Research Article
Volume 4 Issue 2
Efficacy of Intraoral Plates in the Treatment of Snoring and OSA
1School of Continuous Training in Dentistry, Aeronautical University Institute, Specialist in Aeronautical Dentistry, Orthodontic Specialist, Postgraduate Professor in Craniomandibular Disorders, Argentine Republic
2Faculty of Mathematics, Astronomy and Physics, National University of Cordoba, MSc. in Physics, Specialist in TMJ Biomechanics, Argentine Air Force Former Military Aviator, MSc. in Aeronautical and Aerospace Systems, Argentine Republic
*Corresponding Author:Roberto Daniel Mesas, School of Continuous Training in Dentistry, Aeronautical University Institute, Specialist in Aeronautical Dentistry,
Orthodontic Specialist, Postgraduate Professor in Craniomandibular Disorders,
Argentine Republic.
Abstract
Snoring is an acoustic phenomenon that occurs during sleep as a result of the vibration of the nasal-oral structures. It is a consequence of resistance to air flow in the upper airway.
It should be a reason for medical consultation as it can hide an OSA (obstructive sleep apnea). It is estimated that 45% of adults snore.
In general, the structures involved are the uvula and the veil of the palate. An irregular air flow appears caused by a blockage that is normally one or more of the following:
- Weakness in the throat, causing it to close during sleep.
- Displacement of the jaw, often caused by muscle tension in the neck.
- Fat accumulated around the throat.
- Obstructions in the nasal passages.
- Obstructive sleep apnea.
- Narrow channels, causing the lateral tissues to touch each other.
- Relaxers such as alcohol, able to relax the throat muscles.
- Position on the back, which can move the tongue towards the back of the mouth.
Keywords: TMJ; Temporomandibular System; Functional Dynamic; Biomechanical Lever; OSA; Snoring; Integral Holistic Vision, Factor Correlation
Material and Method
34 patients were diagnosed with snoring and moderate OSA, evaluated by pneumonologists and it was decided to see the effectiveness of the mandibular overtaking devices, in order to know if they were effective in this type of patient.
10 patients were over 50 years of age and overweight, 7 patients between 40 years old and 49 years old and 3 of them overweight, 10 patients between 30 years old and 39 years old, with 2 overweight patients and 7 patients between 23 and 29 years of age with normal weight.
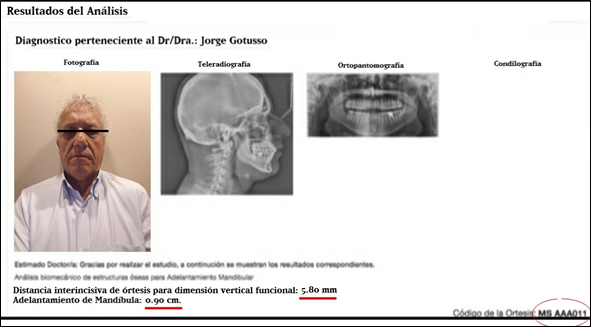
All of them were studied by orthopantomography to see the general stock of the stomatognathic system and mainly the TMJ, resulting in that 100% of the cases had TMJ alterations.
They were also asked for a Cranial Profile Teleradiography, to observe the "Tragus", where the decrease of the airway was observed in all patients.
All had free nasal passages and none said they were consumers of alcoholic beverages.
