Research Article
Volume 2 Issue 2 - 2017
Efficacy and Cost of A Selective Cyclooxygenase-2 Inhibitor Compared with A Traditional Non-Steroidal Anti-Inflammatory Drug for Pain Relief After Orthognathic Surgery: A Retrospective Single-Center Cohort Study
1Department of Oral and Maxillofacial Surgery, Showa University School of Dentistry, Japan
2Department of Pharmacy, Showa University Hospital, Japan
2Department of Pharmacy, Showa University Hospital, Japan
*Corresponding Author: Takaaki Kamatani, Department of Oral and Maxillofacial Surgery, Showa University School of Dentistry 2-1-1 Kitasenzoku, Ota, Tokyo, 145-8515, Japan.
Received: December 12, 2017; Published: December 18, 2017
Abstract
Objectives: The aim of this study was to compare the efficacy and cost of celecoxib, a selective cyclooxygenase-2 inhibitor, with that of loxoprofen, a non-selective traditional non-steroidal anti-inflammatory drug, when used for pain relief after orthognathic surgery.
Methods: We retrospectively identified patients who took celecoxib (n = 21) or loxoprofen (n = 39) for pain relief after orthognathic surgery. When the pain relief provided by celecoxib or loxoprofen was inadequate, as indicated by a visual analog scale score of ≥ 3.0, acetaminophen or diclofenac was administered for rescue analgesia.
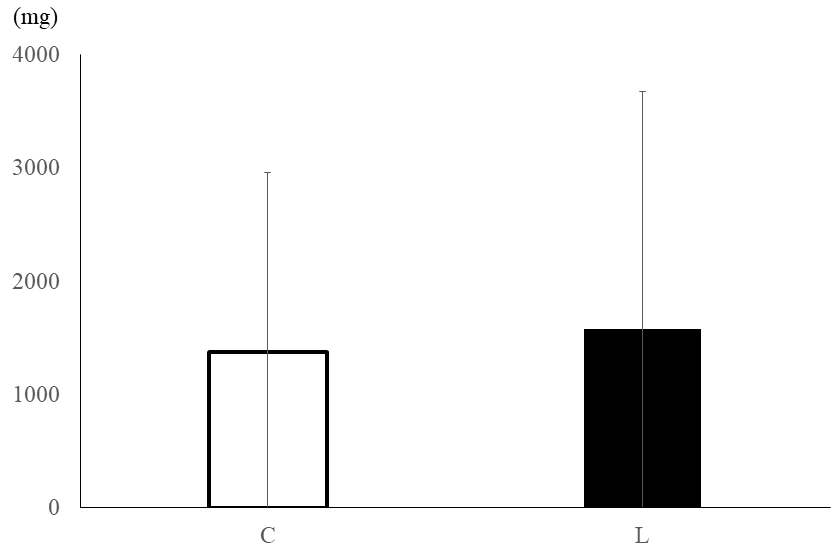
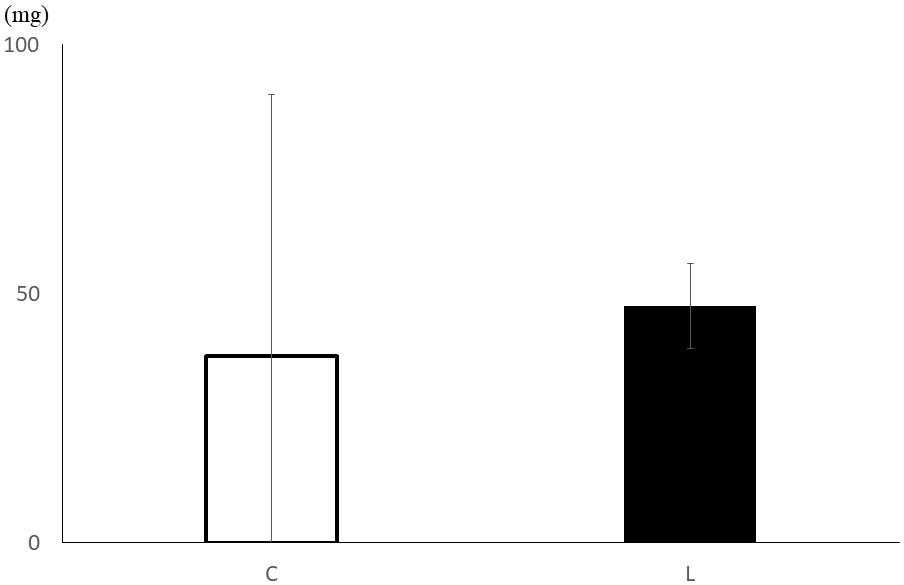
Results: The mean doses of acetaminophen and diclofenac in the celecoxib group were 1380 mg and 37.5 mg, respectively; the mean total cost of analgesia was 1008 Japanese yen and the mean duration of analgesic therapy was 5.9 days. The mean doses of acetaminophen and diclofenac in the loxoprofen group were 1580 mg and 47.5 mg, respectively; the mean total cost of analgesia was 432 Japanese yen and the mean duration of analgesic therapy was 6.3 days. The cost of celecoxib was twice that of loxoprofen.
