Case Report
Volume 1 Issue 4 - 2017
Anterior maxillary distraction: a case report depicting its significance over a repeated lefort I surgery case
1Dr. Shafees Koya, Assistant Professor Dept. of Orthodontics and Dentofacial Orthopaedics, Yenepoya Dental College, Yenepoya University
Mangalore, Karnataka, India
2Dr. Akhter Husain, Professor and Head Dept. of Orthodontics and Dentofacial Orthopaedics Yenepoya Dental College,Yenepoya University Mangalore, Karnataka,India
3Dr. Mohammed Basheer Naha, Post graduate Dept. of Orthodontics and Dentofacial Orthopaedics, Yenepoya Dental College,Yenepoya University Mangalore, Karnataka, India
4Dr. Musthafa K, Oral and maxillofacial Surgeon Kanachur Medical College Mangalore
2Dr. Akhter Husain, Professor and Head Dept. of Orthodontics and Dentofacial Orthopaedics Yenepoya Dental College,Yenepoya University Mangalore, Karnataka,India
3Dr. Mohammed Basheer Naha, Post graduate Dept. of Orthodontics and Dentofacial Orthopaedics, Yenepoya Dental College,Yenepoya University Mangalore, Karnataka, India
4Dr. Musthafa K, Oral and maxillofacial Surgeon Kanachur Medical College Mangalore
*Corresponding Author: Shafees Koya, Assistant Professor Deportment of Orthodontics and Dentofacial Orthopaedics, Yenepoya
Dental College, Yenepoya University Mangalore, Karnataka, India.
Received: August 30, 2017; Published: September 11, 2017
Abstract
A 19-year-old female patient with complete cleft lip and palate on the left side (repair done) with unpleasing profile despite repeated lefort I surgery was reported. On clinical examination patient presented with concave profile, retrusive upper lip and a negative over jet of 3-4 mm. Intra orally patient had angles class II molar and canine relation, congenitally missing upper left lateral incisor with distally tipped anteriors towards the missing tooth region. Treatment involved was anterior maxillary distraction followed by fixed mechanotherapy. A distraction of 7-8 mm was achieved over a period of 2 weeks. The case was finished in a reasonable occlusion and the profile was improved. This case report depicts the significance of anterior maxillary distraction over a repeated lefort I surgery case.
Keywords: Cleft lip & palate; Anterior maxillary distraction; Lefort I; Maxillary Hypoplasia
Introduction
Correction of the hypoplastic maxilla in cleft patients is a great challenge due to difficulty in mobilizing the hypoplastic maxilla because of the scarring resulted from palatoplasty. Generally, Lefort I surgeries are done to correct the maxillary hypoplasia. The limitation of conventional Le Fort I osteotomy is that a major advancement may make stabilization difficult, and the added effect of palatal scarring can result in significant postsurgical relapse. In contrast, the advantage of distraction osteogenesis is its ability to do major advancement without much relapse due to the formation of mature lamellar bone. In a study done on sheep, the maxilla was advanced 40 mm by distraction osteogenesis, with only 7% relapse at 1-year follow-up [1]. In another experimental study using dogs, cephalometric evaluation of 14 mm of maxillary advancement by maxillary distraction demonstrated stable results at 1-year follow-up [2]. Anterior maxillary distraction is the procedure in which the maxilla is distracted forward with the help of an intraoral appliance after the surgical osteotomy cuts are given.
The aim of this article is to describe a technique involving the distraction of the hypoplastic maxilla after failed repeated lefort 1 surgeries in a cleft lip and palate patient.
Case Report
Diagnosis and treatment planning
A 19-year-old female patient (Figure 1) with chief complaint that despite repeated lefort I surgeries to correct her maxillary retrusion she was not satisfied with the results. On extra oral clinical examination, patient presented with class III skeletal pattern and average growth pattern. She had a scar of cleft lip repair on the left side, asymmetrical nose, retrusive upper lip and protrusive lower lip. She had a concave profile, acute nasolabial angle and normal mentolabial sulcus. She had a non-consonant smile with exposure of lower incisors. On intra oral examination, she had an Angles class II molar and canine relation with congenitally missing upper left lateral incisor with distally tipped anteriors towards the missing tooth region creating a midline shift. She presented with 4mm negative over jet, normal deep bite, anterior cross bite and minor crowding in both the arches. Her midline was shifted with respect to facial midline and lower mid line by 4-5 mm.