| No overweight | With overweight | TMJ Disfunction | Alcoholic consumer | Nasal obstructions | |
| 50 years old or more | 10 | 0 | 10 | 10 | 0 |
| Beetwen 40 & 49 years old | 7 | 4 | 3 | 7 | 0 |
| Beetwen 30 & 39 years old | 10 | 8 | 2 | 10 | 0 |
| Beetwen 23 & 29 years old | 7 | 7 | 0 | 7 | 0 |
| Total number of patients | 34 | ||||
Symptoms of Snoring
Snoring is a sign of Sleep Disorder and a disturbance in breathing, and can have serious consequences, starting with a soporific state of temporary drowsiness, temporary loss of memory (difficulty remembering names, dates, etc.), partial disability of the logical reasoning (performing arithmetic operations for example), headaches, irritability, difficulty memorizing, loss of situational awareness and abrupt changes in character. It can be said that it affects the human being in:
Snoring is a sign of Sleep Disorder and a disturbance in breathing, and can have serious consequences, starting with a soporific state of temporary drowsiness, temporary loss of memory (difficulty remembering names, dates, etc.), partial disability of the logical reasoning (performing arithmetic operations for example), headaches, irritability, difficulty memorizing, loss of situational awareness and abrupt changes in character. It can be said that it affects the human being in:
- Physical Health:
The body does not rest, Deterioration of the quality of personal and social life, Hypertension, Heart problems, Irritability. - Mental health:
Tiredness (the person fails to rest), Drowsiness, Difficulty to perform logical associations and analyzes, Stress, Headache, Memory loss.
What is sleep apnea?
Other names of sleep apnea
Other names of sleep apnea
- Central sleep apnea.
- Obstructive sleep apnea (OSA).
- Respiratory sleep disorder.
Sleep apnea is a common disorder in which the person suffering from it pauses one or more breaths or has shallow breaths during sleep.
Pauses can last between a few seconds and several minutes. They often occur 30 times or more per hour. In general, breathing returns to normal, sometimes with a loud snore or a sound similar to what a person makes when choking.
Almost always sleep apnea is a chronic (Constant) health problem that alters sleep. The person goes from a deep sleep to a light sleep when there is a pause in the breath or when the breathing becomes shallow.
For this reason, sleep is of poor quality and you feel tired during the day. Sleep apnea is one of the main reasons why a person can feel very sleepy during the day.
Often sleep apnea remains undiagnosed. Typically, doctors cannot detect it during current consultations. Also, there are no blood tests for this problem.
Most people who suffer from sleep apnea do not know they have it because it only happens during sleep. The first to notice the signs of sleep apnea may be a family member or who sleeps in the same bed with the affected person.
The most common type of sleep apnea is obstructive sleep apnea. In it the airways narrow or block during sleep. This causes shallow breathing or breathing pauses.
When the person tries to breathe, the air that manages to pass through the clogged part can cause loud snoring. Obstructive sleep apnea is more common in overweight people, but it can affect anyone. For example, young children who have swollen tonsils may have obstructive sleep apnea.
Central sleep apnea is a less frequent type of sleep apnea. It happens when the part of the brain that controls breathing does not send the correct signals to the respiratory muscles. As a result, the person makes no effort to breathe for short periods.
Central sleep apnea can occur in anyone. However, it is more frequent in those who suffer certain diseases or use certain medicines.
Central sleep apnea can occur alone or with the obstructive form of the disease. Usually, there is no snoring in the central sleep apnea.
At the anatomical level, the upper airway is a muscular-membranous tube that extends caudal and narrows as it descends. When we inspire, the pharyngeal structures are pushed in by sub atmospheric intraluminal pressure and intrathoracic displacement of the trachea.
Prior muscle activation is required for respiratory movements to occur. There are two muscle groups: those that generate pressure (including the diaphragm) and the muscles of the Upper Airway (suprahyoids, infrahyoids, elevators and constrictors of the pharynx, the musculature of the tongue and the veil of the palate).
The Upper Airway is made up of the nostrils, the pharynx and the larynx. The pharynx can be divided into four zones: rhinopharynx, velopharynx, oropharynx and hypopharynx.
In the functioning of the Upper Airway, in the absence of pathology during the waking state, there is a balance between the strength of the inspiratory muscles and the pharyngeal dilator muscles, allowing adequate gas exchange and the permeability of the upper airway. Likewise, during this state, the oxygen pressure decreases or the carbon dioxide pressure increases due to various stimuli of the proprioceptors and the environment.
During sleep, breathing changes occur, the respiratory control being less rigid than during wakefulness. The decrease in muscle tone during sleep especially affects the pharyngeal dilator muscles, while the diaphragm maintains its muscle tone. This fact induces the collapse of the Upper Airway, increases resistance to air passage and hinders ventilation and gas exchange.
