Research Article
Volume 1 Issue 2 - 2017
Relationship between Refractive Error and Ocular Shape in Ghanaian Adults
1University of Cape Coast, Cape Coast, Ghana
2National Assembly Clinic, Abuja, Nigeria
3Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
4St Thomas Eye Hospital, Accra, Ghana
2National Assembly Clinic, Abuja, Nigeria
3Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
4St Thomas Eye Hospital, Accra, Ghana
*Corresponding Author: Andrews Nartey, St. Thomas Eye Hospital, Accra, Ghana.
#Corresponding Author: Phyllis Austin, University of Cape Coast, Cape Coast, Ghana.
Received: April 29, 2017; Published: May 10, 2017
Abstract
Background: The peripheral optics of the eye underpins changes in retinal shape associated with refractive errors. This study sought to determine the relationship between ocular shape and refractive error in Ghanaian adults.
Method: In this descriptive cross-sectional study, ocular shape was assessed by measuring relative peripheral refractive error (RPRE) of the right eye of 6 myopic, 6 hyperopic and 6 emmetropic adults aged 18 to 25 years as they viewed targets from a distance of 4 meters. Using the Shin-Nippon auto refractor, the relative peripheral refractive error was calculated as the difference between the central spherical equivalent refraction and the peripheral refraction along the horizontal meridian and towards the nasal (N) and temporal (T) regions. The nasal-temporal angles considered in this study were 10º, 20º and 30º giving rise to N10º, N20º, N30º, T10º, T20º and T30º retinal eccentric positions. Data was analysed using Statistical Package for Social Sciences version 20 as well as Excel Statistical Package, and the level of significance was set at a p-value of 5%.
Results: Myopic adults showed a relative hyperopic defocus in the peripheral retina, hyperopic eyes had a relative myopic defocus at the periphery and emmetropic eyes had a relatively flat profile. There was nasal-temporal symmetry seen within each refractive error group with p-values of myopia (p = 0.302), hyperopia (p = 0.555) and emmetropia (p = 0.404). Against-the-rule astigmatism increased with increasing retinal eccentricity and there was no significant difference among the refractive error groups’ at all eccentric positions. Oblique astigmatism, however, differed significantly among the refractive error groups at the temporal 30º, eccentric position (p = 0.037) while the other retinal positions showed no statistically significant difference.
Conclusion: Adult myopic eyes have a prolate (less oblate) shape, adult hyperopic eyes have a more oblate shape and adult emmetropic eyes have a relatively spherical shape. The findings of this study corroborates other papers in extant literature whilst contradicting others. The need for a flurry of research in this area, using robust methodological approaches, is highly recommended.
Keywords: Relationship; Refractive error; Ocular shape; Ghanaian adults
Abbreviations: ANOVA: Analysis of Variance; E: Spherical Equivalent Refraction; J45: Oblique Astigmatism; J180: Horizontal Astigmatism; KNUST: Kwame Nkrumah University of Science and Technology; RPRE: Relative Peripheral Refractive Error; SD: Standard Deviation
Introduction
Refractive error is a condition of the eye in which light rays from optical infinity are not brought to a focus on the retina when accommodation of the eye is fully relaxed. The eye with a refractive error is termed ametropic while the eye without a refractive error is termed emmetropic. In categorizing ametropia by type, we have myopia, hyperopia and astigmatism. Myopia is a condition in which with accommodation fully relaxed, light rays coming from infinity converge to a focus in front of the retina. Hyperopia on the other hand is a condition in which parallel rays of light converge behind the retina with accommodation fully relaxed [1].
Astigmatism is a refractive condition in which the eye’s optical system is incapable of forming a point image for a point object. This is because the refracting power of the optical system varies from one meridian to another. In regular astigmatism, the meridian of greatest refraction and the meridian of least refraction are 90 degrees apart. The amount of astigmatism is equal to the difference in refracting power of the two principal meridians [2].
