Research Article
Volume 3 Issue 2 - 2018
Diabetes Mellitus and Dentistry: Knowledge and Perception of Medical Doctors in Abuja, Nigeria.
1Dental and Maxillofacial Department, State House Medical Centre, State House Abuja, FCT Nigeria
2Family Medicine Department, State House Medical Centre, State House Abuja, FCT Nigeria
3Dental and Maxillofacial Department, University of Abuja Teaching Hospital, Gwagwalada, Abuja, FCT Nigeria
2Family Medicine Department, State House Medical Centre, State House Abuja, FCT Nigeria
3Dental and Maxillofacial Department, University of Abuja Teaching Hospital, Gwagwalada, Abuja, FCT Nigeria
*Corresponding Author: IKIMI Nathan Ukuoghene, Dental and Maxillofacial Department, State House Medical Centre, State House
Abuja, FCT Nigeria.
Received: May 15, 2018; Published: May 24, 2018
Abstract
Diabetes mellitus is a systemic disease with several oral complications which are better managed by the dentist when the diabetic patient is promptly referred to him. Several studies have shown that there is a bi-direction relationship between diabetes mellitus and periodontal disease which is an oral complication. In view of this, it has been recommended that a better management of diabetes mellitus should be multi-disciplinary in approach involving the medical doctors and the dentist. Thus, the medical doctor needs to be equipped enough to know when to refer diabetic cases to the dentist. The objective of this study is to assess the knowledge of the medical doctor on the relationship of dentistry with diabetes mellitus and to review the medical doctor’s perception of the dentist role in the management of the diabetic patient.
This is a cross-sectional survey of medical doctors undergoing postgraduate medical training in three tertiary institutions, randomly selected in Abuja, Nigeria. The data collection tool was mainly questionnaire based, with two types of questions: 1. Structured closed-ended questions to assess perception; 2. Questions prepared with 5-point Likert scale to evaluate knowledge. Data were recorded and analysed statistically using SPSS 20 version (IBM Corp., Armonk, NY, USA) to calculate Student’s t-value, chi-square test and Fischer’s exact test.
Medical doctors in this study showed a good knowledge of the relationship between dentistry and diabetes mellitus with 88.6% ready to collaborate with the dentist in the management of diabetic patients. There was a positive correlation between age of medical doctors and their perception with 85.7% accepting that dental postings should be included in undergraduate medical training; this is different from a previous African study and it is higher than other studies. However, further studies should be carried out to compare medical doctors who are specialists and those who are general medical practitioner.
Key words: Diabetes Mellitus; Dentist, Doctors; Knowledge; Perception
Abbreviations: FCT: Federal Capital Territory; IBM: International Business Machines; WHO-World Health Organization; SPSS: Statistical
package for the social sciences; USA: United States of America
Introduction
Diabetes mellitus could be defined according to the American diabetic society as a group of metabolic disorders which results in hyperglycaemia due to defects in insulin secretion/insulin action, or both [1]. Classification of diabetes mellitus has been categorized into four (4) main classes namely: Type 1 which is mainly immune-mediated or idiopathic [2]; Type 2 which is regarded as the most common form of diabetes mellitus (DM) and it is characterized by hyperglycaemia, insulin resistance and relative lack of insulin [3]; Type 3 which consist of diabetes mellitus (DM) with specific defects such as: (a) genetic defects in the functions of β-cells (b) genetic defects in insulin actions (c) disease of the exocrine pancreas (d) and endocrinopathies [4,5]; and Type 4 which is gestational diabetes found exclusively in pregnant women but hyperglycaemic conditions usually return to normal after the birth of the baby.
The initial Symptoms of marked hyperglycaemia in diabetics include polyuria, polydipsia, polyphagia and blurred vision [6]. Long-term complications of DM include retinopathy with potential loss of vision, nephropathy leading to renal failure, peripheral neuropathy with risk of foot ulcers, amputations and Charcot joints, autonomic neuropathy causing gastrointestinal and cardiovascular symptoms including sexual dysfunction [6-8]. Research has shown that diabetics have a higher chance of having cerebrovascular diseases [8] including hypertension and abnormalities of lipoprotein metabolism [2]. Several oral complications have been associated with DM and these include periodontal diseases [6], salivary dysfunction with negative effects on the quality and quantity of the flow of saliva, oral fungal and bacterial infections [7,9]. Other oral complications are stomatitis, geographic tongue, traumatic ulcer, fissured tongue, benign migratory glossitis, lichen planus, lichenoid reaction and angular chelitis [6,7,10-14].
