Case Report
Volume 2 Issue 3 - 2017
Osteosarcoma of Jaw: A Case Report with Unusal Presentation
1MDS Oral Pathology, Jodhpur, Rajasthan, India
2MD General Pathology
2MD General Pathology
*Corresponding Author: Priyanka Agarwal, MDS Oral Pathology, Jodhpur, Rajasthan, India.
Received: December 12, 2017; Published: December 27, 2017
Abstract
In the jaw bones, Osteo Sarcoma accounts for about 4% of all the primary malignant neoplasms. Low-grade lesions are rare and represent less than 2% of all osteosarcomas reported in the literature. This article reports on a case of a low grade osteosarcoma of the maxilla. A 30-year-old woman came with a chief complain of recurrent ossifying fibroma of the maxillae. The clinical picture showed a well-defined, pedunculated, roughly rectangular growth arising from posterior left maxillary tooth region. An excisional biopsy was performed and diagnosis of low grade osteosarcoma was established and the patient was recommended for oncologic treatment.
Key words: Osteosarcoma; Ossifying fibroma; Aggressive ossifying fibroma
Introduction
Osteosarcoma (OS) is the most common primary malignant bone tumor; however, only 5% of all cases occur in the jaws. The maxilla is less commonly affected than the mandible and in the maxilla the majority of OSs arises in the alveolar ridge and the maxillary antrum. Presenting signs and symptoms of craniofacial osteosarcoma (CFOS) include regional swelling, pain and paresthesia. In addition, unusual clinical presentation such as peri-apical lesion-like appearance has been reported.
In general, osteosarcomas of the jaw are high grade lesions. Low-grade lesions are rare and include the well differentiated intraosseous osteosarcoma (low-grade central osteosarcoma) and parosteal osteosarcomas. Low grade osteosarcoma (LOS; well-differentiated intraosseous osteosarcoma), represents less than 2% of all osteosarcomas reported in the literature [1]. Because of its rarity and well differentiation, LOS is usually misdiagnosed as a benign lesion.
The author would like to report a case of LOS of the maxilla with extremely unusual presentation in a 30 year-old woman.
Case Report
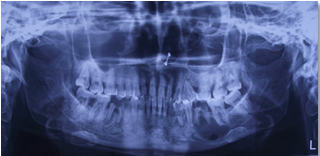
A 30 yr old female patient reported in the OPD with a chief complain of swelling and growth in the upper jaw region. Patient was apparently alright about 15 days back when she developed an intraoral growth in the maxillary posterior jaw region and extra oral swelling in the maxilla. The swelling was sudden in onset. Initially it was small and increased in size suddenly to present size. Patient had reported earlier in the OPD twice since 6 months for swelling and growth. For which she was treated by surgical excision, both the times. She was diagnosed as with peripheral ossifying fibroma and aggressive ossifying fibroma for 1st and 2nd visit respectively (Figure 1 & Figure 2)
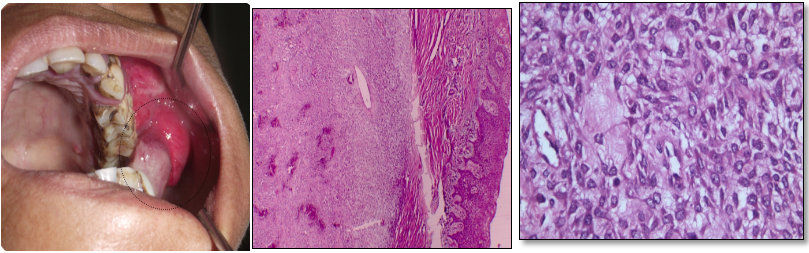
Extraoral findings revealed bilaterally asymmetrical face due to presence of large swelling in the left jaw region, which extends anterio-posteriorly 1 cm below the orbit of the left eye to the lower border of the left mandible & mesio -laterally from lateral wall of the left nose thru lower left lip to 3 cm in front of tragus of ear. The swelling is tender on palpation. Intraoral a well defined, pedunculated, roughly rectangular growth arising from posterior left maxillary tooth region seen. The growth is covering the occlusal surface of 26 and 27. The surface is irregular with surface indentation of teeth (Figure 3). On palpation the growth is tender, soft to firm in consistency, and is not fixed.
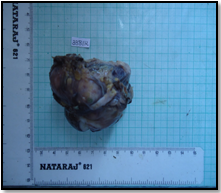
In keeping up with the above findings, provisional diagnosis of ossifying fibroma was made, whereas CEOT, Osteosarcoma, Chondrosarcoma were considered as differential diagnosis. Routine radiological and blood investigations were performed, which fail to reveal any significant finding. Complete surgical excision was done. The gross specimen macroscopically was grayish brown in color and was soft to firm in consistency.