Refractive errors can be measured both centrally and peripherally [3]. Central refraction involves taking the on-axis refractive value of the eye fixating a set target and with the head in the primary position of gaze [3]. Peripheral refraction involves measuring the off-axis refraction of the eye in horizontal and sometimes vertical meridians over a range of angles, using several modified refraction techniques [4].
The peripheral optics of the eye provides insight into changes in retinal shape associated with refractive errors. This concept has been supported by animal studies in which peripheral form deprivation and imposed local retinal defocus appear to induce central axial myopia [5].
So far, only a few studies have allowed inferences about the shape of the human eye. These studies used either imaging techniques such as radiography, magnetic resonance imaging, CT scans and X-rays that directly visualize the eye or optical methods that suggest eye shape indirectly based on peripheral refraction [6-9].
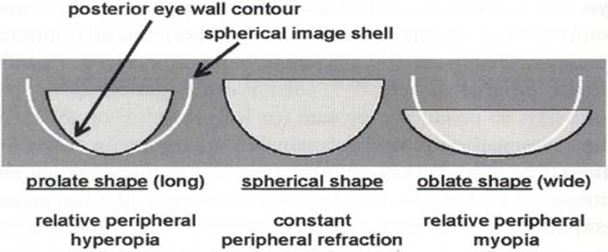
Three shapes are described for the human eye: spherical, prolate (elongated along the visual axis) and oblate (widened in the equatorial dimension). Most of the clinical reports that infer human eye shape from peripheral refraction make use of the assumption of the retinal contour being the only determinant of peripheral refraction as well as a spherically shaped image shell [9-10].
In a spherical eye, the eye wall parallels the spherical image shell. In a prolate eye, the eye wall is steeper than the spherical image shell. The image shell in the periphery becomes displaced progressively more posterior relative to the retinal position and the peripheral refraction becomes progressively more hyperopic than the central refraction with increasing distance from the fovea.
In an oblate eye, the eye wall curvature is flatter than that of the spherical image shell. The image shell in the periphery becomes displaced anteriorly relative to the retina and the refraction becomes more myopic in the periphery relative to that at the fovea [3]
Below is an image of the different ocular shapes as compared to the spherical image shell.
Previous studies have suggested that eye shape varies between individuals and that change in eye shape is associated with refractive errors [3,11]. Most of these studies also have established the relationship of central refraction to peripheral refraction and by implication, to eye shape establishing the fact that myopic eyes tend to have a prolate shape; hyperopic eyes tend to be oblate and emmetropic eyes assume a spherical eye shape [12-13].
The profile of refractive errors in the retinal periphery has since been plotted by several investigators with the general observation that whilst most of the emmetropic and hyperopic eyes demonstrate relative myopic peripheral defocus in the retinal periphery, most of the myopic eyes demonstrate relative hyperopic peripheral defocus [12, 14-17].
Animal studies involving infant monkeys have also showed that deprivation at the periphery could produce axial myopia even in the presence of clear images in the central retina [18] and it was suggested in a study that degradation of peripheral retinal image quality may contribute to the development of refractive errors such as myopia [19].
Degradation of the retinal image quality in the periphery is known to affect central refractive error development [20]. There is a hypothesis that relative hyperopic blur in the peripheral retina is a risk factor for the development and progression of central myopia in both children and adults [21]. With the rate of progression of myopia being different in different ethnic groups, eye shape could also be different in different ethnic groups. Most studies on refractive errors and ocular shape had been done with Caucasians, British and Asian ethnic groups but only a few of such studies had involved Africans. This gap in literature is the necessitating factor for the current study.
The purpose of this study was to determine the relationship between refractive error and ocular shape in Ghanaian adults.
Methodology
Study Participants: The subjects that participated in this study were students of the Kwame Nkrumah University of Science and Technology (KNUST) in Kumasi, Ghana. The College of Science of the KNUST was the study area from which the participating students, aged 18 to 25 years, were recruited.
