Research Article
Volume 1 Issue 1 - 2016
Repair of Periapical lesions Using a Combination of Hydroxyapatite and Calcium Hydroxide
1Clinical Professor of Stomatology Bauta, Artemisa. Cuba
2Researcher at Biomaterials Center. University of Havana
2Researcher at Biomaterials Center. University of Havana
*Corresponding Author: Amisel Almirall La Serna, Researcher at Biomaterials Center, University of Havana, Cuba.
Received: July 12, 2016; Published: October 16, 2016
Summary
Nowadays physicians are searching for new methods to treat perialpical lesions by minimal access to prevent extensive surgeries. The aim of this study was to evaluate the apical repair using the combination of hydroxyapatite and calcium hydroxide, after the extraction of the liquid content from the lesion, procedure that was carried out intracanal way. An experimental interventional study was conducted to determine the apical repair using a different method from the conventional endodontic. In this study the extraction of periapical lesion content was carried out through the root canal after the biomechanical preparation of the canal. A combination of Apafill‑G® and calcium hydroxide as medication between sessions was used. A sample of 12 patients with periapical lesions according to diagnostic criteria, inclusion, exclusion and ethical parameters, was used. All patients signed the informed consent. The lesions were classified as large, medium and small size lesions; and were evaluated at different times (7, 15, 30, 120 and 350 days). The main variable was bone repair, with the clinical response and adverse events as secondary variables.
The results showed that patients presented mostly large lesions. In reference to radiological response, 91.7% of the patients were successfully treated; a similar final clinical outcome was achieved.
In different periods of monitoring, the absence of adverse events and a gradual decrease in symptomatology (pain on palpation, percussion and infection) were shown.
As a conclusion, a mixture of granulated hydroxyapatite (Apafill-G®) with calcium hydroxide, applied as intracanal medication has been successfully used to treat bone defects in periapical endodontic procedures.
Introduction
Biomaterials are substances or combinations of substances of synthetic or natural origin, which are used for any period of time, as all or part of a system that increases, or replace any tissue, organ or function of the body; these materials must meet the following requirements: to be functional, biocompatible and sterilizable [1,2].
Biomaterials based on hydroxyapatites (HA) are able to mimic the properties of natural tissues in their biological environment. The HA is the main inorganic bone component in vertebrates. It is also found in dentin and tooth enamel. This calcium phosphate, when produced synthetically, has characteristics and properties, which allow its use in various dental procedures to repair bone and dental tissues [3-7].
Another important aspect of these biomaterials is the percentage of degradation because it may change according to various physico-chemical and biological parameters. For example, compounds of β- tricalcium phosphate materials (β-TCP) degrade faster than HA, which shows minimal degradation at physiological pH. For maxillofacial Guided Bone Tissue Regeneration (GBTR) the degradation of biomaterials is a common property [8-11] but in the repair of periapical defects, a more stable material is required to achieve a positive response.
Another calcium compound widely used in the dental field is calcium hydroxide [Ca(OH)2] which has been employed in endodontics in a large number of procedures, such as medication between sessions during the root canal treatment, as irrigating solution, in the treatment of resorptions, as cement sealer, in the repair of perforations, pulp capping, apexification and apexogenesis [12]. One of its functions is to act as medication between sessions during the root canal treatment in teeth with periapical lesions in order to reduce bacteria, besides the appropriate instrumentation to prepare the conduct. This product is used because there are areas that are unreachable by the instruments or irrigation solutions, such as dentinal tubules and branches of the duct system [13,14].
The periapical lesions are caused mainly by destruction or necrosis of the pulp, which extends along the duct and pierces the foramen at the apical region, when it is not treated on time or properly. These are the most frequently pathologies developed in the apical bone. However, the possibility that periodontal diseases cause pulp necrosis directly has also been discussed for several decades with different opinions [15-23].
Some apical conditions often do not receive proper attention, since they may develop asymptomatically, causing periapical lesions within the cysts. The major incidence of this lesion occur in the jawbone and odontogenic cyst, formed by the hydropic degeneration of epithelial remains of Malassez as a result of stimulation of non-vital teeth. The differentiation between periapical cyst and granuloma from the histologic point of view has little importance in the treatment [22,23]
Conventional endodontic treatments for this condition have been constantly changing, they have gone from the root canal treatment in one appointment (very controversial in recent years), endodontic on several sections and periods of medication, to Periapical surgery [24]. The endodontic treatment has gone through many trends during surgery, from periods of almost non surgery, and then back to the surgical options, with pre-surgical or trans-surgical endodontic [25, 26].
