Case Report
Volume 1 Issue 5 - 2017
Management of Solid Ameloblastoma of the Mandibular Anterior Region
1Dr. Manjushri Waingade Reader, Deportment of Oral Medicine and Radiology,Sinhgad Dental College and Hospital, S.No: 44/1, Vadgaon (Bk)., Pune – 411041, Maharashtra, India
2Dr. Amit Mhapuskar, Professor, Deportment of Oral Medicine and Radiology, Bharati Vidyapeeth Deemed University Dental College and Hospital, Pune-Satara Road, Katraj, Dhankawadi, Pune - 411043 Maharashtra, India
3Dr. (Mrs). Madhavi A Mhapuskar, Lecturer, Deportment of Prosthodontics, Sinhgad Dental College and Hospital, S. No: 44/1, Vadgaon (Bk)., Pune – 411041, Maharashtra, India
2Dr. Amit Mhapuskar, Professor, Deportment of Oral Medicine and Radiology, Bharati Vidyapeeth Deemed University Dental College and Hospital, Pune-Satara Road, Katraj, Dhankawadi, Pune - 411043 Maharashtra, India
3Dr. (Mrs). Madhavi A Mhapuskar, Lecturer, Deportment of Prosthodontics, Sinhgad Dental College and Hospital, S. No: 44/1, Vadgaon (Bk)., Pune – 411041, Maharashtra, India
*Corresponding Author: Manjushri Waingade, Reader, Deportment of Oral Medicine and Radiology, Sinhgad Dental College and Hospital, No: 44/1, Vadgaon (Bk), Pune – 411041, Maharashtra, India.
Received: September 18, 2017; Published: September 25, 2017
Abstract
Ameloblastoma is a true neoplasm of odontogenic origin. It is the second most common intraosseous benign odontogenic tumor after odontome. Ameloblastoma may pose a diagnostic challenge to the clinician especially if it occurs in rare location. The authors present a case of follicular ameloblastoma involving the mandibular anterior region in a 22-year male patient with emphasis on the management of the lesion.
Keywords: Ameloblastoma; Odontogenic tumor; Follicular; Solid multicystic
Introduction
Ameloblastoma is an uncommon, locally invasive odontogenic neoplasm arising in the jaw characterized by slow growth that can reach an enormous size to cause facial disfigurement and functional impairment. [1,2] It is very aptly described by Robinson as a benign tumor that is “usually unicentric, non-functional, intermittent in nature, anatomically benign and clinically persistent.” [3]
Global incidence is 0. 6 cases per million with variable geographic prevalence, most common in China and Africa, followed by the United States and Canada (odontoma being most common). African Americans have an overall fivefold increased risk of disease as compared to Caucasians. [4-8]
Ameloblastoma is thought to arise from cells of the dental lamina and resembles structures of the cap/bell stage of the developing tooth. In the 2005 World Health Organization (WHO) classification, ameloblastomas include four subtypes based on location and histopathology: solid/multicytic (91%), unicystic (6%), extra-osseous (2%), and desmoplastic (1%). [1,5]
The solid or multicystic variant involves 92% of all ameloblastomas and shows a greater propensity to infiltrate the surrounding tissues with higher recurrence rate and represent a challenging group of tumours to treat, in terms of achieving adequate excision and restoring oral function. [2,9,10]
This paper aims to report a case of a large solid multicystic ameloblastoma in a 22-year-old male in the mandibular anterior region who was successfully treated using surgical resection of the mandible with immediate bone grafting for reconstruction of the mandibular defect.
Case Report
A male patient aged 22 years reported with a chief complaint of swelling in the mandibular anterior region since 6 months. The swelling initially started as a small nodule and gradually increased to the present size. Patient gave history of extraction 2 years back due to mobility of 31, 32 and 41. The patient’s medical and family history and review of systems were unremarkable. Extraoral examination revealed facial asymmetry due to swelling extending from right to left parasymphyseal region crossing the midline measuring approximately 5x7 cm with ovoid shape. The skin over the swelling appeared normal. (Figure 1 and 2) On palpation, the swelling was firm, non-tender with no elevation of temperature. There was no pain, paresthesia or lymphadenopathy associated with the swelling.
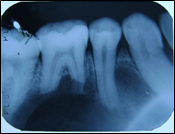
Intraoral examination (Figure 3) revealed a large mass extending from right mandibular canine to left canine region measuring approximately 6x6 cm with the overlying surface showing indentations of the opposing teeth with ulceration associated. The lesion appeared bluish on the lateral aspect while the rest of the mass appeared reddish. On palpation, the mass was firm but fluctuant at some parts. The labial vestibule from 33 to 43 appeared to be obliterated. 42 was displaced superiorly and labially while 34, 35, 36,44,45,46 were mobile. The pulp vitality reveled non-vital 33,34,35,36,42,43,44,45,46,47.