Sampling size and Sampling Technique: A total of 18 students, comprising 6 students each who had myopia, hyperopia and astigmatism were purposively sampled for this research. Refractive status was defined as follows: myopia (-0.50D to -3.00D); emmetropia (-0.25D to +0.25D); hyperopia (+0.50D to +3.00D); astigmatism (less than 1.00 D); anisometropia (less than 1.00 D). The best-corrected visual acuity of any eligible participant was 20/20 or better. Any student with a history of any significant ocular disease was not allowed to partake in the study.
Data Collection Procedures: Data collected for this study was in three parts. The first part involved the participants’ demographic details and a comprehensive history taking. In the second part, a vision assessment comprising visual acuity, ophthalmoscopy and phoria/tropia test were performed in order to set the delimitations of the present study. Visual acuities of both eyes were measured at 4m under ambient light. Participants’ sphero-cylindrical refractive errors were measured by subjective refraction. The endpoint was determined using the traditional maximum plus/minimum minus with the optimum visual acuity.
Ocular integrity was assessed using a slit lamp bio microscope and ophthalmoscope. Both eyes were examined for external ocular disorders, corneal diseases, media opacities. Relative afferent pupillary defects and intraocular disorders such as vitreous and retinal changes, when detected, disqualified a student from partaking of the study.
Lastly, central refraction as well as peripheral refraction was measured on the right eye of all participants using Shin Nippon NV5001K Grand auto refractor. Before commencing the experiment, a calibration model eye provided with the instrument was used to authenticate the instrument’s precision and accuracy.
Only the right eye data were considered because Pearson correlation coefficient between both eyes was as high as 0.90. However, the left eye was occluded throughout the measurement. Non-cycloplegic subjective refractions were measured at 4m beginning with the on-axis measurement and then peripherally along the horizontal visual field at the 10, 20and 30° positions both nasally and temporally.
For measurements along the horizontal visual field, five refraction measurements were taken at each eccentric position and the average taken. The participants were asked to fixate peripheral targets using eye-turn rather than head-turn. The peripheral refraction was simplified by representing it as the spherical equivalent refraction (1/2cylinder + sphere) as in many other clinical writings [9,13]. Refractive error readings obtained as sphere (S), Cylinder (C) and Axis (ø) were converted into vector components [22] as follows:
Spherical Equivalent (E) = S + C/2
J180 = (-C cos 2ø)/2
J45 = (-C sin2ø)/2
J180 = (-C cos 2ø)/2
J45 = (-C sin2ø)/2
The E value was used to categorize the eyes into the three refractive groups: myopia, hyperopia and astigmatism.
The Relative Peripheral Refractive Error (RPRE) was calculated as the difference in E between the central and peripheral positions. That is, RPRE = Peripheral Refractive Error–Central Refractive Error.
Ethical Consideration: Ethical approval was sought from the Committee on Human Research, Publication and Ethics (CHRPE) of the KNUST. Informed consent was obtained from each subject after the nature of the experimental procedures had been explained. Students were assured of anonymity and confidentiality of all data collected. Participants were assured that they have the right to withdraw from the study at any stage and would not suffer any consequence for doing so. Finally, the research was conducted in accordance with the tenets of the declaration of Helsinki [23].
Data Analysis: Data was analysed using the SPSS version 20.0 and Excel statistical packages. The comparisons of mean ± SD of E, RPRE J180 and J45 were made using ANOVA. The level of significance was set at a p-value of 5%.
