Research Article
Volume 1 Issue 3 - 2017
Journey of Removing Retained Intraocular Foreign Body-No Vitrectomy to Silicon Oil
Department of Ophthalmology, Gian Sagar Medical College and Hospital, Punjab, India
*Corresponding Author: Dr. Rajwinder Kaur, Department of Ophthalmology, Gian Sagar Medical College and Hospital, Punjab, India.
Received: September 17, 2017; Published: September 27, 2017
Abstract
We present a series of 20 cases with Penetrating injury with retained intraocular foreign body seen at the vitreo-retina clinic in a tertiary care Medical College and Hospital in North India from a period of June 2011 to January 2012. Based on our experience, we present the preoperative assessment, indication and technique of IOFB removal and document the one year visual outcome of eyes with IOFB.
Keywords: Foreign body; Phacoemusification; Vitrectomy; Intraocular lens; Visual acuity
Introduction
Ocular trauma caused by intraocular foreign body (IOFB) is one of the major reasons for visual impairment with approximately 40% of eyes involving open globe injuries harbours at least one IOFB. IOFBs are associated with acute and long-standing visual loss affecting children and young adults. Metallic foreign bodies (FBs) are present in 75% to 90% of eyes containing IOFBs, and 55% to 80% of all those are magnetic. [1-4]
Traumatic eye injuries with ferrous (magnetic) IOFB may result in significant loss of vision depending on certain factors like mechanism of injury, time of presentation, visual acuity on time of presentation, size of foreign bodies, location of foreign bodies and time of foreign body removal. [1-2] Occurrence of endophthalmitis and proliferative vitreoretinopathy (PVR) are vision threatening complications of retained IOFB –mediated injury. A ferrous intraocular foreign body cause deposition of iron molecules in the ocular tissues, and could ensue siderosis bulbi hence, timely removal is required at the earliest to prevent serious complications. [1,3] This article highlights our experience regarding the management of penetrating injury with retained intraocular foreign body.
Material and Methods
This retrospective, single institutional, interventional case study was conducted in a tertiary care referral centre in North India. All patients visiting the Retina Clinic at the tertiary care Medical College and Hospital in North India from June, 2011to January, 2012 with a diagnosis of penetrating injury with retained intraocular foreign body were enrolled in this study after they gave written informed consent. IOFB were defined as intraocular if all or part of the foreign material was within intraocular space at time of presentation. Patients with intra orbital or extra ocular IOFB were excluded. All patients were reviewed by one of the team members of the study on each follow up visit; the same team member reviewed the patient on each visit.
The Ocular Trauma Classification Group system for zone of entry was applied, with corneal entry referred to as zone one, entry within 5 mm posterior to the limbus as zone two and anything posterior to zone two as zone three. [5]
All records of patients were retrospectively reviewed for data regarding age and sex, mechanism, details of injury, visual acuity (VA) on presentation, anterior and posterior segment findings were noted. Surgical details including timing, type and number of procedure, intraoperative findings and timing of intravitreal drugs administration were also noted. Postoperative follow-up was included extending up to 1 year after injury when available.
After excluding life threatening conditions, twenty patients with penetrating injury and IOFB with or without traumatic cataract; with or without vitreo-retinal involvement were included in the study. Primary repair was done to restore the anatomy of globe along with intravitreal vancomycin 1 mg/0.1 ml and intravitreal ceftazidime 2.25 mg/0.1 ml along with dexamethasone 4 mcg/0.1 ml. In patients where the wound was self-sealed, were taken up for vitreo-retinal procedure directly. A detailed history regarding the mode of injury, visual acuity on presentation, time of presentation was taken; patients underwent a thorough ophthalmologic examination prior to the surgical procedure. Preoperative visual acuity, site of entry of foreign body (FB), involvement of lens, any associated signs of endophthalmitis and retinal detachment were also noted. Ultrasound B-Scan and/or X-ray of orbit were performed in all patients to locate and evaluate the IOFB and CT scan was done in few patients as it was costly. Patients with foreign body in the posterior segment were considered for general anesthesia. As all FBs were magnetic, for case, with involvement of lens, lensectomy was done and then foreign body was lifted to the pupilary plane using an intraocular magnet and then Utrata forceps was used to grasp the FB and gently remove it through the sclerocorneal tunnel. In patients where lens could be saved, foreign body was removed by enlarging one of the sclerotomy sites. A 360 degree belt buckle was put in all posterior segment foreign body. In patients where lens was all clear to allow the foreign body visualization, preoperative barrage laser around the foreign body was done followed by enlarging the sclerotomy site for removal of foreign body. After the removal of IOFB, thorough 360 degree peripheral examination with scleral depression was done to look for retinal tear, dialysis, retinal detachment or choroidal detachment. Endolaser and retinal endotamponade was used in cases with a retinal break and retinal detachment. In case where foreign body was intralenticular, a planned phacoemulsification with Intraocular lens (IOL) and foreign body removal was done.