While the number of people suffering from diabetes mellitus is projected by the World Health Organisation (WHO) to increase from 171 million in 2000 to 366 million in 2030 with greater prevalence reported to occur in Asia and Africa due mainly to change in life style [15], periodontal disease which has been described internationally as the sixth complication of Type 1 and Type 2 diabetes mellitus after microangiopathy, retinopathy, neuropathy, microvascular disease and delayed wound healing would correspondingly increase [15]. The diabetic patient’s first contact for health complains is almost always the medical doctor, therefore the ability of the medical doctor to make accurate diagnosis and prompt referral to the dentist is integral to the successful management of diabetic dental patients [16]. Where this knowledge to make accurate diagnosis and prompt dental referral is missing, it becomes important to create avenues for continue update of knowledge of the medical doctor, including recommending the incorporation of dental education into the undergraduate medical school’s curriculum.
This study’s objectives are:
- To assess the knowledge of the medical doctor on the relationship of dentistry with diabetes mellitus
- To review his perception of the dentist in the management of the diabetic patient. These objectives would enable the researchers determine if the medical doctor is aware of the role of the dentist so as to make prompt dental referrals and if he would be prepared to continue or improve on further collaboration with the dentist in the management of the diabetic patients.
Methods and Materials
This is a cross-sectional survey of medical doctors undergoing postgraduate training in three tertiary institutions randomly selected and medical doctors’ in general medical practice in these institutions. The institutions are: (1) University of Abuja Teaching Hospital, Gwagwalada, Abuja, (2) National Hospital, Abuja and (3) Garki General Hospital, Garki Abuja. Ethical permits was applied for and obtained from the Federal Capital Territory Research and Ethics committee, Abuja.
The Data collection tool was mainly questionnaire-based which was divided into three sections. The first section was used to collect socio-demographic data such as age, sex, professional designation and years of practice. The second section consisted of close-ended questions designed to assess the perception of the medical doctor towards dentistry and diabetes mellitus. Questions such as “What role does the Dentist have in the management of diabetes mellitus” and “Which best describes the reason for bleeding gums in the diabetics” were asked? Options were given and the doctors were required to tick the most appropriate option.
Any correct answer was scored 1 while wrong answers were scored 0, maximum score was 10 and minimum score was 0. 0-3 was graded as poor, 4-6 as fair, 7 and above was graded as good. The third section consisted of questions aimed to assess the knowledge of the medical doctor and statements such as “Halitosis, gum swelling and bleeding gums are all indication of periodontal disease” and “Diabetic patients are prone to having oral infections” were asked. Likert scales of five points was used [17] and respondents were expected to answer by choosing if he “agrees, strongly agrees, don’t know, disagrees or strongly disagrees”. Strongly disagree was scored 0, while strongly agree was scored 4 with a maximum score of 50; scores 0-10 was regarded as poor, 11-20 as fair, 21-30 as good, 31-40 as very good, 41-50 as excellent. Data were recorded and analysed statistically using SPSS 20 version. (IBM Corp., Armonk, NY, USA). Student’s t-value was calculated, chi-square test statistics was done to compare the two variables and Fisher’s Exact Test was also calculated with 95% confidence interval.
Results
Participants consisted of 70 medical doctors from three different tertiary Health institutions and 12.9% were less than 25 years of age while most of the doctors about 48.6% were between 26-30 years of age. About 68.6% had less than 5 year experience in medical practice. See details in Table 1.
| Variable | Frequency (n = 70) | Percentage |
| Age group (years) | ||
| ≤25 | 9 | 12.9 |
| 26-30 | 34 | 48.6 |
| 31-35 | 12 | 17.1 |
| >35 | 15 | 21.4 |
| Gender | ||
| Male | 44 | 62.9 |
| Female | 26 | 37.1 |
| Designation | ||
| Specialized | 34 | 48.6 |
| General practice | 36 | 51.4 |
| Years of practice | ||
| ≤ 5 | 48 | 68.6 |
| 6-10 | 16 | 22.8 |
| > 10 | 6 | 8.6 |
Table 1: Socio-demographic characteristics of respondents.