Results
Characteristics of Study Participants: With respect to age, there was no significant difference between the refractive error groups (p = 0.90) as well as between males and females within each refractive error group (p ≥ 0.92). The data showed a significant difference in mean central refraction between the three refractive error groups (p = 0.021); likewise between the males and females in the myopic group (p = 0.032). However, no significant difference between the males and females in the emmetropic (p =0.61) and hyperopic groups (p = .0.70) was recorded in this study. The details have been presented in Table 1 below.
| Characteristics | Myopia | Hyperopia | Emmetropia | P-value |
| Mean Age (± SD) | 19 ± 0.81 | 20.2 ± 0.63 | 19.66 ± 0.52 | 0.90 |
| Males | 19.34 ± 0.76 | 21± 0.58 | 19.33 ± 0.50 | 0.90 |
| Females | 18.66 ± 0.86 | 19.02 ± 0.68 | 19.99 ± 0.54 | 0.95 |
| P-value | 0.94 | 0.92 | 0.98 | |
| Mean central refraction (± SD) | -2.11 ± 0.61 | +1.05 ± 0.26 | 0.05 ± 0.10 | 0.02 |
| Males | -0.75 ± 0.54 | +1.03 ± 0.18 | 0.07 ± 0.09 | 0.03 |
| Females | -2.16 ± 0.68 | +1.07 ± 0.34 | 0.03 ± 0.11 | 0.02 |
| P-value | 0.032 | 0.70 | 0.61 |
Table 1: Participants’ Characteristics in Relation to Refractive Error Groups.
Refractive Profile of the Refractive Error Groups: The RPRE profile of the myopia group showed an increase in relative hyperopic defocus from the on-axis position in all degrees of eccentricities. Repeated measures ANOVA showed no significant difference between the temporal and nasal retinas (p = 0.30) at all eccentricities.
The RPRE profile of the emmetropia group showed a relatively flat profile with a relative 0 ± 0.05D defocus from the on-axis position in all degrees of eccentricities. There was no significant difference in the RPRE profile between the nasal and temporal retinas (p = 0.40) at all eccentricities.
The RPRE profile of the hyperopia group showed an increase in relative myopic defocus from the on-axis position in all degrees of eccentricities. Comparison showed a nasal-temporal symmetry (p = 0.55) at all eccentricities.
With the level of significance set at p < 0.05, repeated measures ANOVA revealed that there was a significant difference between the refractive error groups’ at all eccentric positions. T30º (F 2, 12 = 11.107, p = 0.002); T20º (F 2, 12 = 5.688, p = 0.018); T10º (F 2, 12 = 6.195, p = 0.014); N10º (F 2, 12 = 34.101, p = 0.000); N20º (F 2, 12 = 45.840, p = 0.000); N30º (F 2, 12 =19.603, p = 0.000).
All the refractive error groups showed an increase in off-axis astigmatism in the horizontal meridian. There was a relative negative defocus from the central location to peripheral retinal locations in both temporal and nasal fields indicating a direct proportionality between against- the-rule astigmatism and retinal eccentricity. The central on-axis locations of all refractive groups showed a positive J180 orientation indicating a with-the rule astigmatism. ANOVA showed that there was no significant difference between the three refractive error groups.
J45 vector represents oblique astigmatism (45º ± 15º to 135º ± 15º). The emmetropia group showed positive values along the temporal retina and nasal retina at all eccentricities. The myopia and hyperopic groups on the other hand showed negative values along the temporal and nasal retinas at all eccentricities. There was no significant difference between the three refractive error groups (p > 0.05) except at the temporal 30º eccentric position, which showed a significant difference (F 2, 12 = 4.416, p = 0.037). Table 2 below provides a detailed summary.