Of the techniques mentioned, the most currently used in necrotic teeth with periapical lesions is the treatment during several appointments to reduce the spread and proliferation of bacteria around the root canal system. This technique includes the application of calcium hydroxide paste as medication between appointments, sometimes combined with different antimicrobial active substances to control infection and thus promote the periapical repair [15, 27-33].
Based on some reports on the treatment of periapical lesions and as results of previous experience, a mixture of HA and calcium hydroxide has been used after conventional endodontics for bone repair in periapical lesions with circumscribed bone loss. The treatment proposed is to remove the internal content of the lesion by root canal via and then apply intracanal medication between sessions with a mixture of calcium hydroxide and hydroxyapatite.
In Cuba there is a synthetic biomaterial for bone and tooth repair based on HA named Apafill-G®, develop by the Biomaterial Centre of the University of Havana, which has shown satisfactory results, reported in the literature. A calcium hydroxide paste (Hydrocal) manufactured by the company Leduc, Montevideo, Uruguay Oriental Republic is also used [34,35].
The general objective of this work was to evaluate the clinical and radiographic response in bone repair of periapical osteolytic lesions, using the combination of calcium hydroxide and hydroxyapatite as medication between sessions, where the content of the lesion was previously extracted by Intracanal via.
Materials and Methods
The material used was a combination of hydroxyapatite granulates Apafill-G® and calcium hydroxide Hydrocal. The Apafill-G® is a dense synthetic ceramic granule, prepared and supplied by the Biomaterial Centre (BIOMAT), University of Havana, Cuba, and the particle size used was less than 0.1 mm. Calcium hydroxide corresponded to a smooth paste called Hydrocal (LEDUC, Montevideo, Uruguay).
The universe of the research consisted in all patients attending consultations in Bauta Endodontics Dental Teaching Clinic, during the period from January 2014 to July 2015. The sample was defined by the principles of non-probability intentional sample, consisting of 12 patients that did not evolve properly to conventional root canal treatment. Patients were evaluated employing the combination of hydroxyapatite granulates Apafill-G® and calcium hydroxide Hydrocal, with removal of the injury content by intracanal via.
All patients fulfilled the diagnostic criteria corresponding to devitalized teeth with periapical osteolytic lesions visualized by X-ray, not solved by conventional endodontic treatment. Inclusion criteria for the study were: a range of age between 18 and 50 years, of both sexes, Cuban citizens, regardless of race, who gave their consent in writing to participate, following the principles of Helsinki and the principles of bioethics for clinical investigations [36,37].
Patients under 18 and over 60 years of age, with decompensated diabetics or difficult to control it, immunosuppressed or under immunosuppressive therapy, mental retardation, malignancies diagnosed in any part of the body and pregnant women were excluded, as well as patients who refused to be included. For diagnosis, primary periapical x-ray was taken and scored in Notebook Data Collection (NDC), and the following symptoms and signs were considered: pain in vertical and horizontal percussion, intra and extra oral palpation, fistula and the presence of spontaneous pain.
Treatment
The treatment applied consisted in the use of a combination of granulated hydroxyapatite Apafill-G® and calcium hydroxide Hydrocal, after extraction of the contents of the injury by intracanal via followed by the already known steps of endodontic treatment. The neutralization of the pathological content was performed by washing with EDTA (Ethylene-diamine-tetraacetic acid), which allowed the used of x-ray conductometry to determine the exact dimensions of the conduit and its form, and the biomechanical preparation of the root canal (PBM) with the removal of all the affected content. After that, a hypodermic syringe was used to perform the Conductometry and the aspiration of apical bone in the injury area (Figures1 and 2).
The treatment applied consisted in the use of a combination of granulated hydroxyapatite Apafill-G® and calcium hydroxide Hydrocal, after extraction of the contents of the injury by intracanal via followed by the already known steps of endodontic treatment. The neutralization of the pathological content was performed by washing with EDTA (Ethylene-diamine-tetraacetic acid), which allowed the used of x-ray conductometry to determine the exact dimensions of the conduit and its form, and the biomechanical preparation of the root canal (PBM) with the removal of all the affected content. After that, a hypodermic syringe was used to perform the Conductometry and the aspiration of apical bone in the injury area (Figures1 and 2).
Developments in the above periods were classified as:
Clinical response.