According to a study, carried out in 1993 by Morrison., et al. (1), On the levels of distribution of the collapsible segments of the pharynx by endoscopic methods, a narrowing of the area greater than 75% was defined as primary narrowing and secondary narrowing to the reductions between 25% and 75% of the luminal area. He made measurements in the three segments of the most collapsible pharynx (velopharynx, oropharynx and hypopharynx) in 64 patients affected by OSA. According to their results, 75% of them presented more than one place of pharyngeal stenosis, in 81% the primary narrowing was in the velopharynx, in half of them there were secondary narrowings in 25% in oropharynx and 32% in hypopharynx, concluding that “the soft palate area (velopharynx) is the most common place of pharyngeal stenosis”.
Other studies mention that the place where the upper airway obstruction occurs is limited to a certain segment; in 50% of OSA to the velopharynx and in another 50% to the hypopharynx. (2)
When our normal respiratory pattern is disturbed during sleep, we will refer to sleep respiratory disorders, which may be obstructive or non-obstructive. Obstructive respiratory disorders have as main feature the collapse of the pharynx, as well as the presence of snoring, which can be classified as primary or chronic. Primary snoring, according to the American Sleep Disorder Association (ASDA), is defined as the severe respiratory sounds produced in the Upper Airway during sleep, as well as a soft tissue vibration of the pharynx that usually occurs on inspiration; no episodes of apnea, hypoventilation, desaturation, or micro-wakefulness or evidence of insomnia, or snoring-related hypersomnia. Chronic snoring includes episodes of apnea, hypoventilation, desaturation or micro wake up, which is associated with OSA (3)
According to some studies, 1/3 adults usually snore and 50% snore from time to time.
Almost 70% of people who snore have a hereditary bond. Regarding sex, men snore in a 2: 1 ratio in relation to women, which is modified from menopause. Snorers are three times more likely to suffer adverse health problems regarding non-snorers.
There are several etiological factors that produce snoring and OSA. We can group them into risk factors, anatomical, physiological, pathological and neurochemical.
As risk factors are age (as we age we lose muscle tone and with it the chances of snoring are increasing; the prevalence of OSA increases 2 to 3 times from 65 years on adults from 30 to 46 years), sex (the prevalence of OSA in men in relation to women is 10: 1. Women, by segregating estrogens, hormones that protect the muscles of the neck, prevent the relaxation of it during sleep at menopause, and consequently estrogen production decreases, women may snore like men.), obesity /overweight (one of the factors that most influences the etiology of snoring and OSA. Excess weight produces sagging neck muscles and consequently closes the light of the Upper Airway. (4)
While two thirds of patients with OSA are obese, thin people can also suffer from the disease.), Tobacco (nicotine irritates the veil of the palate, the uvula and the pharynx, increasing snoring), alcohol ( favors the relaxation of the neck muscles), medications (anxiolytic, hypnotic, antidepressant or anti-tamine, as they relax the upper respiratory tract), inheritance / genetics (if there are relatives with this syndrome, the risk increases from 2 to 4 times, with a higher risk if several family members are affected It has been estimated that between 40% and 50% of the apnea variance can be attributed to family factors, which could influence the mandibular size, tongue or tissue lymphoid It is also known that some genetic defects have a higher frequency of sleep apnea, such as Down syndrome, Pierre-Robin and Marfan). As anatomical factors, we can determine all those structural anomalies such as: the deviation of the nasal septum (hinders the passage of air), the ogival palate (very high, which narrows the opening that communicates the nose and neck), an uvula larger in size usual, large tonsils, retrognathia and mandibular micrognathia (since when relaxing they tend to move backwards and close the passage of air) and macroglossia.
