Research Article
Volume 1 Issue 5 - 2017
The Safety and Effectiveness of Transoral Robotic Surgery (TORS) Comparison with Open Surgery for Head and Neck Cancer; A Systematic Review and Meta-Analysis
1Department of Nursing Science, College of Nursing, Gachon University, Incheon, Korea
2Department of Health Technology Assessment, National Evidence-based Healthcare Collaborating Agency, Seoul, Korea
3Department of Otorhinolaryngology, of Yonsei University College of Medicine, Seoul, Korea
2Department of Health Technology Assessment, National Evidence-based Healthcare Collaborating Agency, Seoul, Korea
3Department of Otorhinolaryngology, of Yonsei University College of Medicine, Seoul, Korea
*Corresponding Author: Se-Heon Kim MD, Director of Yonsei Head & Neck Cancer Center, Professor, Department of Otorhinolaryngology, Yonsei University College of Medicine, Address: 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
#Corresponding Author: Dong Ah Park, Department of Health Technology Assessment, National Evidence-based Healthcare Collaborating Agency, Address: 173Toegye-ro, Jung-gu, Seoul, Korea.
Received: September 19, 2017; Published: October 09, 2017
Abstract
Objective: The laryngopharynx is an anatomically complex structure that plays an important role in eating and breathing. Transoral robotic surgery (TORS) has recently emerged as a surgical technique for oro- and laryngopharyngeal cancer. We performed a systematic review to investigate the clinical safety and effectiveness of robotic surgery in head and neck cancer.
Methods: A literature search was conducted using the English-language databases Ovid-MEDLINE, Ovid-Embase, and the Cochrane Library, as well as domestic databases containing publications through July 2015. The outcomes included demographic characteristics, adverse events, and complications, as well as oncologic, functional, and surgical outcomes.
Results: Six papers met the inclusion criteria. Primary TORS compared with open surgery (four studies, 199 patients) was associated with lower risks of perioperative outcomes including free flap reconstruction (relative risk [RR]: 0.15, 95% confidence interval [CI]: 0.03. 0.81) and tracheostomy (RR: 0.20, 95% CI: 0.08, 0.05). Salvage TORS showed higher two-year disease-free (74% vs. 43%, p = 0.01) and overall survival rates (74% vs. 43%, p = 0.02), and lower positive-margin rates (RR: 0.32, 95% CI: 0.14, 0.73) than open surgery.
Conclusions: The findings of this systematic review suggest that TORS resulted in lower risks of free flap reconstruction and lower tracheotomy rates.
Keywords: Transoral Robotic Surgery; TORS; Meta-Analysis; Oropharynx; Hypopharynx; Larynx
Introduction (Level 1 heading)
The laryngopharynx is an anatomically complex structure that plays an important role in speaking, eating, and breathing; combined, these activities are essential for maintaining quality of life. Open surgery has been the traditional primary therapy for pharyngeal squamous cell carcinoma (PSCC). However, open surgery by mandibulotomy or mandibulectomy results in complications in 10%–60% of cases, including difficulty with speech and swallowing, malocclusion, temporomandibular joint pain, and cosmetic deformities. [1] Although pharyngotomy avoids many complications of mandibulotomy and mandibulectomy, access to nasopharyngeal lesion is significantly limited and pharyngocutaneous fistulas and severe dysphasia may develop. [1] Therefore, the main treatment of choice for pharyngeal cancers are radiation therapy and chemotherapy, rather than open surgery.
New interest in operative approaches for management of PSCC led to the introduction of transoral laser microsurgery (TLM). According to Steiner researching system, TLM was developed as a minimally invasive organ preservation surgery, with comparable medical outcomes compared with open surgery. [14]
A retrospective review of 166 patients who underwent TLM for tonsillar SCC reported an 85% five-year local control rate. [2] TLM has several limitations, including limited exposure and reduced depth perception with binocular vision, which have contributed to its limited clinical use. [3] However, the most significant weakpoint of TLM is that the laser is located outside the oral cavity, which leads to distant transoral approaches to cancerous lesions in the larynx and pharynx. In particular, the “line of sight” limitation, in which the laser is not flexible with refraction and is limited to a linear line, makes safe three-dimensional en bloc tumor resection very difficult.
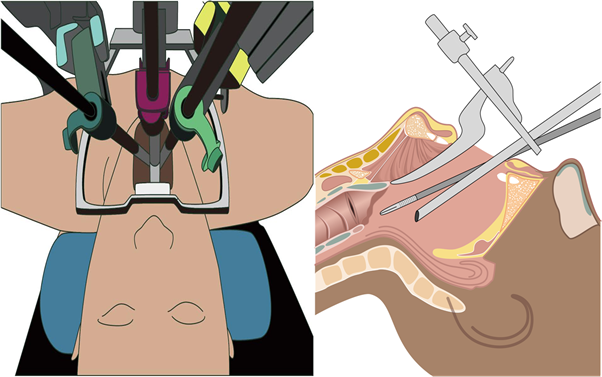
Transoral robotic surgery (TORS), first introduced in 2005, [1] offered improved visualization of the operating field and preservation of organs. TORS performed using the da Vinci Robot System (Intuitive Surgical, Inc., California, USA) has been reported to have better clinical results than open surgery. [3-4, 11-13, 15]
This method allows surgeons to overcome the limitations of oral surgery and TLM by proving three-dimensional visualization, greater than 10×visual magnification, hand-tremor stabilization, and fine control of robotic arms [9] (Figure 1). However, research and reviews comparing TORS to open surgery remain insufficient, and, to our knowledge, systematic reviews and meta-analyses comparing outcomes between TORS and open surgery have not been performed. Therefore, this study aimed to investigate the clinical safety and effectiveness of robotic surgery in oro- and laryngopharyngeal cancer to provide scientific data for the decision-making process of patients and public health workers.