Good: When during the clinical evaluation the signs and symptoms decreased compared to the previous evaluation.
Bad: When the clinical evaluation reflects the permanence or increase of the signs and symptoms present in the previous evaluation.
Radiographic response.
Good: When the radiographic evaluation shows an increased radiopacity compared to the previous radiograph.
Bad: When the radiographic evaluation shows a decreased radiopacity compared to the previous radiograph.
Clinical response.
Good: When during the clinical evaluation the signs and symptoms decreased compared to the previous evaluation.
Bad: When the clinical evaluation reflects the permanence or increase of the signs and symptoms present in the previous evaluation.
Radiographic response.
Good: When the radiographic evaluation shows an increased radiopacity compared to the previous radiograph.
Bad: When the radiographic evaluation shows a decreased radiopacity compared to the previous radiograph.
The final evaluation to measure the effectiveness and safety was made after a year and classified as:
Success: When after a year of treatment, radiopaque bone density was 70% or more and the secondary variable was not present.
Failure: When after a year of treatment, radiopaque bone density was less than 70% and more than two secondary variables were present.
Success: When after a year of treatment, radiopaque bone density was 70% or more and the secondary variable was not present.
Failure: When after a year of treatment, radiopaque bone density was less than 70% and more than two secondary variables were present.
If the final evaluation was successful, the treatment was completed with the seal using the conventional treatment with gutta-percha standardized cones and free cement eugenol. Clinical and radiographic rechecking were indicated to the patients on annual basis for 5 years, precise indications about the care after the completion of the treatment were also given.
Results and Discussion
The results obtained regarding the size of the lesion in the studied ages (Table 1) show that from 18 to 35 large lesions predominate, representing the 50%; in ages from 36 to 60, injuries are equally distributed, each one representing the 33.3%. Mostly the patients with medium and large lesions were selected for this treatment because the small lesions have better response to conventional endodontic treatments. Some studies do not considere as relevant the influence of age in the size of the lesion, but it was reported as an important factor for the success or failure of treatment [22].
| Age | Type of injury | Total | ||||||
| Small | % | Medium | % | Large | % | No | % | |
| 18-35 | 1 | 16,7 | 2 | 33,3 | 3 | 50 | 6 | 50 |
| 36-60 | 2 | 33,3 | 2 | 33,3 | 2 | 33,3 | 6 | 50 |
| Total | 3 | 25 | 4 | 33,3 | 5 | 41,7 | 12 | 100 |
Table 1: Size distribution of the lesion studied in relation to age.
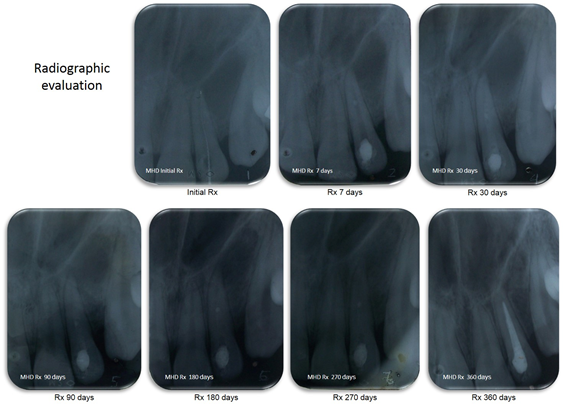
Table 2 shows the frequency (%) of clinical symptoms observed in the six periods of monitoring (7, 30, 90, 180, 270 and 360 days) where the results show the reduction of symptomatology in time. At seven days, the symptomatology remained similar to the beginning of treatment. It is possible that a clinical healing response at that time has not yet taken place, also the intervention itself causes slight attack on tissue. However, after thirty days, there were more pronounced reduction of the tenderness, percussion pain and infection. Only 8.34% of the sample (one patient) remained with negative symptoms after treatment; the cause of failure was considered to be the bulging of the palatal injury, which prevented the completely remove of the liquid contained inside the periapical lesion, which then was pus. In addition, the arrival of antiseptics into the infested area should be difficult [22]. Regarding the improvement observed in the radiograph, it is not possible to observe it until ninety days when radiopacity begins to appear.