As physiological factors, the displacement of the tongue towards the oropharynx and / or alteration in the tone of muscles such as the hyoid, pharyngeal, genioglossal and tensor of the palate veil after sleep relaxation, especially in the supine position; demonstrated through electromyographic studies. (5)
As pathological factors, polyps or tumors in the upper respiratory tract, allergic processes, mucus, type II diabetes mellitus, inflamed and hypertrophied tissues, acromegaly, kyphoscoliosis, hypothyroidism, amyloidosis, Prader Willy syndrome, arthritis rheumatoid with TMJ involvement (causing micrognathia and retrognathia), pharyngeal masses or tissues such as lymphomas, ectopic thyroid, syndromes polyformative, rare diseases (such as syringomyelia, myasthenia gravis, muscular dystrophy and some myopathies that generate poor motor control or lack of muscle tone in the neck structures)
As neurochemical factors, the alterations in the carbon dioxide threshold at the level of the central nervous system that would favor the greater tendency to generate apneas and hypopneas.
As for the pathophysiology of the syndrome, a critical narrowing of the VAS during sleep causes an occlusion and apnea even in the presence of inspiratory effort of the thoracic muscles, but without air entering the lungs due to the obstruction. (6)
This fact will condition several pathophysiological processes for the patient as.
- a) Oxygen desaturation or hypoxemia, hypercapnia and acidosis (produced by apnea or hypopnea).
- b) Secondary stimulation of the autonomic nervous system with activation of the tone of the dilator musculature.
- c) Repeated micro wake up, causing the sleep distructuring.
Hypoxemia occurs during sleep due to the loss of tonicity of the dilator muscles of the upper airway, which will exert an insufficient diminished dilating force to compensate for the negative pressure produced by the inspiring muscles (intercostal and diaphragm), interrupting airflow. This causes the decrease in oxygen saturation in oxyhemoglobin. As well as, it causes the activation of the autonomic nervous system that, in addition to stimulating the tone of the upper airway musculature to reverse apnea, increases(7) in a way that reflects peripheral resistance, with the production of pulmonary hypertension (PHT) and arterial hypertension (HT). Also, through sympathetic stimulation it favors the activation of the renin-angiotensin-aldosterone system, which would enhance the hypertensive effect. The incidence of high blood pressure is between 20-70% of patients with OSA; sleep arousals and snoring, without apnea or hypopnea, are also a factor in elevation of blood pressure. Repeated awakenings are associated with an increase in daytime blood pressure.
Similarly, the activation of the autonomic nervous system favors the development of arrhythmias; of bradyarrhythmic type by parasympathetic stimulation during the apneic phase and tachycardic during the sympathetic stimulation phase, apnea recovery period.
In addition, the increase in sympathetic stimulation in OSA increases platelet aggregation, favoring the prothrombotic state which can lead to acute myocardial infarction. (8)
Likewise, the existence of repeated cycles of hypoxemia and reoxygenation induces possible vascular damage and the activation of inflammatory factors, which contributes to endothelial dysfunction, generating a greater predisposition to cardiovascular diseases. OSA and the presence of coronary artery disease are related; It has been shown in a study with patients with diagnosed symptomatic angina that 30.5% had OSA,
This group had a higher rate of apnea-hypopnea and a greater tendency to be overweight and obese. Likewise, it was found that atherosclerosis and coronary heart disease increased as the grade of OSA worsened. It has also been shown that snoring can put patients at risk of atherosclerosis of the carotid artery, as a result of vibrations that occur in the pharyngeal airway, near the carotid artery, which can cause endothelial damage, producing inflammation that entails to atherosclerosis. The prevalence of atherosclerosis worsens in direct proportion to the degree of snoring. (9)
The risk for stroke is associated with patients with OSA, which is increased by daytime hypertension, due to the decrease in cerebral perfusion and an increase in coagulation; likewise, after a stroke, the prevalence for OSA increases, this being a difficulty for the patient's recovery process.
Snoring and OSA, because they cause obstruction of the upper airway, lead to the desaturation of oxygen, which in turn can cause the level of cortisol and catecholamines to rise, which produces an increase in insulin resistance; This fact would lead to diabetes. Also, hypoxia during sleep can lead to glucose intolerance, regardless of age, sex and body mass index (BMI). A third of those with type 2 diabetes have sleep problems, which are aggravated to a greater severity of it (10).