Materials and Methods
Search strategy
A systematic review was conducted to assess the safety and effectiveness outcomes of robotic surgery compared to conventional surgical methods for treatment of oro- and laryngopharyngeal cancer. Studies published through July 2015 were identified by searching three international (Ovid-MEDLINE, Ovid-Embase, and the Cochrane Library) and five domestic databases (KoreaMed, KMbase, the Korean Studies Information Service System[KISS], Research Information Service System [RISS], and the Korean Institute of Science and Technology Information [KisTi]) using the terms “mouth neoplasm,” “otorhinolaryngologic neoplasms,” “oropharyn,” “pharynx,” “mouth,” “tonsil,” “palate,” “cancer,” “malignancy,” “TORS,” “transoral,” and “robot”. The search strategies were established after consultation with clinical experts to ensure the adequacy and the sensitivity of this search strategy.
A systematic review was conducted to assess the safety and effectiveness outcomes of robotic surgery compared to conventional surgical methods for treatment of oro- and laryngopharyngeal cancer. Studies published through July 2015 were identified by searching three international (Ovid-MEDLINE, Ovid-Embase, and the Cochrane Library) and five domestic databases (KoreaMed, KMbase, the Korean Studies Information Service System[KISS], Research Information Service System [RISS], and the Korean Institute of Science and Technology Information [KisTi]) using the terms “mouth neoplasm,” “otorhinolaryngologic neoplasms,” “oropharyn,” “pharynx,” “mouth,” “tonsil,” “palate,” “cancer,” “malignancy,” “TORS,” “transoral,” and “robot”. The search strategies were established after consultation with clinical experts to ensure the adequacy and the sensitivity of this search strategy.
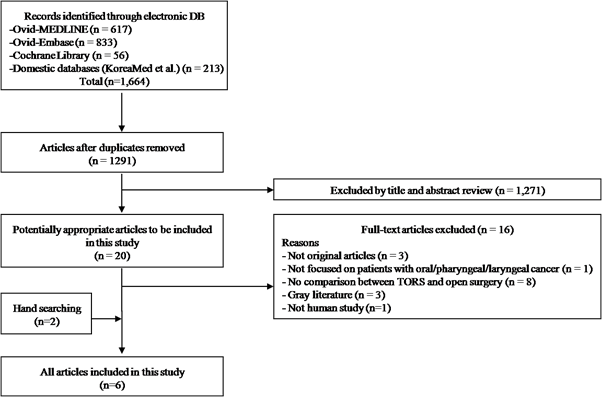
There was no language restriction, and no filters of any kind were applied. The bibliographies of relevant published articles were also reviewed to identify additional publications. After removing duplications, a total of 1,291 references were imported for initial screening based on title and abstract.
Inclusion and exclusion criteria
According to pre-determined study selection criteria, two reviewers independently screened the titles and abstracts to exclude irrelevant studies, and full-text review was subsequently performed for all potentially relevant articles. The inclusion criteria were: (1) studies that focused only on patients with pharyngeal cancer, (2) comparative studies between TORS and open surgery, and (3) studies that reported at least one proper patient outcome. Studies were excluded if they were (1) not original articles and (2) not human populations.
According to pre-determined study selection criteria, two reviewers independently screened the titles and abstracts to exclude irrelevant studies, and full-text review was subsequently performed for all potentially relevant articles. The inclusion criteria were: (1) studies that focused only on patients with pharyngeal cancer, (2) comparative studies between TORS and open surgery, and (3) studies that reported at least one proper patient outcome. Studies were excluded if they were (1) not original articles and (2) not human populations.
Data extraction and quality assessment
The reviewers extracted the following variables to a data extraction form and double-checked all entries. Disagreements between reviewers were discussed and resolved by consensus. An assessment for risk of bias in the selected studies was performed using Risk of Bias for Nonrandomized Studies (RoBANS) version 2.0.
The reviewers extracted the following variables to a data extraction form and double-checked all entries. Disagreements between reviewers were discussed and resolved by consensus. An assessment for risk of bias in the selected studies was performed using Risk of Bias for Nonrandomized Studies (RoBANS) version 2.0.
The data included rates of adverse events and complications, survival, positive resection margins, free flap reconstruction, and tracheostomy as well as time to decannulation, length of hospital stay (LOS), and operation time. These data were used to compare the effectiveness of TORS and open surgery.