| Clinical Symptoms | Frequency (%) | |||||
| 7 days | 30 days | 90 days | 180 days | 270 days | 360 days | |
| Inflammation | 8,34 | - | - | - | - | - |
| Infection | 41,7 | 34,34 | 8,34 | 8,34 | 8,34 | 8,34 |
| palpation | 58,34 | 33,34 | 8,34 | 8,34 | 8,34 | 8,34 |
| Percussion | 58,34 | 33,34 | 8,34 | 8,34 | 8,34 | 8,34 |
| Fistula | 16,68 | 16,68 | 8,34 | 8,34 | 8,34 | 8,34 |
| Radiographic Appearance | Frequency (%) | |||||
| 7 days | 30 days | 90 days | 180 days | 270 days | 360 days | |
| Good | - | - | 83,32 | 91,66 | 91,66 | 91,66 |
| Bad | 100 | 100 | 16,68 | 8,34 | 8,34 | 8,34 |
Table 2: Frequency (%) of clinical symptoms and radiographic appearance during the follow-up.
Altare also considered important the clinical and radiographic control on periapical diseases over time, as it provides data on the evolution or involution of the lesion [38]. Koch also states that the goal of endodontics is to perform treatments that truly meet all the biological objectives, while preserving and even improving the integrity of the natural tooth. The purpose of this procedure should not only solve the endodontic problem, but also improve the long-term conservation of the tooth [25].
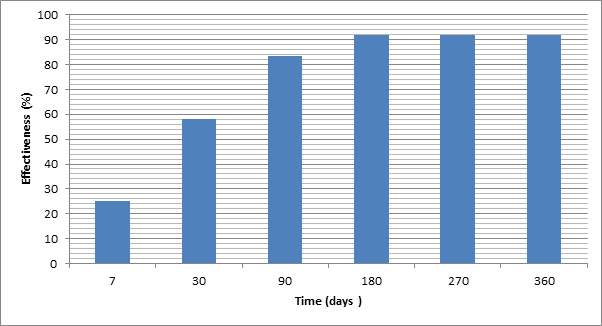
In periods up to 180 days, staggered growth was observed in both clinical and radiographic evaluation (Figure 3). At that time, it was considered that patients had a successful clinical and radiographic healing and these results remained similar for 360 days. This healing should be irreversible on time, although the cases in this study are forecasted to be followed for 5 years.
The effectiveness of treatment at 360 days is reported on Table 3 with a success rate of 91.66%, where only one patient (8.34%) did not have a positive response. This result is considered outstanding taking into account that the patients included did not respond to conventional treatments, and therefore in most of the cases tooth extraction was indicated. The clinical and radiographic failure has been due to the position of the cyst in the palate that prevented the proper evacuation of septic process, which did not allow the complete extraction of cyst content.
The importance of the treatment proposed is to avoid surgery if patients request it or when their health does not allow surgery. Authors like Velazque, agree to promote the non-surgical resolution of periapical cysts, and only use conventional endodontic treatment, which is also a valid possibility [26]. Murray states that the periradicular surgery is not always a necessary step towards the success of endodontic [39]. Vergara says that most cases of apical surgery are performed based on a radiographic diagnosis of "cystic appearance" and most of these conditions could have been solved by endodontic treatment [40].
Previous studies also show this combination of biomaterials as a successful technique as it does not present adverse events, although it has the disadvantage of requiring much time to complete the healing process [40]. Several authors agree that the treatment takes a long time due to the use of temporary filling materials, even though the success of nonsurgical treatment in periapical injuries has been proved [22]. Another concern is the need of the cooperation on the part of the patient, who should be aware of the long time required for the treatment. There are also reports that do not agree with the approach of this paper pointing out serious adverse effects observed in the use of an injectable calcium hydroxide into the root canal [41]. Another study argues that the calcium hydroxide only has limited effectiveness in eliminating bacteria from the root, when evaluated by in vitro techniques [42].
The success of the procedure can also be granted to the benefits of HA, since different authors have observed mineralization of hard tissues in contact with this biomaterial. This has been verified by Jimenez in a study of extracted teeth in orthodontics, which pose the remineralization of the tooth surface in contact with hydroxyapatite [43]. Koch also believes that the hydroxyapatite establishes an important chemical bond with the duct wall [25].
Age |
Final effectiveness of treatment | |||
| Success | % | Failure | % | |
| 18-35 | 6 | 100 | 0 | 0 |
| 36-60 | 5 | 83,3 | 1 | 8,3 |
| Total | 11 | 91,7 | 1 | 8,3 |
Table 3: Clinical response at different periods.
In Figure 4 the radiographic evaluation of a successful clinical case is shown.