| Myopia | Temporal Retina | Central Retina | Nasal Retina | ||||
| -30° | -20° | -10° | 0° | +10° | +20° | +30° | |
| E | -1.35 ± 0.77 | -1.35 ± 1.26 | -1.65 ± 1.02 | -2.11 ± 0.68 | -1.68 ± 0.73 | -1.60 ± 0.80 | -1.65 ± 1.04 |
| J180 | -0.60 ± 0.65 | -0.25 ± 0.59 | -0.15 ± 0.25 | 0.04 ± 0.23 | -0.20 ± 0.30 | -0.35 ± 0.48 | -0.64 ± 0.43 |
| J45 | -0.23 ± 0.35 | 0.08 ± 0.26 | -0.02 ± 0.32 | -0.03 ± 0.18 | -0.18 ± 0.16 | -0.06 ± 0.36 | -0.25 ± 0.13 |
| RPRE | 1.13 ± 0.88 | 0.76 ± 0.95 | 0.46 ± 0.49 | 0.00 | 0.43 ± 0.19 | 0.51 ± 0.26 | 0.48 ± 0.45 |
| Emmetropia | |||||||
| E | 0.05 0.12 | 0.13 ± 0.16 | 0.20 ± 0.11 | 0.05 ± 0.12 | 0.00 ± 0.09 | 0.08 ± 0.19 | 0.05 ± 0.21 |
| J180 | -0.54 0.42 | -0.30 ± 0.37 | -0.19 ± 0.38 | 0.09 ± 3.9 | -0.15 ± 0.28 | -0.25 ± 0.47 | -0.50 ± 0.52 |
| J45 | 0.21 0.35 | 0.17 ± 0.37 | 0.06 ± 0.13 | -0.03 ± 0.14 | 0.04 ± 0.27 | 0.00 ± 0.24 | 0.01 ± 0.16 |
| RPRE | 0.05 ± 0.07 | -0.04 ± 0.06 | 0.02 ± 0.07 | 0.00 | -0.02 ± 0.05 | 0.03 ± 0.05 | 0.05 ± 0.07 |
| Hyperopia | |||||||
| E | 0.55 ± 0.27 | 0.63 ± 0.40 | 0.75 ± 0.18 | +1.05 ± 0.29 | 0.62 ± 0.24 | 0.35 ± 0.24 | 0.33 ± 0.25 |
| J180 | -0.55 ± 0.92 | -0.20 ± 0.56 | -0.10 ± 0.62 | 0.11 ± 0.23 | -0.25 ± 0.37 | -0.32 ± 0.64 | -0.55 ± 0.82 |
| J45 | -0.11 ± 0.23 | -0.01 ± 0.21 | -0.14 ± 0.15 | -0.02 ± 0.13 | -0.12 ± 0.08 | -0.11 ± 0.33 | -0.03 ± 0.47 |
| RPRE | -0.75 ± 0.20 | -0.51 ± 0.20 | -0.23 ± 0.22 | 0.00 | -0.36 ± 0.16 | -0.68 ± 0.19 | -0.80 ± 0.13 |
Table 2: Mean (± SD) E, J180, J45 and RPRE of the Refractive Error Groups.
Correlation between the Central and Peripheral Refractions of the Refractive Error Groups: The central and peripheral refractions were compared within each refractive error group to determine whether there was any correlation, and as well check if any significant difference existed between these two refractive values within the three groups. The peripheral refraction of the three refractive error groups showed a weak positive correlation with the central refraction indicating that an increase in central refraction leads to a corresponding increase in peripheral refraction. There was, however, no significant difference between the peripheral and central refractions of all the three groups as illustrated in Table 3 below.
| Myopia | Emmetropia | Hyperopia | |
| Correlation (r) | 0.4319 | 0.352 | 0.423 |
| P-value | 0.333 | 0.439 | 0.344 |
Table 3: Correlation between Central and Peripheral Refractions.
Differences between RPRE of Myopia in Males and Females: Table 4 below shows a comparison between RPRE of myopia in males
and females at the 10º, 20º and 30º of both nasal and temporal retinal eccentricities. The table shows a higher relative peripheral hyperopic
defocus in girls as compared to boys at all eccentricities (p ≥ 0.23).
| Gender | Temporal Retina Nasal Retina | ||||||
| -30 | -20 | -10 | 0 | 10 | 20 | 30 | |
| Males | 0.80 ± 0.72 | 0.53 ± 0.90 | 0.36 ± 0.50 | 0.00 | 0.38 ± 0.22 | 0.47 ± 0.29 | 0.43 ± 0.42 |
| Females | 1.46 ± 1.04 | 0.99 ± 1.00 | 0.56 ± 0.48 | 0.00 | 0.48 ± 0.16 | 0.55 ± 0.23 | 0.56 ± 0.48 |
Table 4: Mean ± SD of RPRE Values of Myopia in Males and Females.
