Perspective
Volume 1 Issue 5 - 2017
Simplified Treatment Algorithm for NOE Fracture
1Department of Oral & Maxillofacial Surgery, PMS College of Dental Science & Research
2MDS Department of Oral & Maxillofacial Surgery, Jubilee Mission Medical College and Research Institute
3MDS Department of Oral & Maxillofacial Surgery, PMS College of Dental Science & Research
2MDS Department of Oral & Maxillofacial Surgery, Jubilee Mission Medical College and Research Institute
3MDS Department of Oral & Maxillofacial Surgery, PMS College of Dental Science & Research
*Corresponding Author: Varun Menon P, MDS Department of Oral & Maxillofacial Surgery, Jubilee Mission Medical College and Research Institute, India.
Received: September 10, 2017; Published: September 18, 2017
Abstract
The nasoethmoid region is an important area of the face not only for cosmetic but also in
determining facial projection. Management of NOE fracture is considered one of the most
challenging because diagnosis may be difficult and surgical outcomes can be variable. In this
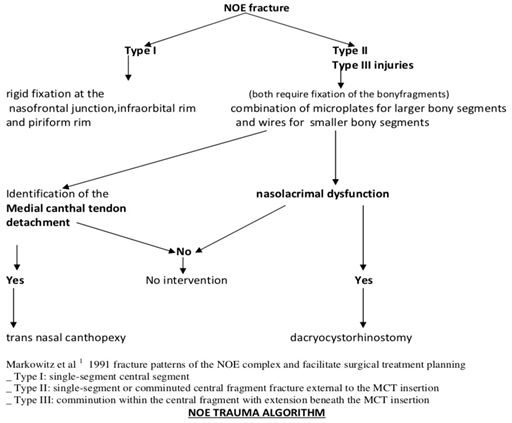
article, we describe a simple clinical algorithm based on Markowitz et al fracture patterns of
the NOE complex and on our clinical experience inorder to facilitate the treatment of NOE
fractures.
Keywords: NOE fracture; Treatment; Algorithm
Introduction
Facial trauma can cause various maxillofacial complications that vary from simple skin abrasions to considerable long-term functional and esthetic defects. Fracture of nasoethmoid and associated bones are commonly referred to as fracture of middle third of facial skeleton. The nasoethmoid fracture represents a challenging surgical problem due to the complexity and density of the anatomic components of the area. Because of the functional and aesthetic implications of the medial can thus, nasolacrimal system, and intraorbital contents, appropriate and timely treatment is crucial to avoid unfavourable sequel. Here we describe a simple clinical algorithm based on Markowitz., et al. [1] fracture patterns of the NOE complex and on our clinical experience in order to facilitate the treatment of NOE fractures.
Discussion
The result of closed manipulation and reduction of nasoethmoidal fractures are unsatisfactory even when supplemented by transnasal wires with compression plates. Such wires and compression plates lie anterior to the critical point where pressure requires to be exerted over the anterior lacrimal crest, particularly the frontal process of maxillary bones. Local skin necrosis under such lead or acrylic plates is frequent complication of this type of treatment. Further, gross separation vertically between the nasal and frontal bones, particularly in the presence of sever mid face comminution, will remain unreduced by closed manipulation. Assessment of patients treated in this way shows an unacceptable incidence of post traumatic telecanthus and complications occurs more frequently when there is evidence of these intercanthal spread prior to reduction.
Secondary reconstruction of this deformity may necessitate craniofacial surgery and results are disappointing. Late repair are plagued with difficulty in identification of the medial canthal ligament and mobilisation of soft tissue in this area [2] as described by Mathog & Bauer in 1979.
Residual deformity in such cases is typified by nasal deformity, the nose being short and saddle shaped with distorted intranasal structures resulting in obstruction .widening of intracanthal distance with prominent epicanthal skin fold is frequently seen. Dysfunction of the lacrimal apparatus is not uncommon.
In 1980 Schultz- Coulon highlighted that the post traumatic telecanthus may not always be avoided, even with prompt surgical treatment [3,4,5], the results are so superior with open reduction that the additional surgical procedure involved are fully justified [4]. Dingman and Natvig in 1964 [4] Advocated open reduction with direct fixation in serious injuries and in 1966 Mustard'e [5].