Sclerotomies and conjunctiva were closed with 6-0 vicryl and 2 mg dexamethasone and 2 mg gentamicin sulphate were injected subconjunctivally. Postoperatively all patients received topical antibiotics and steroid for four weeks with gradual tapering. Oral ciprofloxacin 500 mg twice daily along with nonsteroidal anti-inflammatory agents was given in all cases with addition of systemic steroids in posterior segment foreign body. In each case recording of best corrected visual acuity (BCVA), intraocular pressure measurement, slit-lamp biomicroscopy and indirect ophthalmoscopy was done postoperatively. Cause of decreased vision was assessed considering site of entry of FB, site of lodgment of FB and postoperative complications like RD in each case.
Results
A total of twenty male patients were enrolled in this case study with a mean age of 26.5 years. Twelve patients were in the age group 20 to 40 years, three patients were less than 20 years and five patients were than 40 years. Ten patients had right eye and ten had left eye affected. The mean time of presentation to the ophthalmology department was 14.4 days. Two patients came to the hospital on the same day with hammer and chisel injury, nine patients presented within a week and seven patients came to the hospital within a month. Only two patients reported to the ophthalmology department after 1 month.
Nineteen patients presented with a positive history of metallic foreign body while doing hammer and chisel work. On examination, sixteen patients had visible entry wound; twelve patients had traumatic cataract and vitreous hemorrhage; seven patients had endophthalmitis; two had retinal detachment and one patient each had iris color change; iris prolapsed and double perforation. Twelve patients underwent X-ray orbit and fifteen patients had B-scan done which showed RIOFB.
The Ocular Trauma Classification Group system for zone of entry was applied, with corneal entry referred to as zone one, entry within 5 mm posterior to the limbus as zone two and anything posterior to zone two as zone three [Table 1]. In fifteen patients zone 1 was involved, zone 2 was involved in five patients.
| Zone | Number of eyes (%) | Visual Outcome | ||
| 20/20-20/60 | 20/80-20-120 | < 20/200 | ||
| Zone 1 | 15 (75) | 10 | 3 | 2 |
| Zone 2 | 5 (25) | 5 | ||
Table 1: The Ocular Trauma Classification Group system for zone of entry with final visual outcome.
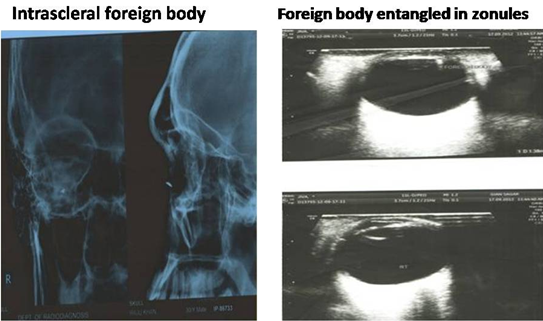
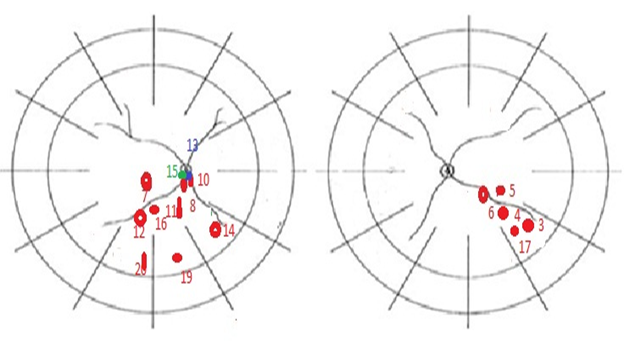
In majority of the cases (sixteen) foreign body was located on the retina and in one case it was subretinal with exit wound, intrascleral [Figure 1], intralenticular, entangled in the zonules [Figure 1]. Layout of site of lodgment of Retained Metallic Foreign Body is shown in Figure 2.