Conclusion: There were no significant differences between the two groups with regard to doses of rescue analgesics administered or duration of analgesic therapy. Celecoxib and loxoprofen were similarly effective for pain relief after orthognathic surgery. From an economic point of view, celecoxib was not superior to loxoprofen when used for postoperative pain relief.
Key words: Celecoxib; Loxoprofen; Postoperative pain; Analgesic effect; Cost
Introduction
Non-steroidal anti-inflammatory drugs (NSAIDs) are used to treat pain after oral surgery. Traditional non-selective NSAIDs block prostaglandin synthesis by inhibiting both cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2). However, use of non-selective NSAIDs to treat postoperative pain is associated with an increased risk of bleeding at the operative site because of inhibition of platelet aggregation [1].
Selective COX-2 inhibitors have recently been introduced as an alternative to non-selective NSAIDs for postoperative pain because they have fewer adverse effects related to inhibition of platelet aggregation and are less likely to cause renal toxicity and gastric ulcers [2,3]. Although these newer drugs are more expensive than non-selective traditional NSAIDs [4], patients undergoing oral surgery have benefited from decreased postoperative pain when treated with COX-2 inhibitors [5,6]. We are not aware of any study that has compared the analgesic effectiveness of celecoxib, a selective COX-2 inhibitor, with that of non-selective traditional NSAIDs for pain after orthognathic surgery.
The aim of this study was to compare the efficacy and cost of celecoxib, a selective COX-2 inhibitor, with that of loxoprofen, a non-selective traditional NSAID, when used for pain relief after orthognathic surgery from the point of view of a rescue analgesia.
Materials and Methods
Study design
The study had a retrospective, single-center, observational cohort design. All patient data were de-identified.
The study had a retrospective, single-center, observational cohort design. All patient data were de-identified.
Patients
The study protocol was approved by the institutional ethics committee of Showa University School of Dentistry (approval number 2013-034). The medical records of 71 patients who underwent orthognathic surgery between January 2012 and December 2013 were included in the initial review. All the patients were Japanese and of Asian ethnicity. We excluded patients who received both celecoxib and loxoprofen and those who received neither of these agents. Sixty patients were deemed eligible for inclusion in the study (Table 1). The subjects were divided into two groups, i.e., those who took celecoxib at an initial dose of 400 mg, followed by a 200-mg dose at least 6 hours later, and then continued to take the drug as needed for postoperative pain as per the manufacturer’s instructions (group C) and those who took 60 mg loxoprofen as needed for postoperative pain up to 3 times per day as per the manufacturer’s instructions (group L). Both groups took acetaminophen or diclofenac as rescue analgesia if the postoperative pain relief provided by celecoxib or loxoprofen was inadequate, as indicated by a visual analog scale score ≥ 3.0. Cost estimates were calculated using the 2012 Japanese medical remuneration points system (Table 2). The outcome measure was the demand for supplementary analgesia after surgery.
The study protocol was approved by the institutional ethics committee of Showa University School of Dentistry (approval number 2013-034). The medical records of 71 patients who underwent orthognathic surgery between January 2012 and December 2013 were included in the initial review. All the patients were Japanese and of Asian ethnicity. We excluded patients who received both celecoxib and loxoprofen and those who received neither of these agents. Sixty patients were deemed eligible for inclusion in the study (Table 1). The subjects were divided into two groups, i.e., those who took celecoxib at an initial dose of 400 mg, followed by a 200-mg dose at least 6 hours later, and then continued to take the drug as needed for postoperative pain as per the manufacturer’s instructions (group C) and those who took 60 mg loxoprofen as needed for postoperative pain up to 3 times per day as per the manufacturer’s instructions (group L). Both groups took acetaminophen or diclofenac as rescue analgesia if the postoperative pain relief provided by celecoxib or loxoprofen was inadequate, as indicated by a visual analog scale score ≥ 3.0. Cost estimates were calculated using the 2012 Japanese medical remuneration points system (Table 2). The outcome measure was the demand for supplementary analgesia after surgery.