On the basis of clinical examination, a diagnosis of a benign tumor most probably a central giant cell granuloma was given. Intraoral periapical radiograph (Figure 4,5) revealed knife edge root resorption with 33,34,35,36,37,43,44,45,46. Occlusal radiograph (Figure 6) revealed a multilocular radiolucency with septa showing a soap bubble appearance associated with bicortical plate expansion with marked scalloping of the peripheral (buccal) border.
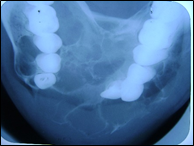
Figure 6: Occlusal radiograph showing buccal and lingual expansion with “soap bubble” internal structure.
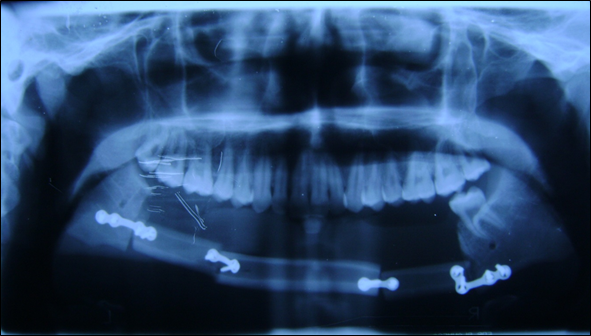
Orthopantomograph (Figure 7) showed a well- defined multilocular radiolucency extending from 37 to 47 antero-posteriorly and supero-inferiorly from alveolar ridge descending down expanding the lower border of mandible crossing the midline. Postero-anterior view (Figure 8) showed a multilocular radiolucency with “soap bubble” appearance in the midline of mandible.
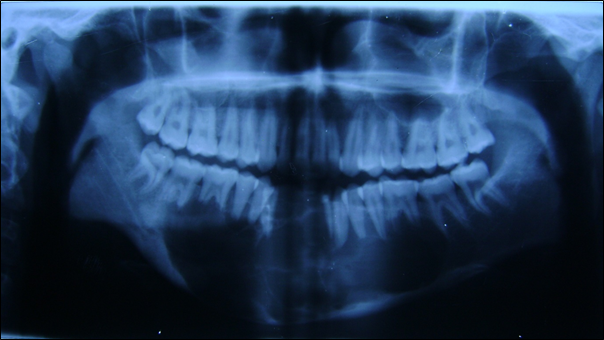
Figure 7: Orthopantomograph showing “soap bubble” appearance
of lesion in the mandibular anterior region.

Figure 8: Postero-anterior view showing multilocular
radiolucency in the mandibular anterior region.
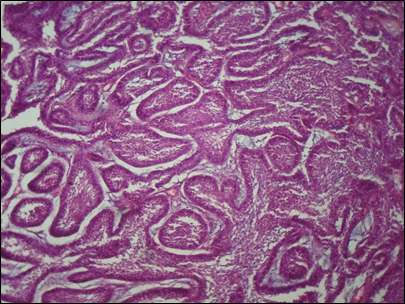
Incisional biopsy (Figure 9) revealed fibrous connective tissue with islands of odontogenic epithelium. Epithelial islands showed peripheral tall columnar cells. Nucleus showed reverse polarity. Cytoplasm towards basement membrane showed vacuolization. Central stellate reticulum like cells undergoing squamous metaplasia in some islands giving a histopathological diagnosis of Follicular Ameloblastoma.
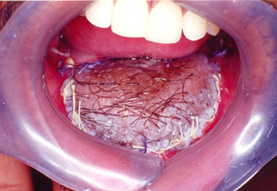
The management of the lesion included partial resection of mandible under general anesthesia performed with a clear margin of approximately 1 cm at each side of the tumor.
Immediately following resection, reconstruction (Figure 10) was done using screws at each side of defect and fibula was used for filling the defect.
The patient was followed up (Figure 11,12) for 2 years and remained clinically and radiographically disease free.
Discussion
Ameloblastoma represents 1% of all tumors and cysts that involve the jaws and about 10% of all odontogenic tumors. [1,11,12]
It often presents as asymptomatic slow growing, painless facial swelling, causing expansion of the cortical bone, perforation of the lingual and or buccal plates and infiltration of soft tissue. There is often delay in the diagnosis because of its slow-growing nature. [1,3,12] The average age at the diagnosis is 33 to 39 years and most patients ranged between ages 20 and 60 years with no gender predilection. Ameloblastoma can occur at any location but about 80% of the tumors occur in the mandibular molar and ramus region and the remaining 20% occur in maxilla. [1,3,11] This case presented describes the unique location of solid multicystic ameloblastoma in a male patient aged 22 years in the mandibular anterior region.
Radiological investigations provide a useful aid to diagnosis. However, these findings are not pathognomonic and must therefore be confirmed with histological examination. [2] The radiographic differential diagnosis includes a variety of odontogenic cysts and tumors, particularly the keratocystic odontogenic tumor, central giant cell lesion, fibro-osseous lesions, simple bone cyst, aneurysmal bone cyst, ameloblastic fibroma, odontogenic myxoma, and brown tumor of hyperparathyroidism. [7,8] In the present case due to rare location of the tumor, the diagnosis of ameloblastoma was confirmed only by histopathology.
