Case Report
Volume 1 Issue 3 - 2017
Acute Strabism Revealing Myasthenia Gravis
1Ophthalmology surgeon, Rodolfo Robles Valverde Hospital, Guatemala
2Neuro-ophthalmologist & strabismus surgeon Rodolfo Robles Valverde Hospital, Guatemala
3Retina-vitreous surgeon, Rodolfo Robles Valverde Hospital, Guatemala
2Neuro-ophthalmologist & strabismus surgeon Rodolfo Robles Valverde Hospital, Guatemala
3Retina-vitreous surgeon, Rodolfo Robles Valverde Hospital, Guatemala
*Corresponding Author: León-Nieto L, Ophthalmology surgeon, Rodolfo Robles Valverde Hospital, Guatemala.
Received: August 16, 2017; Published: September 22, 2017
Abstract
The case of a twenty two year old woman, who consulted for an acute deviation of the right eye, is presented. Physical examination of eyelids, pupillary reflexes, anterior segment and fundus were within normal limits. When evaluating extra-ocular motility, there is a limitation in adduction of the right eye and an alternating exotropia of 15 prismatic diopters in the primary position of the gaze. Imaging tests (orbital CT scan and brain MRI) showed no pathological changes. A neostigmine test was performed; which resulted being positive. The patient was managed with pyridostigmine and steroids, showing progressive improvement. The case is discussed because of the importance of differential diagnoses in the event of an acute ocular deviation.
Keywords: Acute strabismus; Myasthenia gravis; Neostigmine
Introduction
Acute strabismus is an acquired ocular deviation of recent onset (usually days or weeks of appearance). The clinical presentation varies according to the patient's age: with diplopia being the more prominent feature in adults, meanwhile in children it is the compensatory position of the head or the voluntary closure of one eye. In the early stages, an incomitant deviation will be observed. [1]
The purpose of presenting the following clinical case is to mention the possible differential diagnoses in the appearance of an acute ocular deviation, and the importance of systematically discarding the possible causes to specify a diagnosis with its appropriate management.
Clinical Case
A twenty-two-year-old female patient, originally from Guatemala, who consults for ocular deviation of the right eye and diplopia. The illness began three weeks prior to going to the Hospital, with dizziness and headache that worsen with time. On the fifth day the patient complains of diplopia when her gaze goes towards her left side. Ten days later she notices that the right eye is deviated outwards. Patient reports negative medical, ophthalmologic and family history.
During the ophthalmologic examination; the patient presents a visual acuity of 20/20 in both eyes, photo reactive pupils without a relative afferent pupillary defect; and an anterior and posterior segment that were within normal limits.
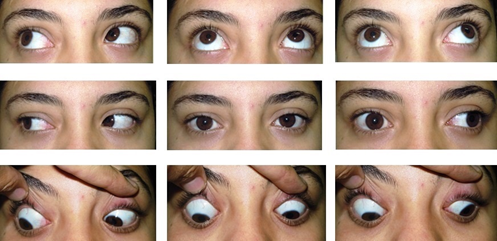
When evaluating the extraocular movements, there is a limitation to the adduction of the right eye and an alternating exotropia of 15 prismatic diopters in the primary position [Figure 1]. The Bielschowsky test is performed; the red-green filter shows a right hypertropia that increases with levoversion and inclination of the head to the left shoulder, suggesting a paralysis of the left superior rectus muscle.
Figure 1: Evaluation of extraocular muscles. Observe the limitation to the adduction of the right eye.
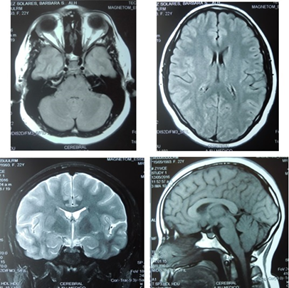
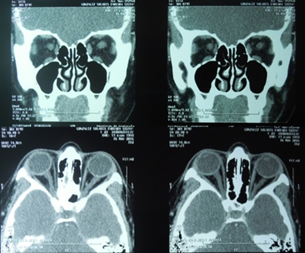
Due to the age of the patient and the absence of extraocular symptoms; imaging studies were requested to rule out occupational or demyelinating processes. Both Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) showed that the tissues presented no abnormalities. See figure 2 and 3.