A 19-year-old female patient (Figure 1) with chief complaint that despite repeated lefort I surgeries to correct her maxillary retrusion she was not satisfied with the results. On extra oral clinical examination, patient presented with class III skeletal pattern and average growth pattern. She had a scar of cleft lip repair on the left side, asymmetrical nose, retrusive upper lip and protrusive lower lip. She had a concave profile, acute nasolabial angle and normal mentolabial sulcus. She had a non-consonant smile with exposure of lower incisors. On intra oral examination, she had an Angles class II molar and canine relation with congenitally missing upper left lateral incisor with distally tipped anteriors towards the missing tooth region creating a midline shift. She presented with 4mm negative over jet, normal deep bite, anterior cross bite and minor crowding in both the arches. Her midline was shifted with respect to facial midline and lower mid line by 4-5 mm.
Cephalometric analysis (Table 1) revealed a Class III skeletal antero-posterior relationship with an ANB of -3°. The maxilla was backwardly placed (SNA-76°) and decreased in length (effective maxillary length-84 mm), but the mandible was normally placed (SNB-79°) and normal in length (effective mandibular length-121 mm). The dental parameters indicated the upper incisors retroclined by 5° to maxillary plane (102°). The lower incisors were normally inclined to mandibular plane (95°).
| Norm | Pre-Treatment | Post Treatment | Difference | |
| SNA | 82° ± 2 | 76° | 81 | 3° |
| SNB | 80° ± 2 | 79° | 80° | 1° |
| ANB | 3° ± 1 | -3° | 1° | 4° |
| Upper incisor to maxillary plane angle | 108° ± 5 | 102° | 107° | -5° |
| Lower incisor to mandibular plane angle | 92° ± 5 | 98° | 95° | -3° |
| Interincisal angle | 133° ± 10 | 128° | 125° | -3° |
| Effective maxillary length | 93.6 ± 3.2 mm | 84 mm | 90 mm | 6 mm |
| Effective mandibular length | 121.6 ± 4.5 mm | 120 mm | 121 mm | 1 mm |
| NLA | 90-110° | 89° | 98° | 9° |
| SN-Go Gn | 32° | 300 | 320 | 20 |
Table 1: Pre and Post treatment cephalometric values.
Treatment objectives were to correct Class III skeletal pattern & maintain skeletal proportions, correct the negative over jet, correct the midline, relief of anterior crowding and to improve her smile. Treatment plan decided was to perform anterior maxillary distraction to bring about maxillary advancement to correct her class III skeletal proportion followed by fixed orthodontic treatment. Non-extraction treatment plan was decided with the conversion of upper left canine to lateral incisor and first premolar to canine. The case was decided to finish in a class II molar and class I canine relationship in the left side.
Treatment Progress
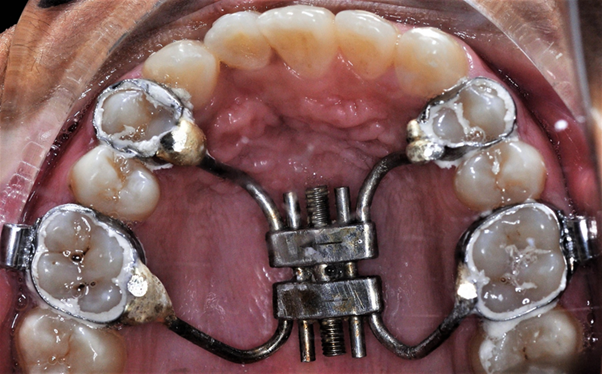
A Hyrax orthodontic appliance (Hyrax expansion screw, Leone) is prepared beforehand on a maxillary dental model (Figure 2). The appliance is oriented so that its activation will produce anteroposterior movement rather than the traditional transverse expansion. It normally has 4 arms. The 2 anterior arms were soldered to the orthodontic bands of the first premolars of each side and the 2 posterior arms was soldered to the first molars.