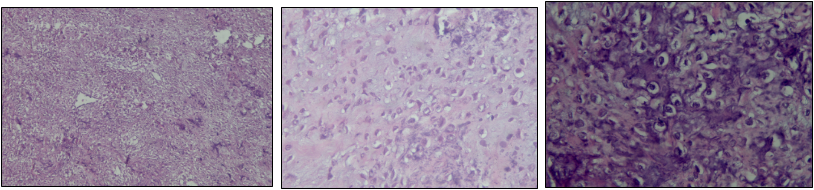
Histopathological finding shows lesional tissue consisting of tumor osteoid with dysplastic osteoblast and fibroblast. The dysplastic osteoblast are of varying shape and size; spindle to oval shaped. They show hyperchromatic nuclei with pleomorphism. Based on these features histopathological diagnosis of Low grade Osteosarcoma was made.
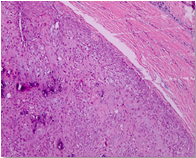
Figure 1-First visit of patient:- 1a-Extraoral view, 1b- Intraoral view, 1c- OPG –showing mixed radiolucent & radio opaque lesion, 1d- Photomicrograph of the biopsy of the lesion under 10X view showing foci of ossification in the background of cellular fibroblastic connective tissue, confirming diagnosis as peripheral ossifying fibroma.
Figure 2 Second visit: 2a-Intraoral view, 2b - Photomicrograph of the biopsy of the lesion under 10X view showing foci of ossification in the background of highly cellular fibroblastic connective tissue, 2c- Photomicrograph of the biopsy of the lesion under 40X view showing plump fibroblast with myxoid stroma confirming diagnosis of aggressive ossifying fibroma.
Third visit: 3a – Extraoral view, 3b-Intraoral view, 3c Gross Specimen, 3d - Photomicrograph of the biopsy of the lesion under 10X view showing foci of ossification in the background of highly cellular fibroblastic connective tissue, 3e,f- Photomicrograph of the biopsy of the lesion under 40X view showing tumor osteoid with dysplastic osteoblast and fibroblast confirming diagnosis of Low grade Osteosarcoma.
Discussion
Osteosarcoma (OS) is the commonest primary neoplasm of the bone, typically affecting the metaphysis of the femur or tibia in children and young adults [2]; it is the third commonest malignancy in adolescents [3]. About 10% of OS occurs in the head and neck [3]; those occurring in the jaws account for 4% [4]
OSs of the jaws are very rare and have a mild male predilection. At the time of diagnosis, the patients are approximately 2 decades older than those with extragnathic OS, which have a peak incidence between the ages of 10 and 14 years. However, most Gnathic OSs are high-grade lesions [5] and demonstrate a high mortality rate associated with local invasion that is usually difficult to control. [6] Similar to the conventional type of osteosarcoma, Lowgrade osteosarcoma (LOS; well-differentiated intraosseous osteosarcoma), has a predilection for the body of the mandible, and usually presents with a long-standing painless swelling [7]. The commonest signs and symptoms associated with jaw OS, as reported in the literature, consist of persistent pain, swelling, and paresthesia/anesthesia [8,9].
Several histologically unusual features of OS such as epitheliod [10,11] or small cell [12] subtypes and variable radiographic appearances [13] have been reported previously, which confirm the importance of meticulous evaluation of the patients with intraosseous lesions resembling OS; but a few cases with uncommon clinical presentation have been described and based on our knowledge the present case is the first reported OS with clinical presentation similar to “peripheral ossifying fibroma” & initially diagnosed as ossifying fibroma. In other reported rare clinical or radiographic presentations of OS, Soares. et al. [14] reported a patient with OS erroneously diagnosed as a periapical lesion and this delay in ac-curate diagnosis led to death of the patient after about 2 years. Yamamoto., et al. [15] described a case of maxillary OS with extremely unusual image findings in an 11-year-old boy and associated this strange feature with initial phase of tumor progression. Babazade., et al. [16] reported an uncommon bilateral metachronous OS of the mandibular body in a 27-year-old man and recommended that physicians should be aware that OS can occur in different sites as a true multicentric lesion. Shakib., et al. repotted a case in a 42 –year female patient with epulis fissuratum like feature. [17]
Histological diagnosis of OF and AOF was made in our case in her previous visits, which lead us to a diagnosis of recurrent OF again, but to the surprise the microscopic features of the lesion presented lead to the diagnosis of OS (low grade). To the best of our knowledge this is the first case reported with an unusual clinical presentation along with histological low grade type OS in maxillae. Sinha., et al. had reported a low grade osteosarcoma in mandible [18].