Statistical analysis
Relative risks (RRs) and weighted mean differences (WMDs) were used to assess dichotomous and continuous variables, respectively, and reported with 95% confidence intervals (CIs). The Chi square test with significance set at p < 0.10 was used to assess statistical heterogeneity among studies, including this meta-analysis, and I [2] statistics were used to quantify heterogeneity. A fixed-effect model was applied for all variables with I [2] < 50%, which was defined as in significant heterogeneity among the studies. A random-effect model was used for variables with I [2] ≥ 50%. We conducted all meta-analyses with Review Manager, version 5.3 (RevMan, Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014), with a two-tailed test of significance (p < 0.05).
Relative risks (RRs) and weighted mean differences (WMDs) were used to assess dichotomous and continuous variables, respectively, and reported with 95% confidence intervals (CIs). The Chi square test with significance set at p < 0.10 was used to assess statistical heterogeneity among studies, including this meta-analysis, and I [2] statistics were used to quantify heterogeneity. A fixed-effect model was applied for all variables with I [2] < 50%, which was defined as in significant heterogeneity among the studies. A random-effect model was used for variables with I [2] ≥ 50%. We conducted all meta-analyses with Review Manager, version 5.3 (RevMan, Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014), with a two-tailed test of significance (p < 0.05).
Results and Discussion
After abstract review, 20 articles were identified as potentially relevant for inclusion in this study. We excluded 14 of these publications because they were not original articles or did not compare TORS and open surgery. Two additional publications were identified during our manual review of relevant bibliographies; finally, a total of six publications were included in the meta-analysis (Figure 2).
Study characteristics
Table 1 shows the characteristics of the six included studies (388 patients) that reported the effectiveness of TORS compared with open surgery. Three of the six studies were conducted in Korea; the others were performed in the USA and France. All studies were published during the last five years, from 2010 to 2014. There were no randomized controlled trials (RCTs), and two of the six studies prospectively collected data. Four studies included primary cancer patients, while two studies included cases of recurrent cancer. There were significant differences in the mean patient age betw een the RT and OT groups in the six studies (Table 1).
Table 1 shows the characteristics of the six included studies (388 patients) that reported the effectiveness of TORS compared with open surgery. Three of the six studies were conducted in Korea; the others were performed in the USA and France. All studies were published during the last five years, from 2010 to 2014. There were no randomized controlled trials (RCTs), and two of the six studies prospectively collected data. Four studies included primary cancer patients, while two studies included cases of recurrent cancer. There were significant differences in the mean patient age betw een the RT and OT groups in the six studies (Table 1).
| First author, year of publication | Cancer Type | Country | Data collection | No. of patients | Clinical stage | Pathologic stage (TNM) | Sites | Age (years), mean | Gender, rate of male (%) | Follow-up (months), TORS/Open, mean or median | Type surgery, TORS/Open | |
| TORS | Open | |||||||||||
| Park, 2013a [12] | PC | Korea | Retro | 17 | 17 | T1-2 (3) 79.4% | I-II (V): 47.1% | Pharynx | 65.7 | 88.2 | 27.3 | OPG/SGLG |
| Park, 2013b [13] | PC | Korea | Retro | 30 | 26 | T1-2 (4) 69.6% | I-II (V): 25.0% | Larynx | 64.7 | 98.2 | 21.4 | HPG/PT |
| Lee, 2013 [11] | PC | Korea | Pro | 27 | 30 | T1-2 (3) 66.7% | NR | Larynx | 51.8 | 80.7 | 20.3 | OPG/TT |
| Hammoudi, 2014 [4] | PC | France | Retro | 26 | 26 | T1-2 (3) 84.6% | NR | Pharynx, Larynx | 61.5 | 69.2 | 19/56 | OPG, SGLG, PLG/ OPG, TMBPG, PLG, SGLG |
| Dean, 2010 [3] | RC | USA | Retro | 7 | 14 | T1-2 100% |
I-II (III): 66.6% | Larynx | 61.9 | 85.7 | NR | NR/NR |
| White, 2013 [15] | RC | USA | Pro | 64 | 64 | T1-2 (4) 86.7% |
I-II: 44.5% | Larynx | 61.0 | 78.9 | NR | NR/NR |
| PC: primary cancer, RC: Recurrent cancer, Retro: retrospective study, Pro: prospective study, TORS: transoral robotic surgery, Open: open surgery, NR: not reported, ND: Neck dissection, OPG: oropharyngectomy, HPG: hypopharyngectomy, SGLG: supraglotticlaryngectomy, PLG: pharyngolaryngectomy, PT: pharyngotomy, TT: Tonsillectomy | ||||||||||||
Table 1: Characteristics of the included studies.