Ameloblastoma occur in distinct clinical and radiographic situations, which need to be considered separately due to therapeutic and prognostic differences. The histologic distinction is important because the treatment for a unicystic lesion can be more conservative due to its less aggressive behavior and usually smaller size than the solid or multicystic variation. [2,7,8,11]
The best form of treatment has been controversial since years. The spectrum of treatment ranges from simple bone curettage to segmental resection also including marsupialization, cryosurgery, electrocautery, sclerotherapy and radiotherapy, but classically, solid ameloblastomas are treated, in most cases, by radical surgical excision with 1-2 cm safety margin beyond the limits of radiographic lesion. [5,10]
Since the mandible holds an important place in function and aesthetics, loss of mandibular continuity, whether caused by tumour resection, produces significant functional disability and cosmetic deformity. [9] Reconstruction of large mandibular defects represents a challenge. Among different methods, microvascular surgery is the preferred option. Four donor sites i.e., fibula, iliac crest, radial forearm, and scapula provide primary sources of vascularized bone and soft tissue. Fibula should be considered as a choice in reconstruction since it has multiple advantages including bone length and thickness, donor site location permitting flap harvest simultaneously with tumor resection and minimal donor site morbidity, as followed in present case. [6]
Th recurrence rate is 55 to 90% for all ameloblastomas treated conservatively (enucleation and curettage). [8,9,10] However, the incidence of recurrence following radical resection is 5%. [5] The histopathological variant of an ameloblastoma is significantly associated with a recurrence. Follicular Ameloblastoma is characterized by higher recurrence rate (29.5%) compared to plexiform ameloblastoma (16.7%) and acanthomatous ameloblastoma (4.5%). [3,11,12]
Ameloblastomas are an enigmatic group of oral tumors. Radical techniques cause serious inconvenience to the patient, including masticatory dysfunction, alteration of mandibular movements, facial mutilation and deformity. Treatment should include rehabilitation, restoring the functional, anatomical and aesthetic capacity. [10]
This case report emphasizes on the importance of complete surgical resection and reconstruction. As Follicular ameloblastoma has high tendency to recur, all possible efforts must be taken to evaluate the extent of the tumor before surgery, to avoid recurrence or metastasis in future. Also, it is important to keep the patient under long term follow-up.
References
- Borgohain R., et al. “Ameloblastoma of Mandible (cystic variety): A Case Report”. Journal of Dental and Medical Sciences 14.6 (2015): 52-55.
- Ruquaya M and Singh VP. “Ameloblastoma—A Locally Destructive and Invasive Tumour Review of Literature”. International Journal of Otolaryngology and Head & Neck Surgery 3.5 (2014): 216-222.
- Deshmane S., et al. “Follicular ameloblastoma: A Case Report”. International Journal of Oral Health and Medical Research 3.4 (2016): 56-59.
- McClary AC., et al. “Ameloblastoma: a clinical review and trends in management”. European Archives of Oto-Rhino-Laryngology 273.7 (2016): 1649-1661.
- Belardo E., et al. “Mandibular ameloblastoma in a 10-year-old Child: Case Report and Review of the Literature.” International journal of odontostomatology 6.3 (2012): 331-336.
- Srivastava R., et al. “Follicular with plexiform ameloblastoma in anterior mandible report of case and literature reviews”. Indian Journal of Dentistry 4.2 (2012): 119-124.
- Hertog D., et al. “Histopathology of ameloblastoma of the jaws; some critical observations based on a 40 years single institution experience”. Medicina Oral, Patologia Oral Y Cirugia Bucal 17.1 (2012): e76-82.
- Prabhu NP., et al. “Ameloblastoma: Report of two Cases and A Brief Literature Review”. Biomedical & Pharmacology Journal 7.1 (2014): 225-230.
- Joorge-Boos FBD., et al. “Radical management of solid ameloblastoma of the mandible: Report of a case with 5-year follow-up”. Head & Neck Oncology 6.4 (2014): 31.
- Menezes JDS., et al. “Recurrence of Multicystic ameloblastoma: Case Report”. Landmark Research Journals 20.3 (2014): 355-360.
- Astekar M., et al. “Follicular ameloblastoma”. Journal of Dental Sciences and Oral Rehabilitation 6.1 (2015): 00-00.
- Kishore M., et al. “Follicular ameloblastoma: A case report”. IJSS Case Reports & Reviews 1.1 (2014): 1-3.
Citation:
Manjushri Waingade., et al. “Management of Solid Ameloblastoma of the Mandibular Anterior Region”. Oral Health and Dentistry
1.5 (2017): 221-227.
Copyright: © 2017 Manjushri Waingade., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.