The differential diagnosis of LOS includes benign and low-grade spindle lesions such as fibrous dysplasia, ossifying fibroma, chondromyxoid fibroma, unclassifiable fibro-osseous lesions, as well as desmoplastic fibroma. Resection with wide surgical margins is the most important factor for prognosis and provides a 5-year survival rate of 80% [19]. Bony margins for resection should at least be 2 cm from the clinical-radiographic edge or the nearest suture in the midface. Soft tissue margins around an osteosarcoma resection should be 2 cm or more and assessed with frozen sections. Adjuvant chemotherapy or radiotherapy seems to be inefficacious in cases of LGCO 20. Recurrences of LGCO may exhibit a higher histopathological grade or dedifferentiation with potential for metastases that can lead to the death of the patient [21].
The transformation of a low-grade central osteosarcoma into a high-grade osteosarcoma on recurrence has been reported in 15% of the patients [20].
Low-grade central osteosarcoma is a rare neoplasm that histopathologically offers the potential for misdiagnosis as benign condition, most specifically fibrous dysplasia. Careful attention to clinical, radiographic, and microscopic findings is necessary to ensure establishment of the correct diagnosis, thus helping to prevent incorrect treatment and unfortunate outcome. Prognosis is good if an early diagnosis of the lesion is made with prompt surgical intervention.
In summary, we have presented an unusual case of LOS of the maxilla in a 42-year-old woman.
References
- Diniz AF., et al. “Low-grade central osteosarcoma of the mandible: a case study report”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 103.2 (2007): 246–252.
- Klein MJ and Siegal GP. “Osteosarcoma: anatomic and histologic variants”. Journal of Clinical Pathology 125.4 (2006): 555-581.
- Alves FA., et al. “Oral metastasis of telangiectatic osteosarcoma”. Oral Diseases 9.2 (2003): 104-106.
- August M., et al. “Osteogenic sarcoma of the jaws: Factors influencing prognosis”. Journal of Oral and Maxillofacial Surgery 69.9(1997): 198-204.
- Sinha R., et al. Low-grade osteosarcoma of the mandible. Journal of Maxillofacial and Oral Surgery 9.2 (2010): 186-190.
- Guadagnolo BA., et al. Osteosarcoma of the jaw/craniofacial region: outcomes after multimodality treatment. Cancer115.4 (2009): 3262-3270.
- Diniz AF., et al. “Low-grade central osteosarcoma of the mandible: a case study report”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 103.2 (2007): 246–252.
- Kassir RR., et al. “Osteosarcoma of the head and neck: Meta-analysis of nonrandomized studies”. Laryngoscope 107.1 (1997): 56-61.
- Cohen IJ: “Significant recent advances in the treatment of osteosarcoma”. Journal of Medical Science 29 (1993): 748-753.
- Carlos-Bregni R., et al. “Epithelioid osteosarcoma of the mandi-ble: a rare case with unusual immunoprofile”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 105.2 (2008): e47-52.
- Kaveri H., et al. “Epithelioid osteosarcoma of the maxilla: report of an unusual case”. British Journal of Oral and Maxillofacial Surgery47.2 (2009): 143-145.
- Uma K., et al. “Small cell osteosar-coma of the mandible: Case report and review of its diagnos-tic aspects”. Journal of Oral and Maxillofacial Pathology15.3 (2011): 330-334.
- Padilla RJ and Murrah VA. “The spectrum of gnathic osteosar-coma: caveats for the clinician and the pathologist”. Head Neck Pathology 5.1 (2011): 92-99.
- Soares RC., et al. “Os-teosarcoma of mandible initially resembling lesion of dental periapex: a case report”. Brazilian Journal of Otorhinolaryngology71.2 (2005): 242-245.
- Yamamoto A., et al. “Osteosarcoma of maxilla with unusual image findings in child”. The Bulletin of Tokyo Dental College52.4 (2011): 201-207.
- Babazade F., et al. “Bilateral metachro-nous osteosarcoma of the mandibular body: a case report”. Chang Gung Medical Journal34.6 Suppl(2011): 66-69.
- PA Shakib., et al. “Seyedmajidi. Osteosarcoma of the Maxilla: A Rare Case with Unusual Clinical Presentation”. Journal of Dental Research, Dental Clinics, Dental Prospects 7.3 (2013): 177-181.
- R Sinha., et al. “Low-Grade Osteosarcoma of the Mandible”. Journal of Maxillofacial and Oral Surgery 9.2 (2010): 186–190.
- Mayur Chaudhary and Shweta Dixit Chaudhary “Osteosarcoma of the jaw”. Journal of Oral and Maxillofacial Pathology 16.2 (2012): 233-238.
- Kurt AM., et al. “Low-grade intraosseous osteosarcoma”. Cancer 65.6 (2012): 1418-1428.
- Bennett JH., et al. “Osteosarcoma of the jaws: a 30-year retrospective review”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 90.3 (2000): 323-332.
Citation:
Priyanka Agarwal and Ahok Agarwal. “Osteosarcoma of Jaw: A Case Report with Unusal Presentation”. Oral Health and Dentistry
2.3 (2017): 375-380.
Copyright: © 2017 Priyanka Agarwal and Ahok Agarwal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.