Site of Lodgment is an important factor for determining the visual outcome, patients in which the foreign body directly hits the macula had postoperative BCVA of counting fingers due to scarring at the macula.
Procedure Performed
In two patients no vitrectomy was done, as in one patient foreign body was into the sclera so only primary repair was done and intravitreal antibiotics were given. In second patient, foreign body was intralenticular so planned intralenticular foreign body removal was done with phacoemulsification and IOL implanatation. In twelve patients hybrid vitrectomy was done, in three cases sclerotomy was to remove the retained intraocular foreign body and in other nine cases, sclerotomy was enlarged for the silicon oil implantation. In six cases transconjunctival 23 G pars plana vitrectomy was done as the foreign body was removed after doing lensectomy saving the anterior capsular margin wherever possible to implant the IOL at later stage.
In two patients no vitrectomy was done, as in one patient foreign body was into the sclera so only primary repair was done and intravitreal antibiotics were given. In second patient, foreign body was intralenticular so planned intralenticular foreign body removal was done with phacoemulsification and IOL implanatation. In twelve patients hybrid vitrectomy was done, in three cases sclerotomy was to remove the retained intraocular foreign body and in other nine cases, sclerotomy was enlarged for the silicon oil implantation. In six cases transconjunctival 23 G pars plana vitrectomy was done as the foreign body was removed after doing lensectomy saving the anterior capsular margin wherever possible to implant the IOL at later stage.
One patient had IOL implanted in the same sitting, while in fourteen patients IOL was implanted in the second sitting. In these patients, phacoemulsification with IOL was done in 2; phacoemulsification with IOL and silicon oil removal was done in one case; secondary IOL was implanted on remnant anterior capsular margin in 7 cases; scleral fixated IOL with silicon oil removal was done in 2 cases. In five patients no IOL was implanted.
In 17 cases, 360 degree belt buckle was used to reduce the incidence of postoperative Retinal Detachment; Retinal tears were treated with endolaser. Nine cases were given internal tamponade in form of Silicon oil and seven cases were left under C3F8 tamponade. Intravitreal injections were given in 19 cases. Second surgery was done in 15cases, secondary IOL was implanted in eleven cases, IOL with silicon oil removal was done in three cases and silicon oil instillation was done for postoperative Retinal Detachment. All patients were followed for one year. Retina was attached in all case at one year follow up so declared successful anatomical outcome. Table 2 presents the comparison of initial and final visual acuity in patients.
| Visual Acuity | Preoperative (%) | Postoperative (%) |
| 20/20-20/60 | 2 (10) | 15 (75) |
| 20/80-20/120 | 3 (15) | 3 (15) |
| < 20/200 | 15 (75) | 2 (10) |
Table 2: Comparison of Initial and Final Visual Acuity.
Discussion
We retrospectively reviewed the visual outcome in 20 patients with penetrating intraocular injury with RIOFB. We found no association between injury and foreign body removal with visual acuity which is well supported by other studies. But a gap of more than two months between injury and vitreo-retinal procedure is mentioned a poor prognostic factor. Several studies have described an increased risk of endophthalmitis and proliferative vitreo-retinopathy in cases in which IOFB removal was delayed (greater than 24h after initial operation), and early removal of IOFB (first 24h after accident) has been recommended. [3, 6-7]
We performed 23 Gauge pars plana vitrectomy in six patients and all the patients had good visual outcome, speedy recovery, less postoperative astigmatism, less operative time and in cases where the lens is all clear, we did hybrid vitrectomy by enlarging one of the sclerotomy port for the foreign body removal.