Medical doctors that knew the role of the dentist in the management of DM were 68.6% while 74.3% knew the sub-specialty that manages gum diseases. About 88.6% of the medical doctors in this study, were willing to collaborate with the dentist in the management of patients with DM. Details in Table 2
| Variable | N = 70 | Frequency (%) |
| Role of dentist in management of diabetes mellitus. | No role | 17 (24.3) |
| Clearing of the gum | 5 (7.1) | |
| Examine the gum | 48 (68.6) | |
| Effect of poor oral hygiene status in diabetic patients. | Affect management of diabetes mellitus | 51 (72.9) |
| Strengthen the teeth | 4 (5.7) | |
| No effect | 13 (18.5) | |
| Not good for psychology of the patient | 2 (2.9) | |
| Best possible reason for bleeding gum in diabetics. | Impaired wound healing | 54 (77.1) |
| Accumulation of plaque and calculus | 11 (15.7) | |
| No reason | 5 (7.2) | |
| Sub-specialty in dentistry which manage gum disease. | Restorative dentistry | 4 (5.7) |
| Maxillofacial surgery | 4 (5.7) | |
| Periodontology | 52 (74.3) | |
| Don’t know | 10 (14.3) | |
| Color of healthy gum. | Red | 8 (11.4) |
| Pink | 58 (82.8) | |
| White | 2 (2.9) | |
| Dark red | 2 (2.9) | |
| Best referral for DM patients having blood taste in the mouth early in the morning. | Dental clinic | 59 (84.2) |
| A physician | 2 (2.9) | |
| An endocrinologist | 9(12.9) | |
| Disease condition that can occur in DM patients (multiple responses). | Increase tooth mobility | 55 (78.6) |
| Halitosis | 59 (84.3) | |
| Swollen gum | 48 (68.6) | |
| Relationship between DM and periodontal disease (multiple responses). | PD affect the management of DM | 43 (61.4) |
| DM affect the management of PD | 59 (84.3) | |
| No relationship | 6 (8.6) | |
| Opinion if dentist can suspect cases of poorly controlled DM from oral examination. | Yes all cases | 52 (74.3) |
| Yes, but under supervision of medical doctor | 7 (10.0) | |
| No | 11 (15.7) | |
| Collaboration with dentist necessary in management of DM patients. | Yes | 62 (88.6) |
| No | 8 (11.4) |
Table 2: Knowledge.
Only a few participants 2.9% did not know that halitosis and bleeding gums were indicative of periodontal disease. Majority of participates agreed that medical doctors should be taught sign and symptoms of periodontal diseases and this would improve dental referrals.
| Strongly agree | Agree | Don’t know | Disagree | Strongly disagree | |
| Halitosis, gum swelling and bleeding gum are all indication of PD | 28 (40.0) | 38 (54.3) | 2 (2.9) | 1 (1.4) | 1 (1.4) |
| Diabetics patients are prone to having oral infection | 33 (47.1) | 33 (47.1) | 2 (2.9) | 1 (1.4) | 1 (1.4) |
| Diabetics patients should visit the dental clinic regularly for oral examination | 31 (44.3) | 34 (48.5) | 2 (2.9) | 2 (2.9) | 1 (1.4) |
| All oral health related complains should be referred to dentist | 28 (40.0) | 25 (35.7) | 5 (7.1) | 10 (14.3) | 2 (2.9) |
| Community and public health training of medical student should include dental posting | 29 (41.4) | 31 (44.3) | 3 (4.3) | 2 (2.9) | 5 (7.1) |
| Periodontal disease in pregnant diabetic patients may affect the weight of the unborn baby | 10 (14.3) | 10 (14.3) | 40 (57.1) | 9 (12.9) | 1 (1.4) |
| Medical doctors being taught signs and symptoms of periodontal disease would improve the management of patients | 28 (40.0) | 40 (57.1) | 0 (0.0) | 0 (0.0) | 2 (2.9) |
| Maintaining a good periodontal health would help in achieving a stable glycemic status | 17 (24.3) | 26 (37.1) | 14 (20.0) | 11 (15.7) | 2 (2.9) |
| Elderly diabetics patients may loss teeth if urgent periodontal intervention don not take place | 23 (32.9) | 41 (58.6) | 4 (5.7) | 1 (1.4) | 1 (1.4) |
| The medical doctor should be taught how to detect periodontal disease | 25 (35.7) | 43 (61.4) | 1 (1.4) | 0 (0.0) | 1 (1.4) |
Table 3: Perception.