Hypercapnia, increased carbon dioxide, conditioned by periods of apnea / hypopnea, would be the cause, due to the vasodilator effect of carbon dioxide, of morning headaches suffered by these patients. Headache in patients with OSA is 8.4 times higher than in the normal population. Of the patients with headache, 53% were diagnosed with OSA.
The increase in intrathoracic negative pressure, generated to overcome the obstruction of the Upper Airway, together with the overload of the cardiac cavities, due to arterial hypertension and pulmonary hypertension, induce the production by the cardiac myocytes of the atrial natriuretic peptide, which favors the renal elimination of water and sodium by inhibiting antidiuretic hormone and SRAA, thus conditioning nocturia. In addition, this negative airway pressure is also associated with narrowing of the VAS during inspiration, which affects the esophagus. (11)
Prospects
Sleep apnea that is not treated can increase the risk of suffering:
Sleep apnea that is not treated can increase the risk of suffering:
- a- High blood pressure,
- b- Heart attack,
- c- Stroke (stroke),
- d- Obesity and diabetes,
- e- Heart failure or if it worsens,
- f- Arrhythmias or irregular heartbeats,
- g- Car or work accidents.
Sleep apnea is a chronic health problem that requires long-term treatment:
- 1) Changes in lifestyle.
- 2) Intra and extra oral devices.
- 3) Surgery or respiratory devices
Intra-oral devices are the most accepted worldwide for the treatment of OSA.
The ASDA (American Association of Sleep Disorders) considers Mandibular Advancement Plates as a valid and first choice alternative for simple snorers, patients with mild OSA, moderate OSA with low body mass index and patients with SRAVAS ( Increased resistance syndrome of the upper airway).
The ASDA (American Association of Sleep Disorders) considers Mandibular Advancement Plates as a valid and first choice alternative for simple snorers, patients with mild OSA, moderate OSA with low body mass index and patients with SRAVAS ( Increased resistance syndrome of the upper airway).
For patients who refuse or do not respond correctly to CPAP treatment, patients with high surgical risks and patients with a poor response to surgical treatment, DAMs are considered as a second option.
Results
Mandibular Overtaking Plates (MOP)
With regard to studies comparing MOP with CPAP, most of them show a similar efficacy of both treatments on drowsiness, although patients usually prefer MOP.
With regard to studies comparing MOP with CPAP, most of them show a similar efficacy of both treatments on drowsiness, although patients usually prefer MOP.
Treatment with mandibular advancement plates
MESER ® is a custom-made intraoral device that is used during sleeping hours. Discreet, comfortable and effective, it produces adequate breathing totally eliminating snoring. Tubes or masks are not necessary, it is removable and the patient can take it with them and use it in their usual accommodation or anywhere else.
MESER ® is a custom-made intraoral device that is used during sleeping hours. Discreet, comfortable and effective, it produces adequate breathing totally eliminating snoring. Tubes or masks are not necessary, it is removable and the patient can take it with them and use it in their usual accommodation or anywhere else.
Adherence to DAM treatment is quite high. Several clinical studies show that 68% of patients continue to use the device after 3 years. (12)
Currently, custom-made DAMs are used to allow progressive advancement of the jaw to reach the optimum and tolerable degree of protrusion.
Benefits of the Meser® System
Therapeutic ease and immediacy
The unit size of the device is reduced, to deprogram the orthognathic system.
Therapeutic ease and immediacy
The unit size of the device is reduced, to deprogram the orthognathic system.
The opening generated by the device in an anterior hinge axis opposite the axis of the TMJ, which favors the mandibular advance by unclogging the pharynx the more opening the patient makes, forcing greater mandibular advancement. The unique effect compared to other devices. (14)
It has sliding tracks with a deprogramming effect of the TMJ, which allow the muscle relaxation of the patient and the omission of neuroblocking signals that favor systemic pathologies and undefined neurofocal effects. (15)
It involves a multiple solution to various problems of both mild snoring, apnea and occlusal pathology, which in some cases are related and in others cases of snoring and stress can be solved simultaneously.
Rules and Recommendations
The MOP in patients are mild and moderate OSA the regulations of the American Academy of Sleep Medicine establish that MOPs are indicated in patients with mild-moderated OSA as an alternative to CPAP.