Following IOFB removal, a thorough, 360 degree peripheral retinal examination with scleral depression is warranted to determine whether a retinal tear, retinal detachment or choroidal detachment is present. Tears are treated with endolaser and the eye is subsequently left under air tamponade. Retinal detachments are repaired and left under either C3F8 or SF6 tamponade. Several studies [8,9] have suggested a for prophylactic scleral buckle in retained IOFBs and posterior segment trauma. If multiple breaks present or PVR or perforating injury present, silicone oil may be instilled following IOFB removal. Retinal attachment was maintained, however in all cases at final follow up. Vitrectomy is often indicated for post-traumatic endopthalmitis, traumatic retinal detachment and perforating ocular injuries. The goals of vitrectomy in the setting include debulking vitreous toxins, microorganisms and inflammatory debris, obtaining intraocular fluid for microbiological analysis, as well as providing for injection of intravitreal antibiotics. [10,11] Repair of retinal detachment and removal of IOFBs are possible as needed. Silicone oil should be considered in most severe cases associated with endoplthalmitis because it not only provides effective endotamonade but also does not support microbial growth. [12,13]
The rate of preoperative retinal detachment associated with an IOFB has been reported at 31%. Intraocular foreign body removal associated with a retinal detachment can be extremely complicated, especially with subretinal IOFBs located away from the entry site of the IOFB. Postoperative IOFB-related retinal detachment can also contribute to poor visual outcome, with large IOFB and endophthalmitis as the strongest predictive factors. Late rhegmatogenous retinal detachments have been documented after posterior segment IOFB removal. [14]
Several studies have suggested a role for prophylactic scleral buckle in retained IOFBs and posterior segment trauma; however, further studies in this area are needed. If a choroidal haemorrhage has developed, a perforating injury is observed, or significant PVR is present, silicon oil may be instilled following IOFB removal. The presence of vitreous hemorrhage was the strongest independent risk factor for PVR formation; other risk factors included the presence of a long, posteriorly located wound and persistent intraocular inflammation. A recent retrospective case series described the use of primary silicone oil tamponade following IOFB removal in eyes with severe concomitant posterior pole injuries, including lacerations of the sclera, choroid and retina. [14]
Conclusion
According to our experience with RIOFB early presentation, site of entry, site of lodgment of foreign body, endophthalmitis, retinal detachment and PVR changes are the prognostic factors in determining the visual outcome. Transconjunctival pars plana vitrectomy has further revolutionized the visual outcome in posterior segment RIOFB. Scleral fixated IOL and Aniridia IOL further improved the visual outcome in treating Aphakia.
References
- McCabe CM., et al. “Surgical management of intraocular foreign bodies. In: Alfano PV, Ligett PE, eds. Vitreoretinal Surgery of the Injured Eye”. (1999): 257-70.
- Shock JP and Adams D. “Long-term visual acuity results after penetrating and perforating ocular injuries”. American Journal of Ophthalmology 100.5 (1985): 714-718.
- Thompson JT., et al. “Infectious endolphthalmitis after penetrating injuries with retained intraocular foreign bodies. National eye trauma system”. Ophthalmology 100.10 (1993): 1468-1474.
- Ahmadieh H., et al.“Vitrectomy in ocular trauma factors influencing final visual outcome”. Retina 13.2 (1993): 107-113.
- Pieramici DJ. “Open globe injuries are rarely hopeless. Managing the open globe calls for creativity and flexibility of surgical approach tailored to the specific case”. Review of Ophthalmology 12 (2005): 6.
- Jonas JB., et al. “Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies”. Ophthalmology107.5 (2000): 823-828.
- Jonas JB and Budde WM. “Early versus late removal of intraocular foreign bodies”. Retina 19.3 (1999): 193-197.
- Azad RV., et al. “Role of prophylactic scleral buckling in the management of retained intraocular foreign bodies”. Clinical & Experimental Ophthalmology 32.1 (2004): 58-61.
- Stone TW., et al.“Primary scleral buckling in open-globe injury involving the posterior segment”. Ophthalmology 107.10 (2000): 1923-1926.
- Mittra RA and Mieler WF. “Controversies in the management of open–globe injuries involving the posterior segment”. Survey of Ophthalmology 44.3 (1999): 215-25.
- Mieler WF and Mittra RA. “The role and timing of pars plana vitrectomy in ocular trauma”. Archives of Ophthalmology 115.9 (1997): 1191-1192.
- Azad R., et al. “Pars plana vitrectomy with or without silicone oil endotamponade in post-traumatic endophthalmitis”. Graefe's Archive for Clinical and Experimental Ophthalmology 241.6 (2003): 478-483.
- Ozdamar A., et al. “In vitro antimicrobial activity of silicone against endophthalmitis causing agents”. Retina 19 (1999): 122-126.
- Szurman P., et al. “Primary silicone oil tamponade in the management of severe intraocular foreign body injuries: an 8-year follow-up”. Retina 27.3 (2007): 304-311.
Citation:
Rajwinder Kaur., et al. “Journey of Removing Retained Intraocular Foreign Body-No Vitrectomy to Silicon Oil”. Ophthalmology
and Vision Science 1.3 (2017): 129-134.
Copyright: © 2017 Rajwinder Kaur., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.