Conclusions
Clinical evidence and radiographic appearance of bone repair was obtained in most of the patients treated; the failure occurred in a patient who had an injury classified as large and presented a palatal bulge. The radiographic appearance at different periods of evolution of the treatment was evaluated and, at the beginning, all cases were evaluated as bad because the periapical lesion was present. It was found that after 90 days a positive change in the radiopacity began to occur, where a decrease in the pathological radiolucent area was observed in most cases (except the failed case). Clinical evaluation was bad in most cases at the beginning of the treatment, but as they were evolving symptoms began to disappear. No adverse reactions were observed in any patient, fact that helped to the completion of the treatment in all of them. A high percentage of effectiveness of treatment was obtained, which places this technique in a privileged place in the endodontic treatment.
References
- Dee KC., et al. “An introduction to tissue-biomaterial interactions: John Wiley & Sons; 2003.
- Rodríguez Moreno MdC and Fang Mercado L. “Regeneración tisular guiada para recubrimiento radicular con biomateriales dentales”. Reporte de un caso. Acta odontol venez1.51 (2013).
- Kowalyszyn K., et al. “La hidroxiapatita como biomaterial para la reconstrucción de rebordes alveolares”. Revista Venezolana de Investigación Odontológica 1.1 (2013): 62-71.
- Díaz JCQ., et al. “Resultados de 15 años empleando la Hidroxiapatita Coralina® HAP-200 como implante óseo en cirugía maxilofacial”. 15 years results of the Coralina® Hydroxyapatite HAP-200 as a bone implants in maxillofacial surgery (2010).
- Checchi V., et al. “Clinical-radiographic and histological evaluation of two hydroxyapatites in human extraction sockets: a pilot study”. International Journal of Oral and Maxillofacial Surgery40.5 (2011): 526-532.
- Velazco G and Ortiz R. “Biomateriales a base de hidroxiapatita sintética para reparación ósea”. (Reporte de un caso). 2009.
- Yang W and Ouyang XY. “Radiographic and Clinical Outcomes of Ridge Augmentation in Molar Extraction Sockets with Severe Bone Wall Defect”. The Chinese journal of dental research: the official journal of the Scientific Section of the Chinese Stomatological Association (CSA)18.4 (2015): 221.
- Sheikh Z., et al. “In vitro degradation and in vivo resorption of dicalcium phosphate cement based grafts”. Acta biomaterialia 26 (2015): 338-346.
- Pérez Alvarez M., et al. “Use of Cuban Granulated Β-Tricalcium Phosphate “Biograft-G” as Maxilar Bone Graft. Journal of Oral Hygiene & Health 1.1 (2013): 103.
- Pérez M., et al. “Respuesta biológica entre una hidroxiapatita y un betafosfato tricalcico en la regeneración de tejido óseo”. Acta Bioclínica1.2 (2011).
- Vega DS. “Principios básicos en Regeneración Ósea Guiada”. Acta Bioclínica2.3 (2012): 94-121.
- Fernandes M. “Nonsurgical management of a large periapical lesion using aspiration in combination with a triple antibiotic paste and calcium hydroxide”. Iranian endodontic journal5.4 (2010): 179.
- Amaíz A. “Hidróxido de Calcio y su aplicación en la terapéutica endodóntica”. 2006.
Mejía Arredondo G. “Reabsorción radicular. Odontólogo moderno Salud dental, medicina y humanismo para el odontólogo moderno. 2014;10(115). - Sasaki H and Stashenko P. “Interrelationship of the pulp and apical periodontitis. Seltzer and Bender’s dental pulp, second ed Chicago, IL: Quintessence Publishing2012. p. 277-99.
- Langeland K., et al. “Periodontal disease, bacteria, and pulpal histopathology”. Oral Surgery, Oral Medicine, Oral Pathology 37.2 (1974): 257-270.
- Flynn TR., et al. “Molecular methods for diagnosis of odontogenic infections”. Journal of Oral and Maxillofacial Surgery 70.8 (2012): 1854-1859.
- San Chong B., et al. “Managing endodontic failure in practice: Quintessence Publishing Company”. 2004.
- Montagner F., et al. “Molecular fingerprinting reveals the presence of unique communities associated with paired samples of root canals and acute apical abscesses”. Journal of endodontics 36.9 (2010): 1475-1479.
- Anderson AC., et al. “Comprehensive analysis of secondary dental root canal infections: a combination of culture and culture-independent approaches reveals new insights”. PloS one7.11 (2012): e49576.