Each operation was performed by a single oral surgeon with more than 20 years of clinical experience. Lidocaine 2% containing 1:80,000 epinephrine was injected for local anesthesia under general anesthesia. The same surgical technique was used in all cases.
Statistical analysis
The non-parametric Friedman test was used to determine the significance of differences between the two groups. P-values < 0.05 were considered to be statistically significant.
The non-parametric Friedman test was used to determine the significance of differences between the two groups. P-values < 0.05 were considered to be statistically significant.
| Group | Celecoxib | Loxoprofen |
| Patients (n) | 21 | 39 |
| Sex (male/female) | 10/11 | 13/26 |
| Age (years) | 25.7 ± 8.3 | 28.2 ± 8.2 |
| Weight (kg) | 58.0 ± 10.4 | 57.2 ± 9.6 |
| Orthognathic surgery | ||
| Upper (n) | 2 | 2 |
| Lower (n) | 5 | 18 |
| Upper and lower (n) | 14 | 19 |
Table 1: Patient characteristics in the two study groups.
| Analgesic | Cost | |
| Loxonin | 60 mg | 18.6 |
| Celecox | 200 mg | 103.6 |
| Calonal | 200 mg | 8.6 |
| Voltaren suppo | 25 mg | 54.0 |
Table 2: Cost of analgesic (Yen).
Results
In group C, the mean doses of acetaminophen and diclofenac (the rescue analgesics) were 1380 mg (Figure 1) and 37.5 mg (Figure 2), respectively. The mean total analgesic cost in this group was 1008 Japanese yen and the mean duration of analgesic therapy was 5.9 days. In group L, the mean doses of acetaminophen and diclofenac were 1580 mg (Figure 1) and 47.5 mg (Figure 2), respectively. The mean total analgesic cost in this group was 432 Japanese yen and the mean duration of analgesic therapy was 6.3 days.
There was no statistically significant difference in the dose of rescue analgesics required or the mean duration of analgesic therapy between groups C and L. Celecoxib and loxoprofen had a similar analgesic effect on postoperative pain. There was a statistically significant difference in mean total analgesic cost between the two groups
Discussion
It was discovered that NSAIDs act by inhibiting COX conversion of arachidonic acid to prostaglandin in the early 1960s [7] and the COX-2 isoform was identified in the early 1990s [8]. This breakthrough ensured development of selective COX-2 inhibitors that had fewer side effects than the early NSAIDs [6]. Celecoxib was the first selective COX-2 inhibitor and was approved for use in the USA in 1998 [9]. In 2011, celecoxib was approved by the Japanese Ministry of Health, Labor and Welfare for the treatment of acute pain after dental procedures or oral surgery. Few studies have compared the efficacy of celecoxib with that of non-selective NSAIDs for pain relief after oral procedures [10].
The present study is the first clinical comparison of the effects of a selective COX-2 inhibitor on pain following orthognathic surgery with those of a non-selective traditional NSAID. We chose to compare celecoxib with loxoprofen in this study because loxoprofen is widely prescribed as a traditional non-selective NSAID in Japan [11].
The causes of postoperative pain include tissue damage at the surgical site, edema after surgery, and sensitization of the peripheral nerves [12]. Surgical trauma induces synthesis of prostaglandins that sensitize peripheral nociceptors [13,14]. NSAIDs inhibit the synthesis of prostaglandins in the periphery and in the spinal cord, thereby decreasing the postoperative hyperalgesic state [15]. For acute pain or postoperative pain, it is recommended that an initial 400-mg dose of celecoxib should be administered, followed by an additional 200-mg dose at least 6 hours later, and then further doses as needed. It is necessary to administer an initial loading dose of celecoxib because of its large volume of distribution [16] and high plasma protein binding affinity [17].