RPRE of Participants in Relation to Average Duration of Spectacle Wear: A comparison between participants who wear their spectacle correction over 12 hours in a day and participants who wear their spectacle correction less than 12 hours in a day in relation to their ocular shape was assessed.
The data as shown in Table 5 below revealed that there was no significant difference in RPRE between the participants who wore their spectacles for more than 12 hours in a day and the participants who wore their spectacles for less than 12 hours in a day in both the myopic and the hyperopic groups.
| Refractive Error Group | Temporal Retina Nasal Retina | ||||||
| -30 | -20 | -10 | 0 | 10 | 20 | 30 | |
| Myopia | |||||||
| > 12 hrs/Day, N = 2 | 1.03 ± 0.80 | 0.75 ± 0.90 | 0.36 ± 0.40 | 0 | 0.43 ± 0.18 | 0.48 ± 0.0.23 | 0.51 ± 0.42 |
| < 12 hrs/Day, N = 4 | 1.23 ± 0.96 | 0.77 ± 0.86 | 0.56 ± 0.58 | 0 | 0.43 ± 0.20 | 0.54 ± 0.29 | 0.45 ± 0.48 |
| P Value | 0.721 | 0.905 | 0.747 | 0.957 | 0.832 | 0.819 | |
| Hyperopia | |||||||
| > 12 hrs/Day, N = 5 | -0.78 ± 0.18 | -0.48 ± 0.20 | -0.27 ± 0.22 | 0 | -0.39 ± 0.16 | -0.68 ± 0.19 | -0.78 ± 0.13 |
| < 12 hrs/Day, N = 1 | -0.72 ± 0.22 | -0.54 ± 0.17 | -0.19 ± 0.25 | 0 | -0.33 ± 0.20 | -0.65 ± 0.17 | -0.82 ± 0.11 |
| P Value | 0.897 | 0.793 | 0.706 | 0.825 | 0.910 | 0.843 | |
Table 5: RPRE and Duration of Spectacle Wear in Myopic and Hyperopic Eyes.
Discussion
The Relationship between Ocular Shapes and Refractive Errors: In line with most studies on the relationship between ocular shapes and refractive errors [14,24], this study on Ghanaian adults has shown that in the horizontal meridian, myopes have a less oblate shape with a relative hyperopic defocus from the on-axis retinal position towards the peripheral retina; hyperopes have a more oblate shape with a relative peripheral myopic defocus from the on-axis retinal position and emmetropes have a spherical shape with a relatively flat profile.
In contrast, other studies on Caucasian eyes had shown that myopic eyes have relative peripheral myopic defocus across the retina indicating an oblate shape for myopic eyes [12, 25-26]. This difference in findings could not be attributed to ethnicity differences as other studies on Caucasian eyes have shown results similar to the findings of the present study [14,20,27].
Again, this disparity could not have emanated from the means by which peripheral refraction was measured because this same method of aberrometry has been used in previous studies [26,28] and still reported that myopes had a relative hyperopic defocus. This contradictory finding could therefore be due to unexplained circumstances that are yet to be identified.
A number of studies have reported no significant difference between whites and East Asians as far as peripheral refraction profiles in the emmetropic and myopic groups are concerned [20,29].
Nasal- Temporal Symmetry within Refractive Error Groups: Nasal-temporal symmetry is seen in the RPRE profile of all the refractive error groups in the current study. This finding is in accordance with a study that reported a more symmetrical expansion of the posterior retinal contour in Chinese eyes [30]. It however contradicts the findings of a study among Chinese where a nasal-temporal asymmetry was seen, with the temporal retina showing a greater relative hyperopic defocus than the nasal retina [21]. These findings of nasal-temporal asymmetry have also been reported previously in Caucasian eyes [12,25].