- García-Rubio A., et al. “Lesiones periapicales: diagnóstico y tratamiento”. Avances en Odontoestomatología 31.1 (2015): 31-42.
- Ferro Benítez PP., et al. “Tratamiento no quirúrgico de lesiones periapicales”. Revista Cubana de Estomatología 42.2 (2005).
- Mohammad Razavi S., et al. “Periapical Lesions: a Review of Clinical, Radiographic, and Histopathologic Features”. Avicenna journal of dental research 7.1 (2015): e19435.
- Ingle JIB., et al. "Hernández LKG, Luis J. Endodoncia. 5a ed: McGraw Hill; 2004. Koch K, Brave D. Redefinir la endodoncia
- Velazque L., et al. “Enucleación de quiste periapical simultáneo a la obturación del sistema de conductos radiculares”. Revista Cubana de Estomatología 51.2 (2014): 179-186.
- Taneja S and Kumari M. “Use of triple antibiotic paste in the treatment of large periradicular lesions”. Journal of Investigative and Clinical Dentistry3.1 (2012): 72-76.
- Gomes-Filho JE., et al. “Tissue Reaction to a Triantibiotic Paste Used for Endodontic Tissue Self-regeneration of Nonvital Immature Permanent Teeth”. Journal of Endodontics38.1 (2012): 91-94.
- Vijayaraghavan R., et al. “Triple antibiotic paste in root canal therapy”. Journal of Pharmacy And Bioallied Sciences 4.6 (2012): 230-233.
- Takahashi Y., et al.“Streptococcus anginosusl-cysteine desulfhydrase gene expression is associated with abscess formation in BALB/c mice”. Molecular Oral Microbiology26.3 (2011): 221-227.
- Wagner C., et al. “Effectiveness of the Proton Pump Inhibitor Omeprazole Associated with Calcium Hydroxide as Intracanal Medication: An In Vivo Study”. Journal of Endodontics37.9 (2011): 1253-1257.
- Silva-Herzog D., et al. “Comparación del hidróxido de calcio como medicamento intraconducto, utilizando vehículos viscosos y acuosos”. Estudio in vitro. Revista de la Asociación Dental Mexicana 62.4 (2005): 137-141.
- da Silva JM., et al. “Microscopic cleanliness evaluation of the apical root canal after using calcium hydroxide mixed with chlorhexidine, propylene glycol, or antibiotic paste”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 111.2 (2011): 260-264.
- Pérez M., et al. “Eficacia y seguridad terapeutica del apafill-g™ en reparacion osea periapical mediante la vía endodontica”. Acta Bioclínica3.6 (2013): 147-162.
- Seguén Hernández J., et al. “Evolución de la periodontitis del adulto tratada con Apafill-G®”. MediSan 17.6 (2013): 970-979.
- Association WM. “Declaración de Helsinki de la AMM. Principios éticos para las investigaciones médicas en seres humanos”. Bioètica & debat: tribuna abierta del Institut Borja de Bioètica 20.73 (2014): 15-18.
- Siurana Aparisi JC. “Los principios de la bioética y el surgimiento de una bioética intercultural”. Veritas 22 (2010): 121-157.
- Altare L. “Reparación apical y periapical post tratamiento endodontico”. Electronic Journal of Endodontics Rosario 19.9 (2010): 2.
- Murray P. “Periradicular Surgery. A Concise Guide to Endodontic Procedures”. Berlin, Heidelberg: Springer Berlin Heidelberg (2015): 177-184.
- Hernández CV., et al. “Manejo clínico del quiste periapical”. Duazary7.2 (2010): 219-222.
- Olsen JJ., et al. “Nerve lesions following apical extrusion of non-setting calcium hydroxide: A systematic case review and report of two cases”. Journal of Cranio-Maxillofacial Surgery42.6 (2014): 757-762.
- Sathorn C., et al. “Antibacterial efficacy of calcium hydroxide intracanal dressing: a systematic review and meta-analysis”. International Endodontic Journal40.1 (2007): 2-10.
- Jiménez Ochoa AM. Estudio comparativo in vitro del grado de remineralización del esmalte dental con el uso de nanopartículas de hidroxiapatita en dientes extraídos con y sin brackets cementados en ellos.
Citation:
Amisel Almirall La Serna., et al. “Repair of Periapical lesions Using a Combination of Hydroxyapatite and Calcium Hydroxide”. Oral Health and Dentistry 1.1 (2016): 30-38.
Copyright: © 2016 Amisel Almirall La Serna., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.