Adverse events and complication rates
Pharyngocutaneous fistulas were reported in three studies; these three studies also reported lower risk of pharyngocutaneous fistulas with TORS compared to open surgery [4,5,9] (RR 0.24, CI: 0.05, 1.10, P = 0.07), [12-13, 15] although this trend was marginally significant. Two studies reported the rate of wound infection in TORS and open surgery, resulting in a RR of 0.34(CI 0.49, 0.77), a statistically significant difference. [3,12]
Pharyngocutaneous fistulas were reported in three studies; these three studies also reported lower risk of pharyngocutaneous fistulas with TORS compared to open surgery [4,5,9] (RR 0.24, CI: 0.05, 1.10, P = 0.07), [12-13, 15] although this trend was marginally significant. Two studies reported the rate of wound infection in TORS and open surgery, resulting in a RR of 0.34(CI 0.49, 0.77), a statistically significant difference. [3,12]
The incidences of other complications, including postoperative bleeding (RR = 0.98, 95%CI 0.40, 2.43), [13, 15] aspiration pneumonia (RR = 0.20, 95% CI: 0.01, 3.88) [12], laryngeal stenosis (RR = 3.00, 95% CI: 0.13, 68.84) [12], airway edema (RR = 1.08, 95% CI: 0.43, 2.19) [15], neck abscess (RR = 0.63, 95% CI: 0.03, 13.65) [3] and hematoma (RR = 0.38, 95% CI 0.02, 6.90) [3], did not differ significantly between the TORS and open surgery groups (Table 2, Figure 3).
| Complication | No. of Studies |
Reference Numbers |
Cancer type |
No. of events | RR | 95% CI | P value | |
| TORS (n/N) | Open (n/N) | |||||||
| Pharyngocutaneous fistula | 3 | [12-13, 15] | PC + RC | 1/111 | 7/107 | 0.24 | 0.05, 1.10 | 0.07 |
| -PC | 2 | [12,13] | 3/47 | 3/43 | 0.40 | 0.06, 2.53 | 0.18 | |
| -RC | 1 | [15] | 0/64 | 4/64 | 0.11 | 0.34, 2.27 | 0.14 | |
| Postoperative bleeding | 2 | [3,13] | PC + RC | 8/94 | 8/90 | 0.98 | 0.40, 2.43 | 0.97 |
| -PC | 1 | [12] | 1/30 | 0/26 | 2.61 | 0.11, 61.51 | 0.55 | |
| -RC | 1 | [3] | 7/64 | 8/64 | 0.88 | 0.54, 2.19 | 0.78 | |
| Wound infection | 2 | [13,15] | PC + RC | 0/24 | 3/31 | 0.36 | 0.04, 3.00 | 0.34 |
| -PC | 1 | [12] | 0/17 | 1/17 | 0.33 | 0.01, 7.65 | 0.49 | |
| -RC | 1 | [15] | 0/7 | 1/14 | 0.36 | 0.01, 2.02 | 0.77 | |
| Aspiration pneumonia | 1 | [12] | PC | 0/17 | 2/17 | 0.20 | 0.01, 3.88 | 0.29 |
| Laryngeal stenosis | 1 | [12] | PC | 1/17 | 0/17 | 3.00 | 0.13, 68.84 | 0.49 |
| Airway edema | 1 | [15] | RC | 13/64 | 12/64 | 1.08 | 0.54, 2.19 | 0.82 |
| Neck abscess | 1 | [3] | RC | 0/7 | 1/14 | 0.63 | 0.03, 13.65 | 0.77 |
| Hematoma | 1 | [3] | RC | 0/7 | 2/14 | 0.38 | 0.02, 6.90 | 0.51 |
| PC: primary cancer, RC: Recurrent cancer, TORS: transoral robotic surgery, Open: open surgery, n:number of events, N: number of patients, RR: risk ratio, CI: confidence interval, NA: not applicable | ||||||||
Table 2: Complication rates comparing Transoral robotic surgery with open surgery.
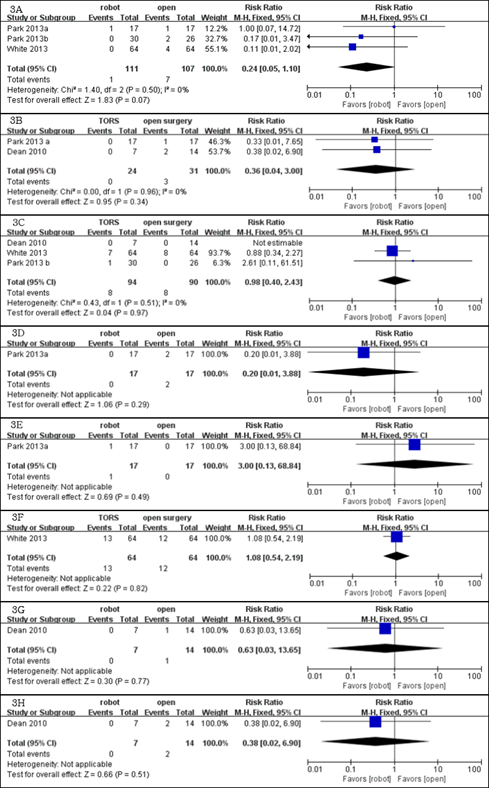
Figure 3: Meta-analysis: safety (A: Pharyngocutaneous fistula; B: Postoperative bleeding; C: Wound infection;
D: Aspiration pneumonia; E: Laryngeal stenosis; F: Airway edema; G: Neck abscess; H: Hematoma).