Astigmatism within Refractive Error Groups: In this study, all refractive error groups showed a with-the-rule astigmatism with the central refraction. Off the visual axis, an against-the-rule astigmatism was reported, which increased with increasing retinal eccentricity. There was nasal-temporal symmetry within each refractive error group as well as symmetry between refractive error groups. This result is consistent with previous findings in the Caucasian population [12,14] and in Chinese eyes [25].
With oblique astigmatism J45, the three refractive error groups showed almost no oblique astigmatism at the on-axis refraction. J45 astigmatism however began to show along the retinal periphery with smaller shifts as compared to J180 astigmatism. There was no significant difference between the groups except at the temporal 30° of the retina. This difference at the temporal 30° might be ascribed to high variability in peripheral refraction [25] and ocular shape [31] usually seen in human eyes.
Correlation between the Central and Peripheral Refractions of the Refractive Error Groups: There was no significant difference between the central refraction and peripheral refractions in all the refractive error groups. This could be due to the fact that there was not enough statistical power to detect the difference between the central and peripheral refractions as a result of the small sample size, being a limitation factor in the current study.
Difference between RPRE of Myopia in Males and Females: From this study, there was a positive correlation between degree of central refraction and degree of relative peripheral hyperopic defocus in myopic individuals. Myopic females showed a higher relative hyperopic defocus than the males due to their higher central refraction. This substantiates the literature that females have a higher prevalence of myopic progression as compared to males [32,33].
Difference between RPRE of Asians and Africans: The RPRE of the myopia group in this study was lower than that reported in low myopia Chinese eyes [21]. This finding therefore supports the fact that Africans might have a lesser prevalence of myopia progression as compared to the Asian population [24].
Conclusion
From this study, there was no significant difference between the central refraction and peripheral refraction within the refractive error groups. The study further reported that myopes had a prolate or less oblate shape, hyperopes had a more oblate shape and emmetropes had a spherical shape. A nasal-temporal symmetry was seen within each refractive error group. The findings in this study also give credence to the hypothesis that astigmatism increases with increasing retinal eccentricity. The small sample size and the cross-sectional nature were the major limitations of this study. Hence, the need for a flurry of research in this area, using robust methodological approaches, is highly recommended.
References
- Grosvenor T and Grosvenor TP. “Primary Care Optometry. Anomalies of Refraction and Binocular Vision”. Elsevier Health Sciences (2007): 3-21.
- Bannon RE and Walsh R. "On Astigmatism, Parts 1 and 2”. American journal of optometry 22 (1945): 101-111, 162-179.
- Stone RA and Flitcroft DI. “Ocular shape and myopia”. ANNALS Academy of Medicine Singapore 33.1 (2004): 7-15.
- Fedtke C., et al. “A Review of Peripheral Refraction Techniques”. Optometry and Vision Science86.5 (2009): 429-446.
- Smith EL III., et al. “Relative Peripheral Hyperopic Defocus Alters Central Refractive Development in Infant Monkeys”. Vision Research 49.19 (2009): 2386-2392.
- Dellar JF., et al. “X-ray measurement of the diameters of the living eye”. Proceedings of the Royal Society of Medicine134.877 (1947): 456-467.
- Cheng HM., et al. “Shape of the Myopic Eye as Seen with High Resolution Magnetic Resonance Imaging”. Optometry and Vision Science69.9 (1992): 698-701.
- Dunne MCM. “A Computing Scheme for Determination of Retinal Contour from Peripheral Refraction, Keratometry and A-Scan Ultrasonography”. Ophthalmic and Physiological Optics15.2 (1995): 133-143.
- Mutti DO., et al. “Peripheral Refraction and Ocular Shape in Children”. Investigative Ophthalmology & Visual Science 41.5 (2000): 1022-1030.
- Asieh E., et al. “Cross-sectional Sample of Peripheral Refraction in Four Meridians in Myopes and Emmetropes”. Investigative Ophthalmology & Visual Science 52.10 (2011): 7574-7585.