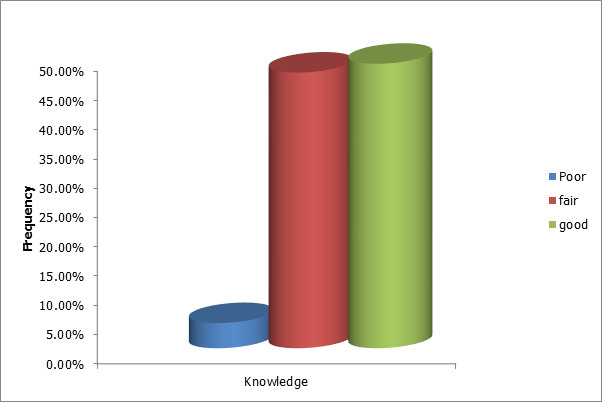
Overall, it was found that medical doctors in this present study had good knowledge of the role of the dentist in the management of diabetes mellitus. Details in Figure 1 below.
| Poor (n = 3) | Fair (n = 33) | Good (n = 34) | Total | statistics | |
| Age group (years) | |||||
| ≤ 25 | 0 (0.0) | 4 (44.4) | 5 (55.6) | 9 (100.0) | F = 5.927 |
| 26-30 | 2 (5.9) | 20 (58.8) | 2 (35.3) | 34 (100.0) | P = 0.439 |
| 31-35 | 0 (0.0) | 4 (33.3) | 8 (66.7) | 12 (100.0) | |
| > 35 | 1 (6.7) | 5 (33.3) | 9 (60.0) | 15 (100.0) | |
| Gender | |||||
| Male | 2 (4.5) | 23 (52.3) | 19 (43.2) | 44 (100.0) | F = 1.388 |
| Female | 1 (3.8) | 10 (38.5) | 15 (57.7) | 26 (100.0) | P = 0.499 |
| Designation | |||||
| Specialized | 2 (5.9) | 14(41.2) | 18(52.9) | 34(100.0) | F = 1.152 |
| General practice | 1 (2.8) | 19(52.8) | 16(44.4) | 36(100.0) | P=0.562 |
| Years of practice | |||||
| ≤ 5 | 2 (4.2) | 25 (52.1) | 21 (43.8) | 8 (100.0) | F = 7.667 |
| 6-10 | 0 (0.0) | 8 (50.0) | 8 (50.0) | 16 (100.0) | P = 0.105 |
| > 10 | 1 (16.7) | 0 (0.0) | 5 (83.3) | 6 (100.0) |
Table 4: Association between knowledge and socio-demographic characteristics.
F = Fischer exacts test
F = Fischer exacts test
| Fair (n = 15) | Good (n = 55) | Total | statistics | |
| Age group (years) | ||||
| ≤ 25 | 5(55.6) | 4 (44.4) | 9 (100.0) | F = 8.547 |
| 26-30 | 6 (17.6) | 28 (82.4) | 34 (100.0) | P = 0.036* |
| 31-35 | 3 (25.0) | 9 (75.0) | 12 (100.0) | |
| > 35 | 1 (6.7) | 14 (93.3) | 15 (100.0) | |
| Gender | ||||
| Male | 9 (18.2) | 36 (81.8) | 44 (100.0) | F = 0.742 |
| Female | 7 (26.9) | 9 (73.1) | 26 (100.0) | P = 0.389 |
| Designation | ||||
| Specialized | 8 (23.5) | 26 (76.5) | 34 (100.0) | F = 0.173 |
| General practice | 7 (19.4) | 29 (80.6) | 36 (100.0) | P = 0.677 |
| Years of practice | ||||
| ≤ 5 | 12 (35.0) | 36 (75.0) | 48 (100.0) | F = 2.068 |
| 6-10 | 3 (18.8) | 13 (81.2) | 16 (100.0) | P = 0.356 |
| > 10 | 0 (0.0) | 6 (100.0) | 6 (100.0) |
Table 5: Association between Perception and socio-demographic characteristics.
F = Fischer exacts test
F = Fischer exacts test
Discussion
The management of diabetic patients involves both medical and dental practitioners, however the first contact in the hospital for most diabetic patients with dental issues is usually their medical doctors and since prompt referral to the dentist is important for effective management of diabetic patients with dental challenges, we decided to examine the knowledge and perception of medical doctors in Abuja, without comparing with their dental counterparts [18] to find out if they have sufficient knowledge with the right perception to make timely referrals to the dentist.
This study was carried out among medical in three tertiary institutions in Abuja who completely filled and returned 70 questionnaires among the 96 questionnaires that were distributed in the institutions and this gave us a 73% return which consisted of 48.6% medical doctors in postgraduate training program and 51.4% medical doctors who are general medical practitioners. It is of interest that 68.6% have less than 5 years’ experience in medical practice and this included 48.6% young medical doctors between 26-30 years of age as shown in table 1.