Non-selective NSAIDs have side effects in multiple organ systems, including the cardiovascular, gastrointestinal, and renal systems, and suppress platelet function because they inhibit both the COX-1 and COX-2 enzymes [18]. In contrast, selective COX-2 inhibitors inhibit the COX-1 enzyme to a minimal extent. The COX-1 enzyme is a housekeeping enzyme that helps to maintain normal cellular function. Therefore, selective COX-2 inhibitors have little or no antiplatelet activity [19]. In the present study, neither celecoxib nor loxoprofen affected the incidence of postoperative bleeding. No postoperative complications involving the gastrointestinal, renal, or cardiovascular system were observed in either study group.
The cost of celecoxib is over twice that of the traditional non-selective NSAIDs. Drug treatment is becoming more expensive because of the increased cost of introduction of new drugs [20]. COX-2-selective NSAIDs seem to be generally unattractive from a cost-effectiveness point of view. Our present findings are comparable with those observed in other cost-effectiveness analyses [21].
Acetaminophen is a good rescue analgesic that is effective for relief of moderate pain and has no anti-inflammatory activity [22]. The combination of NSAIDs and acetaminophen has been shown to be more effective than either drug alone in reducing pain following oral and otolaryngologic surgery with minimal adverse effects [23,24], which is attributed to their different sites of analgesic action [25,26]. The finding that similar total amounts of rescue analgesia were administered in groups C and L suggests that the efficacy of celecoxib is almost the same as that of loxoprofen when used for pain relief after orthognathic surgery.
Although there were no reports on adverse effects with acetaminophen [27], there are some potential disadvantages for combination using of NSAIDs and acetaminophen. One is the increasing the incidence of adverse effects of analgesia and may cause consequent adverse side effects [28]. It is important not to exceed the recommended dose of analgesia. COX-2 inhibitors is possibly increased the risk of rare but serious adverse events [29]. Using COX-2 inhibitors for postoperative pain after orthognathic surgery, duration of administration is short term. This may not be a problem for thromboembolic events
Conclusion
There was no significant difference in the doses of rescue analgesics administered or the duration of analgesic therapy between patients treated with celecoxib, a selective COX-2 inhibitor, and those treated with loxoprofen, a non-selective NSAIDs, after orthognathic surgery. From an economic point of view, a selective COX-2 inhibitor is no more useful than a non-selective NSAID for pain relief after this type of surgery.
Conflict of interest
The authors have no conflicts of interest related to this article.
The authors have no conflicts of interest related to this article.
References
- Watcha MF., et al. “Costs and effectiveness of rofecoxib, celecoxib, and acetaminophen for preventing pain after ambulatory otolaryngologic surgery”. Anesthesia & Analgesia 96.4 (2003): 987-994.
- Malmstrom K., et al. “Comparison of rofecoxib and celecoxib, two cyclooxygenase-2 inhibitors, in postoperative dental pain: a randomized, placebo- and active-comparator-controlled clinical trial”. Clinical Therapeutics 21.10 (1999): 1653-1663.
- Graff J., et al. “Effects of selective COX-2 inhibition on prostanoids and platelet physiology in young healthy volunteers”. Journal of Thrombosis and Haemostasis 5.12 (2007): 2376-2385.
- Kamath CC., et al. “The cost-effectiveness of acetaminophen, NSAIDs, and selective COX-2 inhibitors in the treatment of symptomatic knee osteoarthritis”. Value in Health 6.2 (2013): 144-157.
- Mehlisch DR., et al. “Single doses of parecoxib sodium intravenously are as effective as ketorolac in reducing pain after oral surgery”. Journal of Oral and Maxillofacial Surgery (2003): 61.9 1030-1037.
- May N., et al. “Selective COX-2 inhibitors: A review of their therapeutic potential and safety in dentistry”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 92.4 (2001): 399-405.
- Rao P and Knaus EE. “Evolution of nonsteroidal anti-inflammatory drugs (NSAIDs): cyclooxygenase (COX ) inhibition and beyond”. Journal of Pharmacy & Pharmaceutical Sciences 11.2 (2008): 81s-110s.
- Fu J., et al. “The induction and suppression of prostaglandin H2 synthase (cyclooxygenase) in human monocytes”. The Journal of Biological Chemistry 265.28 (1990): 16737-16740.
- Gillron I., et al. “Cyclooxygenase-2 inhibitors in postoperative pain management: current evidence and future directions”. Anesthesiology 99.5 (2003): 1198-1208.
- Yamashita Y., et al. “A parallel-group comparison study of celecoxib with loxoprofen sodium in third mandibular molar extraction patients”. International Journal of Oral and Maxillofacial Surgery 43.12 (2014): 1509-1513.