Survival rates and positive resection margin rates
Salvage TORS showed higher two-year disease-free (74% vs. 43%, p = 0.01) and overall survival rates (74% vs. 43%, p = 0.02) [15], as well as lower positive margin rates (RR: 0.32, 95% CI: 0.14, 0.73) compared with open surgery [3,15].
Salvage TORS showed higher two-year disease-free (74% vs. 43%, p = 0.01) and overall survival rates (74% vs. 43%, p = 0.02) [15], as well as lower positive margin rates (RR: 0.32, 95% CI: 0.14, 0.73) compared with open surgery [3,15].
Free flap reconstruction rate
Compared with open surgery, primary TORS (four studies, 165 patients) was associated with lower risks of perioperative outcomes including free flap reconstruction (RR: 0.15, 95% CI: 0.03. 0.81), and there was no significant heterogeneity between these two groups [4,11,13]. In open surgery, free flap reconstruction is required to fill in through-and-through defects or to cover the exposed carotid artery. However, in TORS, the normal structures are maximally preserved; through-and-through defects are rare, and the structures covering the carotid artery are typically preserved. Thus, the reduced requirement for free flap reconstruction is one of most significant advantages of TORS.
Compared with open surgery, primary TORS (four studies, 165 patients) was associated with lower risks of perioperative outcomes including free flap reconstruction (RR: 0.15, 95% CI: 0.03. 0.81), and there was no significant heterogeneity between these two groups [4,11,13]. In open surgery, free flap reconstruction is required to fill in through-and-through defects or to cover the exposed carotid artery. However, in TORS, the normal structures are maximally preserved; through-and-through defects are rare, and the structures covering the carotid artery are typically preserved. Thus, the reduced requirement for free flap reconstruction is one of most significant advantages of TORS.
Tracheostomy rates and times to decannulation
Primary TORS (one study, 90 patients) was associated with lower risks of tracheostomy (RR: 0.21, 95% CI: 0.08, 0.51) [4]; salvage TORS also showed a lower tracheostomy rate (RR: 0.24, 95% CI: 0.15, 0.40) [3, 15]. The time to decannulation was shorter in primary TORS by 6.4 days in concurrent studies (mean difference [MD]: -6.4 days, 95% CI -10.05, -2.81, I [2] = 78%) [11, 12].
Primary TORS (one study, 90 patients) was associated with lower risks of tracheostomy (RR: 0.21, 95% CI: 0.08, 0.51) [4]; salvage TORS also showed a lower tracheostomy rate (RR: 0.24, 95% CI: 0.15, 0.40) [3, 15]. The time to decannulation was shorter in primary TORS by 6.4 days in concurrent studies (mean difference [MD]: -6.4 days, 95% CI -10.05, -2.81, I [2] = 78%) [11, 12].
Feeding tube rates, dependence, and the duration of feeding tube use
The rates of feeding tube use at the time of surgery (RR 0.52, 95% CI 0.38, 0.72) [3,15] and feeding tube dependence six months after surgery (RR 0.27, 95% CI 0.12, 0.61) [3,15] were also lower than those rates for open surgery in patients with recurrent laryngopharyngeal cancer. The feeding tube dependence (≥ 6 months) for primary TORS was less than open surgery (RR: 0.30, 95% CI: 0.05, 1.83). [12,13] Prospective studies of TORS in primary laryngopharyngeal cancer showed significant reduction in the duration of feeding tube use (MD: -10.2 days, 95% CI: -13.40, -7.00). [11]
The rates of feeding tube use at the time of surgery (RR 0.52, 95% CI 0.38, 0.72) [3,15] and feeding tube dependence six months after surgery (RR 0.27, 95% CI 0.12, 0.61) [3,15] were also lower than those rates for open surgery in patients with recurrent laryngopharyngeal cancer. The feeding tube dependence (≥ 6 months) for primary TORS was less than open surgery (RR: 0.30, 95% CI: 0.05, 1.83). [12,13] Prospective studies of TORS in primary laryngopharyngeal cancer showed significant reduction in the duration of feeding tube use (MD: -10.2 days, 95% CI: -13.40, -7.00). [11]
Hospital stay
Three studies assessed the length of hospital stays after surgery; the pooled data showed that TORS resulted in significantly shorter hospital stays (8.5 days, MD -8.5, 95% CI -10.79, -6.11) compared to open surgery in patients with primary laryngopharyngeal cancer [4,11,12].
Three studies assessed the length of hospital stays after surgery; the pooled data showed that TORS resulted in significantly shorter hospital stays (8.5 days, MD -8.5, 95% CI -10.79, -6.11) compared to open surgery in patients with primary laryngopharyngeal cancer [4,11,12].
Operating time
Only one study reported operating time. TORS was associated with a shorter operation time of 135.9 minutes compared with open surgery (MD -135.9, 95% CI -222.39, -49.41) during treatment of primary laryngopharyngeal cancer [12] (Table 3, Figure 4).