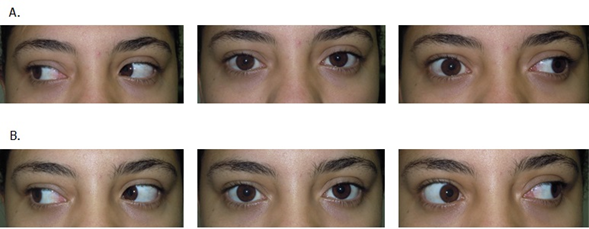
Fifteen days later, the patient reports that the diplopia has worsen; especially when reading or towards the end of the day. We decided to perform the Neostigmine test [Figure 4]; which thirty minutes later resulted positive; being compatible with the diagnoses of Myasthenia gravis.
Figure 4: Neostigmine test. A. Prior to injection: limitation to the adduction of the right eye.
B. Posterior to injection of neostigmine: improvement of the restriction to the adductive movement of the right eye.
B. Posterior to injection of neostigmine: improvement of the restriction to the adductive movement of the right eye.
Treatment was initiated with pyridostigmine and oral steroids; showing progressive improvement
Discussion
The characteristics of strabismus of acute and congenital etiology are compared in Table 1. [1]
| Chronic/Congenital Strabismus | Acute Strabismus | |
| Diplopia | Rare | Always present |
| Amblyopia | May be present | Absent |
| Abnormal Posture of the Head | May persist when covering the paretic eye due to secondary scoliosis and/or contraction of the neck muscles | Disappears when covering the paretic eye |
| Facial Asymmetry | May be present with torticollis | Absent |
| Contraction of the antagonist muscles during the test of forced ducciones | May be present | Absent |
| Old photographs | May present anomalous positioning | Negative |
Table 1:
In the presence of acute strabismus, the following differential diagnoses should be ruled out [2]:
- Cranial trauma: The most common condition affecting the superior oblique’s (IV cranial nerve palsy) due to its long trajectory. Increased hypertrophy is observed on the opposite side of the paralytic eye and the inclination of the head towards the same side of the paralysis.
- Increased intracranial pressure: It mainly affects the lateral rectus muscle (paralysis of the IV cranial nerve). Esotropia; which is greater in distant than near vision. Other symptoms include: papilledema, headache, transient vision loss, pulsatile tinnitus and diplopia.
- Post-viral disease: Preference for the lateral rectus muscle (VI cranial nerve palsy). Esotropia is present; which is greater in distant than near vision.
- Gradenigo Syndrome: Limitation to abduction with esotropia. Symptoms made include: otitis media, facial pain in the distribution of the trigeminal branches; and fever due to inflammation of the petrosal apex of the temporal bone.
- Occupational process of the central nervous system: Variable; signs and symptoms will depend on the location and dimension of the tumor. It is frequently associated with acute esotropia that varies depending on the location of the tumor. It may or may not have nystagmus or systemic neurological deficit.
- Internuclear ophthalmoplegia: It is characterized by paresis of ocular adduction in the horizontal gaze but not during convergence. It is the result of an injury in the medial longitudinal fasciculus. In young individuals, the disorder is usually caused by multiple sclerosis and may be bilateral. In the elderly, it is usually caused by a stroke and it is unilateral.
- Thyroid Ophthalmopathy/Myositis: It primarily affects the lower rectus> medial> superior> lateral muscles. Vertical and horizontal deviations will vary depending on the affected muscle. Eyelid retraction, palpebral delay in the downward glance, proptosis, optic neuropathy, and keratopathy due to exposure may be present. [2]
- Malformation of Arnold Chiari: Paralysis of the VI cranial nerve with involvement of the lateral rectus and esotropia. Vertical nystagmus, headache, dizziness, altered balance, divergent paralysis.
- Myasthenia gravis: A chronic neuromuscular disorder characterized by weakness and fatigability of voluntary muscles. [3] It involves the production of autoantibodies directed against musculoskeletal receptors, in the vast majority of cases affecting acetylcholine; but in some others, non-acetylcholine components of the postsynaptic muscular plate, such as the muscle-specific receptor tyrosine kinase (MuSK). [4] Ocular myasthenia (OM) is a subtype of MG with weakness that is clinically isolated to the periocular muscles, including the levator of the upper eyelid, the extraocular muscles, and orbicularis muscle.