- Onda A., et al. “Comparison of the effects of treatment with celecoxib, loxoprofen, and acetaminophen on postoperative acute pain after arthroscopic knee surgery: A randomized, parallel-group trial”. Journal of Orthopaedic Science 21.2 (2016): 172-177.
- Yeganeh Mogadam A., et al. “Comparison of analgesic effect between gabapentin and diclofenac on post-operative pain in patients undergoing tonsillectomy”. Archives of Trauma Research 1.3 (2012): 108-111.
- Huang YM., et al. “Perioperative celecoxib administration for pain management after total knee arthroplasty – A randomized, controlled study”. BMC Musculoskeletal Disorders 9.1 (2008).
- Samad TA., et al. “Interleukin-1beta-mediated induction of Cox-2 in the CNS contributes to inflammatory pain hypersensitivity”. Nature 410.6827 (2001): 471-475.
- McCormack K. “Non-steroidal anti-inflammatory drugs and spinal nociceptive processing”. Pain 60.3 (1994): 353.
- Walter MF., et al. “Sulfone COX-2 inhibitors increase susceptibility of human LDL and plasma to oxidative modification: comparison to sulfonamide COX-2 inhibitors and NSAIDs”. Atherosclerosis 177.2 (2004): 235-243.
- Paulson SK., et al. “Plasma protein binding of celecoxib in mice, rat, rabbit, dog and human”. Biopharmaceutics & Drug Disposition 20.6 (1999): 293-299.
- Teerawattananon C., et al. “Risk of perioperative bleeding related to highly selective cyclooxygenase-2 inhibitors: A systematic review and meta-analysis”. Seminars in Arthritis and Rheumatism 46.4 (2017): 520-528.
- Leese PT., et al. “Effects of celecoxib, a novel cyclooxygenase-2 inhibitor, on platelet function in healthy adults: a randomized, controlled trial”. The Journal of Clinical Pharmacology 40.2 (2000): 124-132.
- Falagas ME., et al. “A comparative study on the cost of new antibiotics and drugs of other therapeutic categories”. PLoS One 1.1 (2006).
- Maetzel A., et al. “The cost effectiveness of rofecoxib and celecoxib in patients with osteoarthritis or rheumatoid arthritis”. Arthritis Rheum 49.3 (2003): 283-292.
- Rahimi SY., et al. “Postoperative pain management after craniotomy: Evaluation and cost analysis”. Neurosurgery 59.4 (2006): 852-857.
- Breivik EK., et al. “Combining diclofenac with acetaminophen or acetaminophen-codeine after oral surgery: a randomized, double-blind single-dose study”. Clinical Pharmacology and Therapeutics 66.6 (1999): 625-635.
- Issioui T., et al. “The efficacy of premedication with celecoxib and acetaminophen in preventing pain after otolaryngologic surgery”. Anesthesia & Analgesia 94.5 (2002): 1188-1193.
- Issioui T., et al. “Cost-efficacy of rofecoxib versus acetaminophen for preventing pain after ambulatory surgery”. Anesthesiology 97.4 (2002): 931-937.
- Kraglund F. “Acetaminophen plus a nonsteroidal anti-inflammatory drug decreases acute postoperative pain more than either drug alone”. Journal of the American Dental Association 145.9 145.9 (2014): 966-968.
- Elia N., et al. “Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials”. Anesthesiology 103.6 (2005): 1296-1304.
- Cliff KO., et al. “Combining Paracetamol (Acetaminophen) with nonsteroidal Antiinflammatory Drugs: A Qualitative Systematic Review of Analgesic Efficacy for Acute Postoperative Pain”. Anesthesia & Analgesia 110.4 (2010): 1170-1179.
- Mukherjee D., et al. “Risk of Cardiovascular Events Associated with Selective COX-2 Inhibitors”. JAMA 286.4 (2001): 954-959.
Citation:
Takaaki Kamatani., et al. “Efficacy and Cost of A Selective Cyclooxygenase-2 Inhibitor Compared with A Traditional Non-
Steroidal Anti-Inflammatory Drug for Pain Relief After Orthognathic Surgery: A Retrospective Single-Center Cohort Study”. Oral Health
and Dentistry 2.2 (2017): 362-368.
Copyright: © 2017 Takaaki Kamatani., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.