- Hoogerheide J., et al. “Acquired Myopia in Young Pilots”. Ophthalmologica163 (1971): 209-215.
- Siedmann A., et al. “Peripheral Refractive Errors in Myopic, Emmetropic and Hyperopic Young Subjects”. Journal of the Optical Society of America 19.12 (2002): 2363-2373.
- Gustafsson J., et al. “Peripheral Astigmatism in Emmetropic Eyes”. Ophthalmic and Physiological Optics 21.5 (2001): 393-400.
- Atchison DA., et al. “Peripheral Refraction along the Horizontal and Vertical Visual Fields in Myopia”. Vision Research 46.8 (2006): 1450-1458.
- Atchison DA., et al. “Shape of the Retinal Surface in Emmetropia and Myopia”. Investigative Ophthalmology & Visual Science 46.8 (2005): 2698-2707.
- Charman WN and Jennings JAM. “Longitudinal Changes in Peripheral Refraction with Age”. Ophthalmic and Physiological Optics 26.5 (2006): 447-455.
- Millodot M. “Effect of Ametropia on Peripheral Refraction”. American journal of optometry and physiological optics 58.9 (1981): 691-695.
- Smith ELIII., et al. “Peripheral Vision Can Influence Eye Growth and Refractive Development in Infant Monkeys”.Investigative Ophthalmology & Visual Science 46.11 (2005): 3965-3972.
- Ehsaei A., et al. “The Effect of Instrument Alignment on Peripheral Refraction Measurements by Automated Optometer”. Ophthalmic and Physiological Optics 31.4 (2011): 412-420.
- Chen X., et al. “Characteristics of Peripheral Refractive Errors of Myopic and Non-myopic Chinese Eyes”. Vision Research 50.1 (2009): 31-35.
- Thibos LN., et al. “Power Vectors: An Application of Fourier analysis to the Description and Statistical Analysis of Refractive Error”. Optometry and Vision Science 74.6 (1997): 367-375.
- World Medical Association. “World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects”. JAMA 310.20 (2013): 2191-2194.
- Mutti DO., et al. “Refractive Error, Axial Length, and Relative Peripheral Refractive Error before and after the Onset of Myopia”. Investigative Ophthalmology & Visual Science 48.6 (2007): 2510-2519.
- Schmid GF. “Variability of Retinal Steepness at the Posterior Pole of Children”. Current Eye Research 27.1 (2003): 61-68.
- Mathur A and Atchison DA. “Peripheral Refraction Patterns out to Large Field Angles”. Optometry and Vision Science90.2 (2013): 140-147.
- Berntsen DA., et al. “Study of Theories about Myopia Progression (STAMP) Design and Baseline Data”. Optometry and Vision Science 87.11 (2010): 823-832.
- Kang P., et al. “Peripheral Refraction in Different Ethnicities”. Investigative Ophthalmology & Visual Science51.11 (2010): 6059-6065.
- Logan NS., et al. “Computation of Retinal Contour in Anisomyopia”. Ophthalmic and Physiological Optics15.5 (1995): 363-366.
- Verkicharla PK., et al. “Eye Shape and Retinal Shape and their Relation to Peripheral Refraction”. Ophthalmic and Physiological Optics 32.3 (2012): 184-199.
- Donovan L., et al. “Myopia Progression Rates in Urban Children Wearing Single-Vision Spectacles”. Optometry and Vision Science 89.1 (2012): 27-32.
- Jobke S., et al. “The Prevalence Rates of Refractive Errors among Children, Adolescents and Adults in Germany”. Clinical Ophthalmology 2.3 (2008): 601-607.
Citation:
Phyllis Austin., et al. “Relationship between Refractive Error and Ocular Shape in Ghanaian Adults”. Ophthalmology and Vision
Science 1.2 (2017): 55-63.
Copyright: © 2017 Phyllis Austin., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.