Among the 70 respondents in this study, 68.6% believed that the role of the dentist in the management of diabetic patients includes the examination of the gums while 72.9% agree that poor oral hygiene would affect the management of diabetic mellitus (DM). Also, 61.4% believe that periodontal diseases (PD) would affect the management of DM. This result seems to be better than some previous African studies where in one case, only 46% of medical doctors felt PD could have a negative effect on DM while in another case, only 25.0% of medical doctors agreed that diabetic patients with poor oral hygiene where at risk of PD [18,19]. Furthermore, the bi-directional relationship between PD and DM was clear to medical doctors in this study as shown by the 61.4% who agreed that PD would affect the management of DM and 84.3% also agreed that DM would affect the management of PD.
This is different from a previous study where as low as 27.1% of medical doctors had knowledge of this bi-directional relationship between PD and DM [19] while the study of Al-Khabbaz., et al. reported that 42.2% general medical practitioners were found to have such knowledge [20]. Nevertheless, Rola Al-Habashneh., et al. [21] agreed with our study when they gave a report that 70% out of the 164 doctors in their study, had heard of the link between diabetes and oral health. Medical doctors in this study were knowledgeable about the symptoms of periodontal diseases as indicated by the 78.6% who reported that increased tooth mobility would occur in diabetic patients with periodontal diseases while 68.6% reported that swollen gum might also be noticed in diabetic patients. This is in consonance with the study of Alkan and Tasdemir who both gave a report that 87% of medical doctors knew the symptoms of PD while 90% agreed that there was a relationship between PD and systemic health [22].
The medical doctors in this present study had sufficient knowledge of periodontal disease (PD) and diabetic mellitus (DM) thus, 88.6% were ready to collaborate with the dentist in the management of diabetic patients. Also, a combination of 75.7% had a good perception of DM and dentistry and they were all in agreement that all oral health related complains in diabetic patients should be referred to the dentist for effective management. The result in this present study is better than the results of Alkan and Tasdemir who both reported that 56.5% were in agreement of referring [22], Al-Habashneh et al reported 49.7% in agreement [23] while Owen et al reported 48% in agreement. [24].
Majority of the medical doctors in our study also agreed that they should be taught signs and symptoms of PD in medical school. While 41.4% strongly agreed, 44.3% agreed that community and public health training of medical students should include dental postings. This level of perception towards dental education is different from the report of a different study where the medical doctors did not agree that dental topics should be included in undergraduate medical classes [19]. Nonetheless, doctors in North Carolina were eager to receive more training on how to examine for oral diseases in diabetic patients according to the reports of Owen., et al. [24]. A positive correlation was found between perception and age-group in this study which was statistically significant; this might explain the adequate knowledge seen in this study among this age-group of less than 35years of age and also the good perception towards dentistry and dental education. Moreover, since majority of these young medical doctors were in postgraduate medical training for specialization, they were more receptive to new ideas and this is in agreement with the observations of Sede and Ehizele who both concluded in their study that the level of knowledge increases as specialization of medical doctors increases [19].
Some drawbacks in this study were a lack of participation of medical doctors older in age with longer years of practice in the medical profession either as general practitioners or as specialists. Also, the relationship of other systemic diseases and periodontal diseases was not investigated, instead only the relationship between DM and PD was investigated.
Conclusion
Within the limitations of this study, medical doctors in Abuja have adequate knowledge and good perception of periodontal diseases and diabetes mellitus. Their continued collaborations with the dentist in the management of diabetic patients should be encouraged while equipping the medical doctors further with regular continued dental educations in form of dental journals, update lectures and seminars. Collaborative research works like this present one should also be sponsored and encouraged between medical and dental practitioners.
Acknowledgement
I wish to acknowledge the continue support and encouragement of my wife Roselyn Olaronke Ikimi who proof read the whole manuscript.
I wish to acknowledge the continue support and encouragement of my wife Roselyn Olaronke Ikimi who proof read the whole manuscript.
Conflict of Interest
There is no conflict of interest to report. This entire research was self-sponsored.
There is no conflict of interest to report. This entire research was self-sponsored.
References
- American Diabetes Association. “Diagnosis and classification of Diabetes mellitus”. Diabetes care 34 (Suppl 1) (2011): S62-S69.