Only one study reported operating time. TORS was associated with a shorter operation time of 135.9 minutes compared with open surgery (MD -135.9, 95% CI -222.39, -49.41) during treatment of primary laryngopharyngeal cancer [12] (Table 3, Figure 4).
| Outcomes | Variables | No. of studies |
Reference numbers |
Cancer type |
No. of events | WMD/RR | 95% CI | P value | |
| TORS (n/N) | Open (n/N) | ||||||||
| Oncologic outcomes |
Mortality | 4 | [4, 11-12] | PC | 6/100 | 7/99 | 0.81 | 0.30, 2.20 | 0.68 |
| Recurrent rate | 4 | [4, 11-12] | PC | 6/100 | 11/99 | 0.55 | 0.22, 1.40 | 0.21 | |
| Disease-free Survival rate |
5 | [4, 11-13, 15] | 137/164 | 112/163 | 1.14 | 0.94, 1.38 | 0.18 | ||
| -PC | 4 | [4, 11-13] | 90/100 | 85/99 | 1.05 | 0.96, 1.14 | 0.32 | ||
| -RC | 1 | [15] | 47/64 | 27/64 | 1/74 | 1.26, 2.40 | 0.0008 | ||
| Positive margin rate | 6 | [3-4, 11-13, 15] | 17/171 | 32/177 | 0.55 | 0.32, 0.95 | 0.03 | ||
| -PC | 4 | [4, 11-13] | 11/100 | 11/99 | 0.98 | 0.45, 2.16 | 0.96 | ||
| -RC | 2 | [3, 15] | 6/71 | 21/78 | 0.32 | 0.14, 0.73 | 0.006 | ||
| Perioperative outcomes |
Free flap reconstruction rate | 4 | [4, 11, 13, 15] | 0/147 | 15/146 | 0.12 | 0.03, 0.48 | 0.003 | |
| -PC | 3 | [4, 11, 13] | 0/83 | 8/82 | 0.15 | 0.03, 0.81 | 0.03 | ||
| -RC | 1 | [15] | 0/64 | 7/64 | 0.07 | 0.00, 1.14 | 0.06 | ||
| Tracheostomy tube rate | 3 | [3-4, 15] | 18/97 | 112/142 | 0.23 | 0.15, 0.36 | < 0.00001 | ||
| -PC | 1 | [4] | 4/26 | 48/64 | 0.21 | 0.08, 0.51 | 0.0007 | ||
| -RC | 2 | [3, 15] | 14/71 | 64/78 | 0.24 | 0.15, 0.40 | < 0.00001 | ||
| Feeding tube rate | 2 | [3, 15] | RC | 27/71 | 57/78 | 0.52 | 0.38, 0.72 | < 0.00001 | |
| Functional outcomes |
Feeding tube dependence | 4 | [3, 12-13, 15] | 7/118 | 30/121 | 0.28 | 0.13, 0.58 | 0.0007 | |
| -PC | 2 | [12, 13] | 1/47 | 4/43 | 0.30 | 0.05, 1.83 | 0.19 | ||
| -RC | 2 | [3, 15] | 6/71 | 26/78 | 0.27 | 0.12, 0.61 | 0.002 | ||
| Time to decannulation (days) | 3 | [4, 11, 12] | PC | 70 | 73 | -3.56 | -9.75, 2.62 | 0.26 | |
| Time to oral diet (days) | 2 | [4, 12] | PC | 53 | 40 | -4.19 | -16.14, 7.77 | 0.49 | |
| Others | Operative time (mins) | 1 | [12] | PC | 17 | 17 | -135.90 | -222.39, -49.41 | 0.0002 |
| Length of stay (days) | 3 | [4, 11, 12] | PC | 87 | 74 | -8.45 | -10.79, -6.11 | < 0.00001 | |
| TORS: transoral robotic surgery, Open: open surgery, n:number of events, N: number of patients, RR: risk ratio, CI: confidence interval, NA: not applicable, WMD: weighted mean difference, PC: primary cancer, RC: Recurrent cancer | |||||||||
Table 3: Other outcomes comparing Transoral robotic surgery with open surgery.
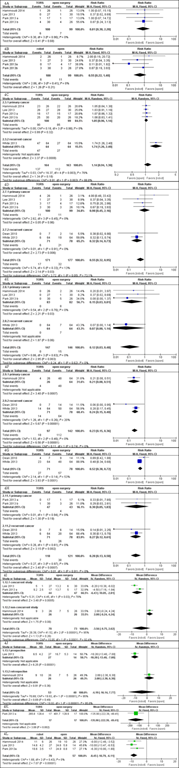
Figure 4: Meta-analysis: Effectiveness (A: Mortality; B: Recurrent rate; C: Disease-free survival rate; D: Positive
margin rate, E: Free flap reconstruction rate; F: Trachostomy tube rate; G: Feeding tube rate; H: Feeding
tube dependence; I: Time to decannulation; J: Time to oral diet; K: Operation time; L: Length of stay).