Described an open technique for restoration of the displaced medial canthal ligament by transnasal wiring. The momentum of open exploration was given impetus by Stranc in 1970 [6] who advocated opening of such injuries with positive clinical signs of increased intercanthal distance, a view supported by Converse and Hogan [7] when they described the 'open sky' approach for comminuted naso-orbital fractures.
The realignment of bone fragment under direct vision is preferable to close approach. This view was confirmed by Bowerman [8,9] in 1975 who also advocated that open exploration and reduction of such fractures was mandatory, particularly if there is increased intracanthal distance, and treatment should be carried out at an early stage provided there are no medical complications. We have devised our treatment algorithm based on Markowitz., et al. [1] 1991 fracture patterns of the NOE complex and on our clinical experience.
Type 1 fractures Treated essentially by fixation of the bone fragment to adjacent surrounding bone. Fixation is done by small miniplates with self-tapping monocortical screws except if the conjoining bony segment is only a small piece of lacrimal bone that may be wired to its normal position using a 28-gauge steel wire. In type 2 and type 3 fractures the treatment plan varies based on whether the medial canthal tendon is still attached and also on nasolacrimal dysfunction as shown above.
In type 2 fracture when the fragment is too small for fixation, trans nasal wiring can be used to position the fragment and medial canthal tendon appropriately. Additional bone grafting may be required.
Type 3 injuries usually require trans nasal fixation of the medial canthal tendon in addition to appropriate reduction of bone fragments and bone grafting. When trans nasal medial canthoplasty is necessary, it must be performed so that the direction of pull on the canthal tendon is posterior and superior. A common mistake is to reattach the canthal tendon too anteriorly, resulting in persistent telecanthus.
Once soft tissue swelling has settled, epiphora secondary to ectropion where punctum of the lower canaliculus is everted from the conjunctiva should be dealt with, by appropriate surgery. Dacrocystitis should be treated by intensive antibiotic therapy .persistent obstruction of the lacrimal system should be investigated by dacrocystography .This will outline the nasolacrimal system and pinpoint the cause of obstruction. The majority of these obstructive symptoms are relieved by dacrocystorhinostomy.
Conclusion
NOE fractures are rare and can be difficult to diagnose and manage successfully. Early diagnosis and surgical management are imperative to achieving an optimal functional and cosmetic outcome and hopefully the above treatment algorithm will benefit clinicians in early diagnosis as well as enabling in appropriate treatment.
References
- Manson PN., et al. “Toward CT –based facial fracture management”. Plastic Reconstructive Surgery 85.2 (1990): 202-212.
- Mathog R. Maxillofacial trauma.Baltimore (MD): William & Wilkins (1984).
- Gruss JS., et al. “The importance of the zygomatic arch in complex midfacial fracture repair and correction of posttraumatic orbitozygomatic deformities”. Plastic reconstructive Surgery 85.6 (1990): 878-890.
- Dingman RO and Natvig P. Surgery of facial fractures. Philadelphia: W.B Saunders; (1964): 226.
- Uglesic V and Virag M. “A method of zygomatic arch stabilization”. British Journal of Oral and Maxillofacial Surgery 32.6 (1994): 396-397.
- Waite PD and Carr DD. “The transconjunctival approach for treating orbital trauma”. Journal of Oral and Maxillofacial Surgery 49.5 (1991): 499-503.
- 7. Baumann A and Eweres R. “Use of the preseptal transconjunctival approach in orbit reconstruction surgery”. Journal of Oral and Maxillofacial Surgery 59.3 (20010: 287-291.
- Tessier P. “The conjunctival approach to the orbital floor and maxilla in congenitalmalformations and trauma”. Journal of Oral and Maxillofacial Surgery 1 (1973): 3-8.
- Manson PN., et al. “Single eyelid incison for exposure of the zygomatic bone and orbit reconstruction”. Plastic Reconstructive Surgery 79.1 (1987): 120-126.
Citation:
Varun Menon P., et al. “Simplified Treatment Algorithm for NOE Fracture”. Oral Health and Dentistry 1.5 (2017): 217-220.
Copyright: © 2017 Varun Menon P., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.