A Hyrax orthodontic appliance (Hyrax expansion screw, Leone) is prepared beforehand on a maxillary dental model (Figure 2). The appliance is oriented so that its activation will produce anteroposterior movement rather than the traditional transverse expansion. It normally has 4 arms. The 2 anterior arms were soldered to the orthodontic bands of the first premolars of each side and the 2 posterior arms was soldered to the first molars.
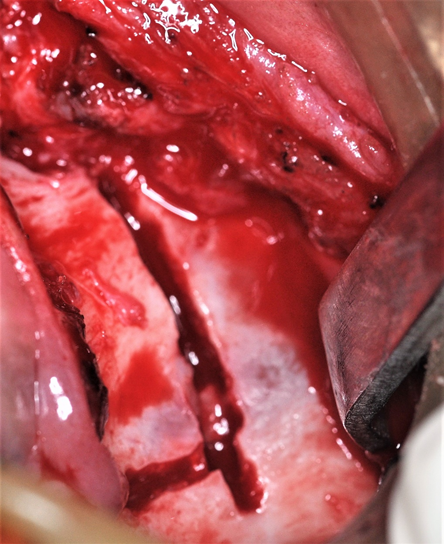
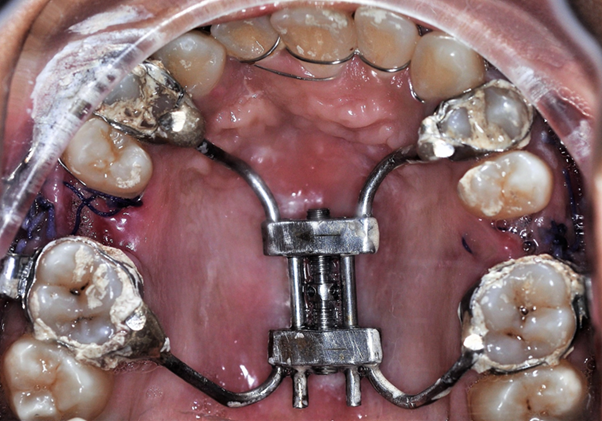
Under general anaesthesia, a horizontal maxillary vestibular incision is made from first molar to the other (Figure 3). The mucoperiosteum is then reflected upward, exposing the osteotomy site up to the infraorbital foramen. A buccal linear osteotomy cut is made above the apices between the maxillary first molar and second premolar on both the sides. The lateral nasal wall is cut from the pyriform rim by a small osteotome at the same horizontal level with the nasal mucosa protected. The anterior maxilla is then down fractured and slightly mobilized, while the palatal mucosal pedicle is maintained the prefabricated Hyrax appliance is then inserted into the maxilla (Figure 4). The orthodontic bands attached to the four appliance arms are then cemented to the selected teeth. The maxilla then becomes reasonably stable and the mucosal wound is closed primarily. The appliance was activated after 2 days onwards at a rate of 1 mm per day, using 4 quarter turns. The patient was admitted for 14 days and an advancement of maxilla was achieved by 8 mm (Figure 5). The appliance was continued for the next 8 months as a consolidation period.
Upper and lowers were bonded with pre-adjusted edgewise fixed appliances (0.022"x0.028" slot) with MBT prescription and 0.014” nickel titanium arch wire were placed. The wires were sequencely changed from 0.016 NiTi to 0.019 X 0.025 NiTi arch wire. After sufficient levelling and aligning was achieved the conversion of upper left canine to lateral incisor and first premolar to canine was done. Settling elastics were given to settle the posterior occlusion. Fixed appliance was debonded after overall active treatment of 26 months. Beggs wrap around retainers were given for the upper arch and lower lingual fixed retainer was given.
