Case Report
Volume 2 Issue 5 - 2018
Oral Submucous Fibrosis- a Potentially Malignant Disease.
1Postgraduate, Department of Oral Medicine and Radiology, A.J .Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
2Professor and Head, Department of Oral Medicine and Radiology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
3Professor Department of Oral Medicine and Radiology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
4Postgraduate, Department of Oral and Maxillofacial Pathology, A.J .Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
5Professor and Head, Department of Oral and Maxillofacial Pathology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
6Reader, Department of Oral and Maxillofacial Pathology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
2Professor and Head, Department of Oral Medicine and Radiology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
3Professor Department of Oral Medicine and Radiology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
4Postgraduate, Department of Oral and Maxillofacial Pathology, A.J .Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
5Professor and Head, Department of Oral and Maxillofacial Pathology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
6Reader, Department of Oral and Maxillofacial Pathology, A.J. Institute of Dental Sciences, Kuntikana, Mangaluru, Karnataka, India
*Corresponding Author: Vijayendranath Nayak S, Postgraduate, Dept of Oral Medicine & Radiology, AJ Institute of Dental Sciences, Kuntikana, NH-66, Mangaluru – 575004, Karnataka, India.
Received: February 05, 2018; Published: February 16, 2018
Abstract
Oral submucous fibrosis is a chronic premalignant condition which is predominantly seen in patients of Southeast Asia and India. OSMF is now considered to be a potentially malignant disorder with 1% malignant transformation rate.
Key words: Potentially malignant disorder; OSMF; OSF; Tobacco chewing; Arecanut
Introduction
Oral submucous fibrosis (OSMF) is a premalignant disorder associated with the chewing of areca nut (betel nut). The habit is prevalent in South Asian populations but has been recognized nowadays also in Europe and North America. OSMF causes significant morbidity. [1] In 1952, Schwartz coined the term atrophica idiopathica mucosa oris to describe an oral fibrosing disease, he discovered in 5 Indian women from Kenya. The strongest risk factor for OSMF is the chewing of betel quid containing areca nut. The amount of areca nut in betel quid and the frequency and duration of chewing betel quid are clearly related to the development of OSMF. [2] In this article, we report a case of betel quid induced OSMF.
Case Report
A 50 years, old male patient reported to the department of oral medicine and radiology with the chief complaint of inability to open mouth since 1 year. Patient gave a history of burning sensation which aggravated on having spicy food. Past medical and dental history was non-contributory. Patient gives history of betel quid chewing habit since 20 years with a frequency of 10-11 times/day. Intraoral examination revealed reduced cheek blowing capacity and tongue protrusion and restricted mouth opening (Figure A). Inspectory findings revealed blanching appearance of right and left buccal mucosa, labial mucosa, palate and on floor of the mouth. Blanching was also evident on soft palate, faucial pillars. (Figure B, C and D) On palpation interincisally opening was limited to 21 mm. Vertical bands were palpable in the buccal mucosa with respect to right and left posterior molar region and retro molar area. Circular band were palpable with respect to the mandibular labial mucosa. Based on the clinical findings a provisional diagnosis of Oral Submucous Fibrosis Stage III was given (According to Khanna and Andrade). [3] Incisional biopsy was taken. Histopathological sections revealed atrophic stratified squamous epithelium with erosion of surface epithelial cells is seen. Subepithlial areas show homogenized areas of fibrosis. Dense infiltrate of chronic inflammatory cells were seen (Figure E). On the basis of Histopathological and clinical findings a final diagnosis of Group III (moderately advanced Oral Submucous Fibrosis was considered. Patient was counselled about the ill effects of tobacco and arecanut chewing and was prescribed anti-oxidant capsules twice daily for 3 months and patient was recalled after 3 months for evaluation.
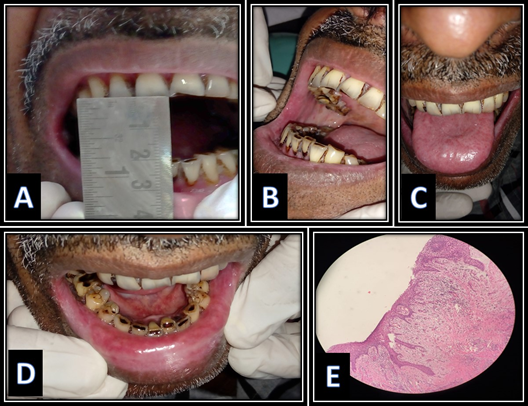
Figure 1: A: limited mouth opening evident.
B: Blanching of right buccal mucosa evident.
C: Depapillation of dorsal aspect of the tongue is seen.
D: Blanching of lower labial mucosa and floor of the mouth.
E: Histopathological section revealing classical features of OSMF.
B: Blanching of right buccal mucosa evident.
C: Depapillation of dorsal aspect of the tongue is seen.
D: Blanching of lower labial mucosa and floor of the mouth.
E: Histopathological section revealing classical features of OSMF.