It is estimated that the annual incidence is 4 to 11 cases per million, with a prevalence between 5 to 15 cases per 100,000 people. The disease predominantly affects women in the third and fourth decades, with a ratio of 3:2; However OM is more common in men. [5]
The characteristic of the clinical presentation is the fatigability and weakness that tend to worsen during the course of the day. Patients note that their weakness fluctuates from day to day or even from one hour to another, worsening with activity and improving with rest. Ocular weakness is the most common initial manifestation, with 75% of patients suffering from it. Approximately 40% to 50% of myasthenic patients initially will present purely with ocular symptoms. [6] About 30% to 40% will remain as an isolated ocular myasthenia, and 50% to 70% will progress to generalized myasthenia. Progression to generalized weakness in these cases usually occurs within two years after the onset of the disease. [7]
The diagnosis should be based on a history of fluctuating weakness, with findings that corroborate the fatigue during the examination. There are several ways to validate or confirm the clinical diagnosis.
- Clinical examination: Sleep test, ice test, Cogan test (a phenomenon caused by rapid muscle fatigability where the patient is asked to keep the gaze down for 10-20 seconds and then return to the primary position, observing how the upper eyelid rises and falls slowly but with repeated contractions before reaching a stable position). [7]
- Serum exams: Anti-acetylcholine antibody test whose specificity is not very clear but false positives are extremely rare; Muscle specific anti-thyrokinase antibodies (MuSK) can also be elicited.
- Pharmacological tests: Test of edrophonium (tensilon) with a sensitivity of 70-95% for generalized disease; a neostigmine test whose duration of effects is greater and allows diagnosis in 70% of cases. [8]
- Others: Electrophysiology has a sensitivity of 75% in patients with generalized Myasthenia gravis and less than 50% in ocular myasthenia. Single-fiber electromyography is a highly specialized technique with a sensitivity of 95-99% when performed on the appropriate muscles. The use of CT and MRI images is due to the probability of a thymoma in up to 10% of cases with Myasthenia gravis. [8]
The treatment can be divided into: 1) symptomatic, which basically includes cholinesterase inhibitors, 2) short-term therapy (plasmapheresis, intravenous immunoglobulin), and 3) long-term therapy (prednisone, azathioprine, mycophenolate, cyclosporine, tacrolimus, cyclophosphamide, and rituximab). [9]
Conclusion
In cases of acute strabismus, a long list of differential diagnoses is presented. It is important to have a complete history and clinical evaluation, which will help decide on the necessary complementary examinations that will be needed to confirm a diagnosis. The main differential diagnoses to be considered are: cranial trauma, increased intracranial pressure, post-viral disease, central nervous system occupational process, thyroid orbitopathy, Myasthenia gravis, internuclear ophthalmoplegia; among others. Complementary exams should include neuroimaging, laboratory tests and/or lumbar puncture depending on each individual case. In the case of the patient presented, due to her age and symptoms, it was decided to perform a brain MRI and a CT scan of orbits to rule out occupational or demyelinating processes. Because both were within normal limits, it was decided to perform a neostigmine test which was positive, corroborating the diagnosis of Myasthenia gravis. This case reaffirms the recommendation that, in the presence of acute ocular deviations, it is necessary to systematically rule out the possible causes for accurate diagnosis and treatment.
Acknowledgements
Special thanks to Dr. Mario Cahueque for his unconditional support in the realization of this article.
Special thanks to Dr. Mario Cahueque for his unconditional support in the realization of this article.
References
- Archer SM., et al. “Strabismus in infancy”. Ophthalmology 96.1 (1989): 133-137.
- Del Monte MA and Archer SM. “Atlas of pediatric ophthalmology and strabismus surgery”. American Academy of Ophthalmology (1993):
- Elias I Traboulsi., et al. Practical management of pediatric ocular disorders and strabismus”. A case based approach(2016):
- Merggioli M and Sanders D. “Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity”. The Lancet Neurology 8.5 (2009): 475-490.
- Meyer A and Levy Y. “Geoepidemiology of myasthenia gravis”. Autoimmunity Reviews 9 (2009): A383-386.
- Merggioli M and Sanders D. “Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity”. The Lancet Neurology 8.5 (2009): 475-490.
- Steinman L. “Immunogenetic mechanisms in myasthenia gravis”. Progress in Brain Research 84 (1990): 117-124.
- Chiu HC., et al. “Immunoglobulin allotypes in Caucasian and Chinese myasthenia gravis: differences from Japanese patients”. Journal of Neurology, Neurosurgery, & Psychiatry 51.2 (1988): 214-217.
- Gadient P., et al. “Juvenile myasthenia gravis: Three case reports and a literature review”. Journal of Child Neurology 24.5 (2009): 584-590.
Citation:
León-Nieto L., et al. “Acute Strabism Revealing Myasthenia Gravis”. Ophthalmology and Vision Science 1.3 (2017): 119-124.
Copyright: © 2017 León-Nieto L., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.