Recent European regulations also recommend treatment with MOP in patients with mild or moderate OSA and in those who do not tolerate CPAP.
According to SEPAR (Spanish Society of Pulmonology and Thoracic Surgery), MOPs are effective in the treatment of snoring and mild-moderated with low BMI and minor desaturations. They may also be useful in patients with increased resistance syndrome of the upper airway and those who do not tolerate CPAP and who are not candidates for surgery. (15)
Why Use Mandibular Advancing Plates? (MESER® SYSTEM)
- a) Your comfort and easy use.
- b) It is custom made with an ergonomic and comfortable design.
- c) Its manufacture is based on biocompatible materials.
- d) It can be easily adjusted.
- e) Allows mouth movements, without too many limitations.
- f) Allows proper breathing by totally eliminating snoring.
- g) It can be applied to permanent pieces, partial tooth lessness or artificial fixations.
- h) It helps improve the quality of life, getting a restful sleep.
- i) Easy cleaning of the device.
- j) Product warranty of up to 12 months.
TOLERANCE OF MESER® IN PATIENTS: 95%
AIR VOLUME INCREASE: 40% or more.
PATIENTS THAT IMPROVE YOUR IAH BELOW: 94%
REDUCE YOUR LEVEL OF SLEEP APNEA TO: 90%
AIR VOLUME INCREASE: 40% or more.
PATIENTS THAT IMPROVE YOUR IAH BELOW: 94%
REDUCE YOUR LEVEL OF SLEEP APNEA TO: 90%
MESER® can end snoring and reduce sleep apnea, returning to many patients and their partners the quality of sleep and life of which, for years, they have been deprived.
Conclusions
Snoring and OSA, because they cause obstruction of the upper airway, lead to the desaturation of oxygen, which in turn can cause the level of cortisol and catecholamines to rise, which produces an increase in insulin resistance(16); This fact would lead to diabetes. Also, hypoxia during sleep can lead to glucose intolerance, regardless of age, sex and body mass index. A third of those with type 2 diabetes have sleep problems, which are aggravated to a greater severity of it (17).
Hypercapnia, increased carbon dioxide, conditioned by periods of apnea / hypopnea, would be the cause, due to the vasodilator effect of carbon dioxide, of morning headaches suffered by these patients. Headache in patients with OSA is 8.4 times higher than in the normal population. Of the patients with headache, 53% were diagnosed with OSA.
The increase in intrathoracic negative pressure, generated to overcome the obstruction of the upper airway, together with the overload of the cardiac cavities, due to arterial hypertension and pulmonary hypertension, induce the production by cardiac myocytes of the atrial natriuretic peptide, which favors the renal elimination of water and sodium by inhibiting antidiuretic hormone (ADH) and SRAA, thus conditioning nocturnal. In addition, this negative airway pressure is also associated with narrowing of the Superior Airway during inspiration, which affects the esophagus. (18)
During the expiration the negative pressure is released, which increases the probability of suffering from gastroesophageal reflux.
The micro awakenings occur after hypoxemia, because the neurological centers of the central system detect the desaturation of oxygen in the blood and emit an immediate response through the efferent pathways. The micro-awakenings return the subject to the physiological conditions of wakefulness, recovering the phasic activity of the Upper Airway and causing loud noises, ending apnea, preventing death, but interrupting and altering the sleep process, which prevents adequate night rest, resulting in drowsiness daytime, fatigue, attention problems and concentration. All these symptoms may favor the depressive tendency in patients, although, for the moment, it has not been able to show that the syndrome acts as a factor in its appearance. (19)
The mandibular advancement devices have proven effective for several years in the treatment of snoring and OSA, but only with the algorithm used by the Meser ® Software, can intra-articular compression in the TMJ be avoided, avoiding this It forms the resorption of the heads of the condyles and the incorrect displacement of the soft articular intra-articular components, which can then generate disorders in the ear, such as: tamponade, tinnitus, dizziness, earache. (20)
References
- Velayos JL. “Medicina del sueño: enfoque multidisciplinario”. Madrid: Editorial Medica Panamericana (2009).