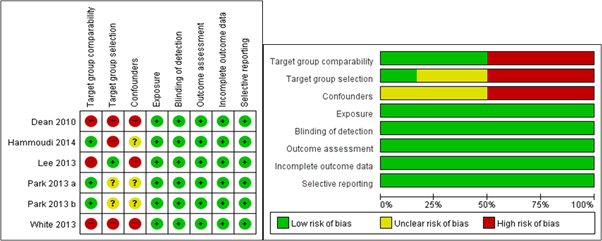
Quality appraisal
No randomized clinical trials were included in the present analysis. Investigation of methodological quality revealed that the included studies had high risk of selection bias and perturbed variables. Statistical evaluative components especially important in observational research, including comparison of two groups, selection of object groups, and correction of perturbed variables have been reported to increase the risk of bias, resulting in an overall low quality of research (Figure 5).
No randomized clinical trials were included in the present analysis. Investigation of methodological quality revealed that the included studies had high risk of selection bias and perturbed variables. Statistical evaluative components especially important in observational research, including comparison of two groups, selection of object groups, and correction of perturbed variables have been reported to increase the risk of bias, resulting in an overall low quality of research (Figure 5).
Discussion
The laryngopharynx is an anatomically complex structure that plays an important role in eating and breathing. Resection of cancerous lesions in this area by invasive open surgery could cause functional disabilities, including dysphasia and phonation problems.
Consequently, minimally invasive surgical techniques were developed, which shortened recovery periods and maximally preserved anatomical structures that minimized loss of function.
TORS was developed to supplement these short comings and has been thought to have many clinical advantages. However, due to the lack of objective comparisons, this study investigated and verified this hypothesis based on evidence reported in the literature.
This study systematically reviewed studies published since 2010 in order to compare the safety and effectiveness between TORS and conventional open surgery for treatment of patients with oro- and laryngopharyngeal cancer. Although several meta-analyses have been recently been published (Jackson., et al.; Lang., et al. Sun, Peress and Pynnonen) to our knowledge, it is the first to include the greatest number of relevant publications and compare the latest surgical results between TORS and open surgery; previous studies only compared results between TORS and radiotherapy or showed only the single effectiveness of TORS. In the present systematic review and meta-analysis of comparative studies, we found that primary TORS significantly reduced the free flap reconstruction rate, feeding tube rate, and LOS.
Salvage TORS showed higher two-year disease-free and overall survival rates and lower positive margin rates compared with open surgery.
The results of our meta-analysis showed that primary TORS reduced the risk of free flap reconstruction compared with open surgery. In open surgery, free flap reconstruction is required to fill in surgical defects or to cover the exposed carotid artery. However, in TORS, normal structures are mostly preserved, leading to rare through-and-through defects and preservation of the structures over the carotid artery. This subsequently reduces the requirement for free flap reconstruction, an important advantage of TORS that is well reported in the current meta-analysis.
The rate of positive resection margins in patients with recurrent larynx or pharynx cancer was significantly lower for TORS than for open surgery: 250 studies published after 2005 reported that resection margin-positive rates were not significantly higher than those of open surgery. In addition, the 10×magnification of the surgical view offers outstanding advantages for the evaluation of resection margins. However, well-designed prospective RCTs are necessary to corroborate this observation, as selection bias in the current study could have influenced the findings.
Our meta-analysis revealed higher two-year disease-free and overall survival rates in salvage TORS compared to rates in open surgery. [15] The first Asian study on five-year survival also showed similar results, with 5%-10% higher survival outcomes for TORS compared to those of open surgery. However, many factors may contribute to differences in survival; therefore, these results should be interpreted with caution.
The factors associated with improved survival rates include reduced suicidal rate and increased quality of life due to functional preservation of breathing, eating, and phonation. In addition, determination of appropriate treatment plans based on accurate identification tumor biology is possible with TORS. Finally, TORS offers advantages in accurately evaluating resection tissue margins, especially in anatomically complicated head and neck salvage surgeries that are more difficult than primary surgeries.
Researches on breathing and swallowing function have reported differences in functional outcomes, including the period to starting oral diets and tube removal. However, prospective and concurrent cohort studies have demonstrated the significant advantages of TORS, including the minimal functional loss compared with open surgeries.
Finally, TORS tended to have lower risks of pharyngocutaneous fistulas compared to open surgery, although the difference was marginally significant.
Two studies compared wound infection in TORS and open surgery, reporting a statistically significant RR of 0.34 (CI 0.49, 0.77). Compared with open surgery, TORS rarely requires mandibulectomy or skin graft, which contributes to its decreased postoperative pharyngocutaneous fistula formation.
Additionally, the expanded surgical vision offered by TORS can allow protection of the carotid artery, in addition to other advantages not possible in open surgery.