Discussion
Oral submucous fibrosis (OSMF) is a chronic debilitating and potentially malignant condition of the oral cavity. It is resistant and progressive affecting the entire oral cavity that sometimes causes a gradual reduction in mouth opening that may even extend up to the pharynx. [4] Oral submucous fibrosis (OSMF) as defined by Pindborg as an insidious chronic fibrotic disease that involves the oral mucosa and occasionally the pharynx and upper third of oesophagus. OSMF is characterized by a juxtraepithelial inflammatory reaction followed by fibroelastic changes in the submucosa and epithelial atrophy that leads to stiffness of the oral mucosa causing trismus and inability to eat. Many names were given by many reserchers since 1952 (Table 1). [5]
| Authors | Year | Nomenclature given |
| Schwartz | 1952 | Atrophia Idiopathica mucosa oris |
| Joshi | 1953 | Submucosa fibrosis of palate and pillars |
| Lal | 1953 | Diffuse oral submucous fibrosis |
| Su | 1954 | Idiopathic scleroderma of mouth |
| De sa | 1957 | Submucous fibrosis of palate and cheek |
| George | 1958 | Submucous fibrosis of palate and mucosa membrane |
| Pindborg & Sirsat | 1964 | Oral submucous fibrosis |
| Goleria | 1970 | Sub-epithelial fibrosis |
Table 1: Nomenclature given by authors.
OSMF is a condition which is well recognized for its malignant potential and is particularly associated with areca nut chewing, the main component of betel quid. [6] various factors have been thought as causative agents for OSMF. Some of the factors implicated in the aetiology of this disease include areca nut chewing, ingestion of chillies, genetic processes, immunological process and nutritional deficiencies. [7]
Common signs and symptoms of the disease are difficulty in opening mouth, burning sensation on eating, particularly spicy food, and problems in hearing and speaking. The various treatment options are medical, surgical and oral physiotherapy; for the individual patient, customised treatment plan is to be made based on the extent of the disease. [8]
According to the study conducted by B Krishnamurthy., et al. Colchicine has been reported to be beneficial in the treatment of diseases associated with fibrosis. Antioxidant therapy has given good results in recent years. [9]
| Treatment modality | Group |
| Conservative treatment | Restriction of habits/behavioral therapy Nutritional or Supportive therapy Oral physiotherapy |
| Medical treatment | Steroids Hyaluronidase Collagenase Placental extracts Chymotrypsin INF‑gamma Haque Aloe vera Turmeric Pentoxifylline therapy |
| Surgical treatment | Nasolabial flaps and lingual pedicle flaps The use of buccal fat pad as a grafting source ErCr: YSGG lasers |
| Combined therapy | Combination of steroids and topical hyaluronidase. Nutritional and iron supplements with intralesional injection therapy using hyaluronidase, dexamethasone and topical application of triamcinolone acetonide 0.1%. |
Table 2: Various treatment modalities for OSMF according to various studies.
Conclusion
It’s always said that prevention is better than cure, which hold good even in treating OSMF. Withdrawal of habit plays a big role in treating this potentially malignant disorder. Since the etiopathogenesis is clearly not understood, more and more research needs to be carried, so that permanent cure for this condition can be attained.
References
- Haider SM., et al. “Clinical and functional staging of oral submucous fibrosis”. British Journal of Oral and Maxillofacial Surgery 38.1 (2000): 12–15.
- Rajalalitha P and Vali S. “Molecular pathogenesis of oral submucous fibrosis- a collagen metabolic disorder”. Journal of Oral Pathology & Medicine 34.6 (2005): 321–328.
- More CB., et al. “Classification system for oral submucous fibrosis”. Journal of Indian Academy of Oral Medicine and Radiology 24.1 (2012): 24-29.
- James, L., et al. “Management of Oral Submucous Fibrosis with Injection of Hyaluronidase and Dexamethasone in Grade III Oral Submucous Fibrosis: A Retrospective Study”. Journal of International Oral Health: JIOH 7.8 (2015): 82–85.
- Pindborg JJ., et al. “Clinical aspects of oral submucous fibrosis”. Acta Odontologica Scandinavica 22 (1964): 679–691.
- Chattopadhyay A and Ray JG. “Molecular Pathology of Malignant Transformation of Oral Submucous Fibrosis”. Journal of Environmental Pathology, Toxicology and Oncology 35.3 (2016): 193-205.
- Karemore TV and Karemore VA. “Etiopathogenesis and treatment strategies of oral submucous fibrosis”. Journal of Indian Academy of Oral Medicine and Radiology 23 (2011): 598–602.
- Deshpande A., et al. “Oral submucous fibrosis: a premalignant condition in a 14-year-old Indian girl”. BMJ Case Reports 2013 (2013): bcr2013200786.
- Krishnamoorthy B and Khan M. “Management of oral submucous fibrosis by two different drug regimens: A comparative study”. Dental Research Journal 10.4 (2013): 527-532.
- Koneru A., et al. “A systematic review of various treatment modalities for oral submucous fibrosis”. Journal of Advanced Clinical & Research Insights 2 (2014): 64-72.
Citation:
Vijayendranath Nayak S., et al. “Oral Submucous Fibrosis- a Potentially Malignant Disease.” Oral Health and Dentistry 2.5 (2018):
452-455.
Copyright: © 2018 Vijayendranath Nayak S., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.