- Carlos Villafranca F., et al. “Tratamiento de la apnea obstructiva del sueño con posicionadores mandibulares”. RCOE 7.4 (2002): 379-86.
- Duthie J., et al. “A Longitudinal Study of Normal Asymmetric Mandibular Growth and Its Relationship to Skeletal Maturation”. American Journal of Orthodontics and Dentofacial Orthopedics 132.2 (2010): 179-184.
- Neto GP., et al. “Changes in the Masticatory Cycle After Treatment of Posterior Crossbite in Children Aged 4 to 5 Years”. American Journal of Orthodontics and Dentofacial Orthopedics 131. 4 (2007): 464-472.
- Cartwright RD., et al. “The Effects of Sleep Posture and Sleep Stage on Apnea Frequency”. Sleep 14.4 (1991): 351-353.
- “Is the sleep apnea/hypoapnea syndrome inherited?” Thorax 7 (1993): 719-721.
- H G Colt., et al. “Hypoxemia vs Sleep Fragmentation as Cause of Excessive Daytime Sleepiness in Obstructive Sleep Apnea”. Chest 100.6 (1991): 1542-1548.
- N J Moser., et al. “What Is Hypopnea, Anyway?” Chest 105.2 (1994): 426-428.
- Hoffstein V., et al. “Flow-volume Curves in Snoring Patients With and Without Obstructive Sleep Apnea”. The American Review of Respiratory Disease 139.4 (1989): 957-960.
- Terán Santos J., et al. “The Association Between Sleep Apnea and the Risk of Traffic Accidents. Cooperative Group Burgos-Santander”. The New England Journal of Medicine 340.11 (1999): 847-851.
- Browman CP., et al. “Obstructive Sleep Apnea and Body Weight”. Chest 85.3 (1984): 435-436.
- Orr WC., et al. “Hypersomnolent and nonhypersomnolent patients with upper airway obstruction during sleep”. Chest 75.4 (1979): 418-422.
- M Atkins., et al. “Nasal resistance in obstructive sleep apnea”. Chest 105.4 (1994): 1133-1135.
- “American Thoracic Society. Indications and standards for cardiopulmonary sleep studies”. The American Review of Respiratory Disease 139.2 (1989): 559-568
- American Sleep Disorders Association. “Practice parameters for the indications for polysomnography and related procedures”. Sleep 20.6 (1997): 406-422.
- Harman EM., et al. “The effect of weight loss on sleep disorder breathing and oxygen desaturation in morbidly obese men”. Chest 82.3 (1982): 291-294.
- Surta PM., et al. “Changes in breathing and pharynx after weight loss in obstructive sleep apnea”. Chest 92.4 (1987): 631-637.
- Sugerman HJ., et al. “Long term effects of gastric surgery for treating respiratory insufficiency of obesity”. The American Journal of Clinical Nutrition 55.2 (1992): 597-601
- Pevernagie DA., et al. “Effects of body position on the upper airway of patients with obstructive sleep apnea”. American Journal of Respiratory and Critical Care Medicine 152.1 (1995): 179-185.
- Nasal CPAP compliance therapy for sleep apnea. San Francisco (1993).
- Keenan SP., et al. “Long-term Survival of Patients With Obstructive Sleep Apnea Treated by Uvulopalatopharyngoplasty or Nasal CPAP”. Chest 105.1 (1994): 155-159.
- R W Riley., et al. “Maxillofacial Surgery and Nasal CPAP. A Comparison of Treatment for Obstructive Sleep Apnea Syndrome”. Chest 98.6 (1990): 1421-1425.
Citation:
Roberto Daniel Mesas and Eduardo Alejandro Seguetti. “Efficacy of Intraoral Plates in the Treatment of Snoring and OSA”. Oral Health and Dentistry 4.2 (2020): 49-58.
Copyright: © 2020 Roberto Daniel Mesas and Eduardo Alejandro Seguetti. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.







































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.