Unfortunately TORS also has several limitations, including high costs and bulky equipment. In addition, individual differences between patients, such as obesity, short neck, and small jaw could make limit the surgical exposure. In these cases, excessive neck extension could cause pain, and dental injuries could result from application of the retractors. [5]
Nevertheless, TORS is a promising new surgical approach that offers minimally invasive tumor removal and functional preservation of breathing, phonation, and swallowing, factors important to human quality of life. Despite these encouraging findings, this systematic review and meta-analysis has some limitations. First, this review involved a small number of studies, including two prospective and four retrospective studies. Nevertheless, our outcomes led to statistically significant results with low heterogeneity. Second, most of the studies enrolled in this meta-analysis were not of high quality due to observational study design with insufficient controls of group comparability and confounding factors. Therefore, the results should be interpreted with caution. Third, most of the included studies were conducted in Korea (n = 3) and the USA (n = 2; thus, regional factors could have affected the results. Additional multi-national clinical trials on this topic are necessary to overcome these limitations.
Conclusion
In conclusion, the results of this meta-analysis suggest that primary TORS significantly reduces free flap reconstruction, feeding tube rates, and length of hospital stay; similarly, salvage TORS significantly lowered the positive margin rates compared to conventional open surgery in patients with oro- and laryngopharyngeal cancer. However, there was not enough evidence to draw a definite conclusion regarding safety and effectiveness between TORS and open surgery. TORS is a promising technique for larynx and pharynx cancer, but well-designed prospective studies are required to clearly elucidate the clinical effects of robotic surgery.
References
- Jackson NR., et al. "Safety of Robotic Thyroidectomy Approaches: Meta-Analysis and Systematic Review." Head & Neck36.1 (2014): 137-143.
- Lang BH., et al. "A Systematic Review and Meta-Analysis Comparing Surgically-Related Complications between Robotic-Assisted Thyroidectomy and Conventional Open Thyroidectomy." Annals of Surgical Oncology21.3 (2014): 850-861.
- Sun GH., et al. "Systematic Review and Meta-Analysis of Robotic Vs Conventional Thyroidectomy Approaches for Thyroid Disease." Otolaryngology - Head & Neck Surgery150.4 (2014): 520-532.
- Almeida JR., et al. “A systematic review of transoral robotic surgery and radiotherapy for early oropharynx cancer: a systematic review”. The Laryngoscope 124.9 (2014): 2096-2102.
- Clayburgh DR and Gross N. “Surgical Innovations”. Otolaryngologic Clinics of North America 46.4 (2013): 615-628.
- Dean NR., et al. “Robotic-assisted surgery for primary or recurrent oropharyngeal carcinoma”. Archives of Otolaryngology--Head & Neck Surgery 136.4 (2010): 380-384.
- Hammoudi K., et al. “Transoral robotic surgery versus conventional surgery in treatment for squamous cell carcinoma of the upper aerodigestive tract”. Head Neck 37.9 (2014): 1304-1309.
- Hockstein NG., et al. “Assessment of intraoperative safety in transoral robotic surgery”. The Laryngoscope 116.2 (2006): 165-168.
- Holsinger FC., et al. “Transoral lateral oropharyngectomy for squamous cell carcinoma of the tonsillar region: I. Technique, complications, and functional results”. Archives of Otolaryngology–Head & Neck Surgery 131.7 (2005): 583-591.
- Howard J., et al. “Minimally invasive surgery versus radiotherapy/chemoradiotherapy for early‐stage oropharyngeal carcinoma”. The Cochrane Database of Systematic Reviews (2016).
- Hutcheson KA., et al. “Functional outcomes after TORS for oropharyngeal cancer: a systematic review”. European Archives of Oto-Rhino-Laryngology 272.2 (2015): 463-471.
- Kelly K., et al. “Oncologic, functional and surgical outcomes of primary Transoral Robotic Surgery for early squamous cell cancer of the oropharynx: a systematic review”. Oral Oncology 50.8 (2014): 696-703.
- Lawson G., et al. “Transoral robotic surgery for the management of head and neck tumors: learning curve”. European Archives of Oto-Rhino-Laryngology 268.12 (2011): 1795-1801.
- Lee SY., et al. “Comparison of oncologic and functional outcomes after transoral robotic lateral oropharyngectomy versus conventional surgery for T1-T3 tonsillar cancer”. Head & Neck 36.8 (2013).
- Park YM., et al. “Comparison of treatment outcomes after transoral robotic surgery and supraglottic partial laryngectomy: our experience with seventeen and seventeen patients respectively”. Clinical Otolaryngology (2013): 270-274.
- Park YM., et al. “Comparison study of transoral robotic surgery and radical open surgery for hypopharyngeal cancer”. Acta Oto-Laryngologica 133.6 (2013): 641-648.
- Steiner W., et al. “Transoral laser microsurgery for squamous cell carcinoma of the base of the tongue”. Archives of Otolaryngology–Head & Neck Surgery 129.1 (2003): 36-43.
- White H., et al. “Salvage surgery for recurrent cancers of the oropharynx: comparing TORS with standard open surgical approaches”. JAMA Otolaryngology – Head & Neck Surgery 139.8 (2013): 773-778.
Citation:
Se-Heon Kim., et al. “The Safety and Effectiveness of Transoral Robotic Surgery (TORS) Comparison with Open Surgery for
Head and Neck Cancer; A Systematic Review and Meta-Analysis”. Oral Health and Dentistry 1.5 (2017): 245-257.
Copyright: © 2017 Se-Heon Kim., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.