- Baynes HW. “Classification, Pathophysiology, Diagnosis and Management of Diabetes Mellitus”. Journal of Diabetes and Metabolism (2015).
- Maitra A and Abbas AK. Endocrine system. Robbins and Cotran Pathologic basis of disease (7th edtn). Saunders, Philadelphia (2005)1156-1226.
- Alberti KG and Zimmet PZ. WHO Expert Committee on Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications, Geneva: (1999): 1-59.
- Jumpup Williams Textbook of endocrinology (12thed.). Elsevier/Saunders, Philadelphia, USA (2007): 1371-1435.
- Azodo CC. “Current trends in the management of diabetes mellitus: The Dentist’s Perspective”. Journal of Postgraduate Medicine 11.1 (2009): 113-129.
- Ogunbodede EO., et al. “Oral health status in a population of Nigerian diabetics”. The Journal of Contemporary Dental Practice 6.4 (2005): 75-84.
- Chinenye S., et al. “Profile of Nigerians with Diabetes mellitus- Diabcare Nigerian study group (2008); Results of a multicentre study”. Indian Journal of Endocrinology and Metabolism 16.4 (2012): 558-564.
- Al-Maskari AY., et al. “Ora Manifestations and Complications of Diabetes Mellitus: A review”. Sultan Qaboos University Medical Journal 11.2 (2011): 179-186.
- Sandberg GE., et al. “Type 2 diabetes and oral health: A comparison between diabetic and non-diabetic subjects”. Diabetes Research and Clinical Practice 50.1 (2000): 27-34.
- Chomkhakhai U., et al. “Oral health in Thai patients with metabolic syndrome”. Diabetes & Metabolic Syndrome 3 (2009): 192-197.
- Collin HL., et al. “Oral symptoms and signs in elderly patients with type 2 diabetes mellitus”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 90.3 (2000): 299-305.
- Guggenheime J., et al. “Insulin-dependent diabetes mellitus and oral soft tissue pathologies I: Prevalence and characteristics of non-candidal lesions”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 89.5 (2000): 563-569.
- Guggenheimer J., et al. “Insulin-dependent diabetes mellitus and oral soft tissue pathologies II: Prevalence and characteristics of Candida and candidal lesions”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 89.5 (2000): 570-576.
- Ikimi NU., et al. “Oral Health Knowledge and Attitude of diabetic patients in Lagos State University Teaching, Lagos State”. Nigerian Journal of Dental Research 2.1 (2017): 36-41.
- Al-Habashneh R., et al. “Diabetes and Oral health: doctor’s knowledge, perception and practices”. Journal of Evaluation in Clinical Practice 16.5 (2010): 976-980.
- Likert R. “A Technique for the Measurement of Attitudes”. Archives of Psychology140 (1932) 1–55.
- Habib ZM and Moshy J. “Periodontal disease; Knowledge awareness and attitude of medical doctors towards periodontal disease in Dar es Salaam, Tanzania”. The Professional Medical Journal 20 (2013): 290-295.
- Sede MA and Ehizele AO. “Oral diseases and diabetes: Nigerian medical and dental caregivers' perspective”. Annals of African Medicine 14.4 (2015): 193-199.
- Al-Khabbaz AK., et al. “Knowledge about the association between periodontal diseases and diabetes mellitus: contrasting dentists and physicians”. Journal of Periodontology Online 82.3 (2011): 360-366.
- Al-Habashneh R., et al. “Diabetes and oral health: doctors' knowledge, perception and practices”. Journal of Evaluation in Clinical Practice 16 (2010): 976-980.
- Alkan BA and Tasdemir Z. “Knowledge of medical doctors in Turkey about the relationship between periodontal disease and systemic health”. Brazilian Oral Research 29.1 (2015).
- Al-Habashneh R., et al. “Survey of medical doctors’ attitudes and knowledge of the association between oral health and pregnancy outcomes”. International Journal of Dental Hygiene 6.3 (2008): 214-220.
- Owens JB., et al. “North Carolina internists’ and endocrinologists’ knowledge, opinions, and behaviors regarding periodontal disease and diabetes: need and opportunity for interprofessional education”. Journal of Dental Education 75.3 (2011): 329-338.
Citation:
IKIMI Nathan Ukuoghene., et al. “Diabetes Mellitus and Dentistry: Knowledge and Perception of Medical Doctors in Abuja,
Nigeria.” Oral Health and Dentistry 3.2 (2018): 583-591.
Copyright: © 2018 IKIMI Nathan Ukuoghene., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.