Treatment Results
The patient was successfully treated by anterior maxillary distraction with the advancement of maxilla by 8mm followed by non-extraction treatment approach over 26 months. Her post treatment smile was improved exceptionally. A reasonable functional and aesthetic result was achieved being a cleft lip and palate case (Figure 6). A class I skeletal base with average proportions were achieved along with an Angles class II molar and class I canine relation in the left side, but the right side had a compromised finish in a relation close to class I molar and canine. The negative -4mm over jet was successfully reduced to within normal limits. The distally tipped anteriors towards the missing tooth region was corrected and later the conversion of upper left canine to lateral incisor and first premolar to canine was done correcting the midline discrepancy especially with respect to her facial midline. Patient profile was improved to a near straight profile. Nasolabial angle was corrected to its normal. Lips were competent at rest. Incisal show at smile was dramatically improved compared to pre-treatment.
The patient was successfully treated by anterior maxillary distraction with the advancement of maxilla by 8mm followed by non-extraction treatment approach over 26 months. Her post treatment smile was improved exceptionally. A reasonable functional and aesthetic result was achieved being a cleft lip and palate case (Figure 6). A class I skeletal base with average proportions were achieved along with an Angles class II molar and class I canine relation in the left side, but the right side had a compromised finish in a relation close to class I molar and canine. The negative -4mm over jet was successfully reduced to within normal limits. The distally tipped anteriors towards the missing tooth region was corrected and later the conversion of upper left canine to lateral incisor and first premolar to canine was done correcting the midline discrepancy especially with respect to her facial midline. Patient profile was improved to a near straight profile. Nasolabial angle was corrected to its normal. Lips were competent at rest. Incisal show at smile was dramatically improved compared to pre-treatment.
On cephalometric analysis (Table 1), SNA was increased by 3° suggesting forward movement of maxilla. There was no much change
in SNB. ANB was increased by 4° indicating a class I skeletal pattern, thus showing improvement in the sagittal relationship. Effective
maxillary length was also increased by 6 mm suggesting forward movement of maxilla. The overall super imposition demonstrated the
forward movement of maxilla with slight upper incisor proclination. In analysis of dental parameters upper incisor to maxillary plane
angle increased by 4° and the lower incisors to mandibular plane were decreased by 3° bringing it to the normal inclination. Overall the
patient was happy with the results improving her confidence and social life being a cleft patient and she is now pursuing nursing course
in a reputed university.
Discussion
Patients with severe maxillary hypoplasia secondary to congenital facial deformities are challenging problems for the surgeon. The primary cleft lip and palate repair done during infancy and early childhood improves the facial appearance, speech and deglutition, but these early surgical interventions cause impairment of maxillary growth, producing secondary deformities of the jaw and malocclusion. Traditional orthodontic and surgical procedures are done to overcome this deformity.
Distraction osteogenesis [3-6] is a good armamentarium for surgeons especially patients with major skeletal discrepancy. With distraction osteogenesis, the maxillary advancement can exceed the 10-mm limitation compared with traditional orthognathic procedures. In a meta-analysis [7]of cleft maxillary osteotomy and distraction osteogenesis based on 98 articles from 1966 to 2003, Cheung and Chua found that 72 articles related to cleft maxillary osteotomy performed on 1,418 cleft patients, and that the other 26 articles described 276 cleft patients who had undergone maxillary distraction osteogenesis. This study concluded that distraction osteogenesis tends to be preferred to conventional osteotomy for younger cleft patients with more severe deformities. In such cases, it is feasible to use distraction to achieve moderate to large movement of the maxilla. More studies [8,9] have demonstrated the efficiency of maxillary distraction over the conventional Le Fort I osteotomy. Kloukos [10]., et al. did a meta-analysis in 2016 regarding the effects and long-term results of maxillary distraction osteogenesis compared to orthognathic surgery for the treatment of hypoplastic maxilla in people with cleft lip and palate.
They concluded that distraction osteogenesis may produce more satisfactory results; however, further prospective research comprising assessment of a larger sample size with participants with different facial characteristics is required to confirm possible true differences between interventions. The advantages of distraction over conventional orthognathic are many but specifically in cleft palate operated patients it helps in two ways. (1) Avoidance of relapse due to scar tissue [11]. (2) Preventing any further speech disturbance due to the increase in velopharyngeal insufficiency caused by sudden maxillary advancement [12]. One of the disadvantage of distraction osteogenesis is lack of vector control which can result in anterior open bite. The precision of distraction depends primarily on the vector planning to avoid open bite. This can be achieved preoperatively by simulated model surgery.
