee JS., et al. “Reduced drug accumulation and multidrug resistance in human breast cancer cells without associated P-glycoprotein or MRP overexpression”. Journal of Cellular Biochemistry 65.4 (1997): 513-526.
- Batist G., et al. “Overexpression of a novel anionic glutathione transferase in multidrug-resistant human breast cancer cells”. The Journal of Biological Chemistry 261.33 (1986): 15544-15549.
- Chao CC., et al. “Overexpression of glutathione S-transferase and elevation of thiol pools in a multidrug-resistant human colon cancer cell line”. Molecular Pharmacology 41.1 (1992): 69-75.
- Diasio RB and Harris BE. “Clinical pharmacology of 5-fluorouracil”. Clinical Pharmacokinetics 16.4 (1989): 215-237.
- Yarden Y and Sliwkowski MX. “Untangling the ErbB signalling network”. Nature Reviews Molecular Cell Biology 2.2 (2001): 127-137.
- Chen X., et al. “Enhanced drug resistance in cells coexpressing ErbB2 with EGF receptor or ErbB3”. Biochemical and Biophysical Research Communications 277.3 (2000): 757-763.
- Magne N., et al. “Influence of epidermal growth factor receptor (EGFR), p53 and intrinsic MAP kinase pathway status of tumour cells on the antiproliferative effect of ZD1839 (“Iressa”).” British Journal of Cancer 86.9 (2002):1518-1523.
- Levine AJ. “p53, the cellular gatekeeper for growth and division”. Cell 88.3 (1997): 323-331.
- O'Connor PM., et al. “Characterization of the p53 tumor suppressor pathway in cell lines of the National Cancer Institute anticancer drug screen and correlations with the growth-inhibitory potency of 123 anticancer agents”. Cancer Research 57.19 (1997): 4285-4300.
- Chun E and Lee KY. “Bcl-2 and Bcl-xL are important for the induction of paclitaxel resistance in human hepatocellular carcinoma cells”. Biochemical and Biophysical Research Communications 315.3 (2004): 771-779.
- Tsang W P and Kwok TT. “Epigallocatechin gallate up-regulation of miR-16 and induction of apoptosis in human cancer cells”. The Journal of Nutritional Biochemistry 21.2 (2010): 140-146.
- Tong JL., et al. “Epigallocatechin gallate induces apoptosis in human hepatocellular carcinoma HepG2 cells via TGF/Smad signaling pathway”. Zhonghua Zhong Liu Za Zhi 31.9 (2009): 646-650.
- Darweish MM., et al. “Chemopreventive and hepatoprotective effects of Epigallocatechin-gallate against hepatocellular carcinoma: role of heparan sulfate proteoglycans pathway”. Journal of Pharmacy and Pharmacology 66.7 (2014): 1032-1045.
- Chen K., et al. “Baicalein inhibits the invasion and metastatic capabilities of hepatocellular carcinoma cells via down-regulation of the ERK pathway”. Plos one 8.9 (2013). e72927.
- Chang WH., et al. “Effect of baicalein on apoptosis of the human Hep G2 cell line was induced by mitochondrial dysfunction”. Planta Medica 68.4 (2002): 302-306.
- Jin CY., et al. “Genistein enhances TRAIL-induced apoptosis through inhibition of p38 MAPK signaling in human hepatocellular carcinoma Hep3B cells”. Chemico-Biological Interactions 180.2 (2009): 143-150.
- Liu W., et al. MAC related mitochondrial pathway in oroxylin A induces apoptosis in human hepatocellular carcinoma HepG2 cells. Cancer Letters 284.2 (2009): 198-207.
- Zhang HT., et al. “Galangin induces apoptosis in hepatocellular carcinoma cells through the caspase 8/t-Bid mitochondrial pathway”. Journal of Asian Natural Products Research 14.7 (2012): 626-633.
- Granado-Serrano AB., et al. “Quercetin induces apoptosis via caspase activation, regulation of Bcl-2, and inhibition of PI-3-kinase/Akt and ERK pathways in a human hepatoma cell line (HepG2).” Journal of Nutrition 136.11 (2006): 2715-2721.
- Momeny M., et al. “Effects of silibinin on cell growth and invasive properties of a human hepatocellular carcinoma cell line, HepG-2, through inhibition of extracellular signal-regulated kinase 1/2 phosphorylation”. European Journal of Pharmacology 591.1-3 (2008): 13-20.
- Meeran SM and Katiyar SK. “Cell cycle control as a basis for cancer chemoprevention through dietary agents”. Frontiers in Bioscience 13 (2008): 2191-2202.
- Vundru SS., et al. “β-Sitosterol induces G1 arrest and causesdepolarization of mitochondrial membrane potential in breast carcinoma MDA-MB-231cells”. BMC Complementary and Alternative Medicine 13 (2013): 280.
- Gupta SC., et al. “Chemosensitization of tumors by resveratrol”. Annals of the New York Academy of Sciences 1215 (2011): 150-160.
- El-Mowafy AM and Alkhalaf M. “Resveratrol activates adenylyl-cyclase in human breast cancer cells: a novel, estrogen receptor-independent cytostatic mechanism”. Carcinogenesis 24.5 (2003): 869-873.
- El Mowafy AM. “Emerging Clues and Altered Metabolic Findings in Autism: Breakthroughs and Prospects from Omics Studies”. Autism Open Access (2016).
Citation:
Abdalla M El-Mowafy. “Phytomedicines: far Beyond Cytotoxicity in Cancer therapy. Sole Multitarget-Polypharmacology,
Chemopreventive and Safety Profiles: Combinatorial Synergy, Chemosensitization and Mitigation of Chemotherapy Adverse-Reactions.”.
Nutrition and Food Toxicology 2.3 (2017): 359-370.
Copyright: © 2017 Abdalla M El-Mowafy. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.