The newly formed soft bone after distraction could be moulded by using inter arch elastics to achieve better interdigitation of teeth. This settling of the occluding teeth might contribute to maintain the sagittal advancement. The forward movement of the entire anterior maxillary segment also improves upper lip and paranasal prominence in cleft lip and palate patients.
Distraction Osteogenesis with the help of a hyrax screw placed in such a way that anteroposterior movement is achieved was found to be effective in the treatment of this patient. Patient's compliance with hyrax appliance for anterior maxillary distraction was good. In addition, the cost of this appliance is very minimal compared with internal external distractors. Cases are being reported with distractions done up to 18 mm by similar technique and have given stable outcomes [13]. An integrated treatment plan by orthodontists, prosthodontists, and surgeons are important to bring optimal improvement of the malocclusion and aesthetics.
Conclusion
The case report depicts the significance of anterior maxillary distraction over a failed repeated lefort I advancement surgical case in a cleft lip and palate patient. Inverted Hyrax appliance as an internal distractor was effective, patient compliant and provided good vector control. Maxillary distraction is an alternative technique to correct maxillary hypoplasia.
References
- Rachmiel A., et al. “Midface advancement in sheep by gradual distraction: a 1-year follow-up study”. Journal of Oral and Maxillofacial Surgery 53.5 (1995):525-529.
- Stalmans K., et al. “Cephalometric evaluation of maxillary advancement with an internal distractor in an adult boxer dog”. Orthodontics & Craniofacial Research 6.2 (2003):104-111.
- Block MS., et al. “Anterior maxillary advancement using tooth-supported distraction osteogenesis”. Journal of Oral and Maxillofacial Surgery 53.5 (1995): 561-565.
- Dolanmaz D., et al. “Maxillary anterior segmental advancement by using distraction osteogenesis: A case report”. The Angle Orthodontist 73.2 (2003): 201-205.
- Swennen G., et al. “Maxillary distraction in cleft lip palate patients: A review of six cases”. Journal of Craniofacial Surgery 10.2 (1999): 117-122.
- Gunaseelan R., et al. “Anterior maxillary distraction by tooth-borne palatal distractor”. Journal of Oral and Maxillofacial Surgery 65.5 (2007): 1044-1049.
- Cheung LK and Chua HD. “A meta-analysis of cleft maxillary osteotomy and distraction osteogenesis”. International Journal of Oral and Maxillofacial Surgery 35.1 (2006):14-24.
- Cheung LK., et al. “Stability consideration for internal maxillary distractors”. Journal of Cranio-Maxillo-Facial Surgery 31.3 (2003): 142-148.
- Rachmiel A. “Treatment of maxillary cleft palate: distraction osteogenesis versus orthognathic surgery-part one: Maxillary distraction”. Journal of Oral and Maxillofacial Surgery 65.4 (2007): 753-757.
- Kloukos D., et al. “Maxillary distraction osteogenesis versus orthognathic surgery for cleft lip and palate patients”. The Cochrane Database of Systematic Reviews (2016).
- Hirano A and Suzuki H. “Factors related to relapse after Le Fort I maxillary advancement osteotomy in patients with cleft lip and palate”. The Cleft Palate-Craniofacial Journal 38.1 (2001): 1-10.
- Ko EW., et al. “Velopharyngeal changes after maxillary advancement in cleft patients with distraction osteogenesis using a rigid external distraction device: A 1-year cephalometric follow-up”. Journal of Craniofacial Surgery 10.4 (1999): 312-320.
- Richardson S., et al. “Anterior maxillary distraction using a tooth-borne device for hypoplastic cleft maxillas - A pilot study”. Journal of Oral and Maxillofacial Surgery 69.12 (2011): 542-548.
Citation:
Shafees Koya., et al. “Anterior maxillary distraction: a case report depicting its significance over a repeated lefort I surgery
case”. Oral Health and Dentistry
1.4 (2017): 210-216.
Copyright: © 2017 Shafees Koya., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.