Research Article
Volume 1 Issue 4 - 2017
Effect of the Duration of Eye Closure on Therapeutic Mydriasis
Eye Clinic, Volta River Authority Hospital, Akosombo, Ghana
*Corresponding Author: Felix Agyemang-Mireku, Volta River Authority Hospital, Akosombo, Ghana.
Received: November 06, 2017; Published: November 22, 2017
Abstract
Purpose: This study seeks to establish the effect of the duration of eye closure on therapeutic mydriasis.
Method: This was a prospective cross-sectional survey involving 60 participants who were put into two groups of 30. One drop of a combination of cyclopentolate 1% and phenylephrine 2.5% eye drop was instilled on both eyes of each participant. Group A was asked to close eyes for 5 minutes and group B for 20 minutes. The pupils were assessed for dilation with torchlight after one hour.
Results: Out of the 60 participants, majority 38 (63.33%) were females. The females dominated both Groups A 21 (70.0%) and B 17 (56.67%). Overall, the age group 51+ had the highest frequency 25 (41.67%). Full pupil dilation was achieved in 80.0% of participants in Group A as compared to 23.33% of those in Group B, despite the longer period of eye closure in Group B. There was a significant difference between Groups A and B in terms of degree of pupil dilation (p ≤ 0.05).
Conclusion: Shorter duration of eye closure during therapeutic pupil dilation is ideal in achieving maximal dilation. The long periods of eye closure that clients are subjected to in eye clinics needs to be avoided.
Keywords: Mydriasis; Miosis; Phenylephrine; Cyclopentolate; Sphincter pupillae; Ciliary muscles; Parasympatholytic; Sympathomimetic
Introduction
The dilation and contraction of the pupil of the eye has been extensively studied for so many years and it has been established that in addition to being influenced by light, a number of processes and activities influence the size of the pupil. This includes general arousal, the circadian rhythm, perception of emotional stimuli, pharmacological action of drugs, novelty detection and even cognitive processes, including memory operations (Sirois & Brisson, 2014; Laeng., et al. 2012; Pamplona., et al. 2009).
The largest change in pupil diameter is caused by light changes that elicit the pupil light reflex. Although the pupil diameter can vary between 2-8 mm (Pamplona., et al. 2009; Watson & Yellott, 2012), in normal light conditions it is around 3 mm (Wyatt, 1995). The normal pupil size in adults varies from 2 to 4 mm in diameter in bright light to 4 to 8 mm in the dark. The pupils are generally equal in size. They constrict to direct illumination (direct response) and to illumination of the opposite eye (consensual response). The pupil dilates in the dark. Both pupils constrict when the eye is focused on a near object (accommodative response). The pupil is abnormal if it fails to dilate to the dark or fails to constrict to light or accommodation.
Pupil size and dynamics are controlled by two synergistic pathways that operate on the smooth muscles of the pupil. The parasympathetic pathway is mediated by the Edinger Westphal oculomotor complex in the midbrain and innervates the sphincter which is the circular muscle responsible for constriction. The sympathetic pathway, mediated by the hypothalamus, innervates the radial dilator muscle of the iris responsible for dilation. The iris dilator fibres contain α-adrenergic sympathetic receptors that respond to changes in sympathetic tonus and changes in the blood level of circulating catecholamines.
Therapeutic mydriasis in ophthalmology is achieved with the use of mydriatics which comprise two groups of drugs: parasympatholytic and sympathomimetic. The parasympatholytic causes pupillary dilatation and paralysis of accommodation by rendering the sphincter pupillae and ciliary muscles insensitive to acetylcholine. Parasympatholytic drugs include atropine, tropicamide, cyclopentolate and homatropine. The sympathomimetic imitates or potentiates the action of adrenaline and produce pupillary dilatation but no cycloplegia. These drugs potentiate the action of parasympatholytic drugs. Sympathomimetic drugs include phenylephrine, hydroxyl amphetamine and ephedrine. Most mydriatics have different duration of action with some reaching their maximal effect by 30 to 60 minutes, although in children and people with deeply pigmented irides, this may take longer. A combination of the two groups of mydriatics is commonly used to achieve faster mydriasis.
It is a common practice for clinicians to instruct clients to close eyes for varying periods, till they are attended to, after instillation of mydriatics. The general belief is that longer eye closure helps to achieve better dilation. This is however not backed by research to the best of our knowledge. This study therefore seeks to establish the effect of the duration of eye closure on therapeutic mydriasis.
Materials and Methods
This study was a prospective cross-sectional survey conducted at the eye unit of the Volta River Authority Hospital, Akosombo. The study included 60 participants who were recruited for the study after their consent had been sought. These were clients whose eyes needed to be dilated for examination. The participants were put into two groups of 30. Participants were also told they could withdraw from the study at any time. Clients with shallow anterior chamber were excluded from the study. The study and the data collection scheme were approved by the eye clinic in-charge and carried out in accordance with the tenets of the declaration of Helsinki.
Baseline horizontal pupillary diameter of each participant was observed under the maximum illumination of torchlight before the instillation of the mydriatics. One drop of a combination of cyclopentolate 1% and phenylephrine 2.5% eye drop was instilled on both eyes of each participant. Group A was asked to close eyes for 5 minutes and group B for 20 minutes. The pupils were then assessed for dilation with torchlight after an hour.
Data was analysed with Microsoft Excel (2016; Microsoft, Redmond, WA) and SPSS version 23.0 (IBM Corporation, Armonk, NY, USA). The results were presented in graphs and tables. Categorical variables were tested employing Pearson’s Chi square test. A p value ≤ 0.05 was considered statistically significant.
Results
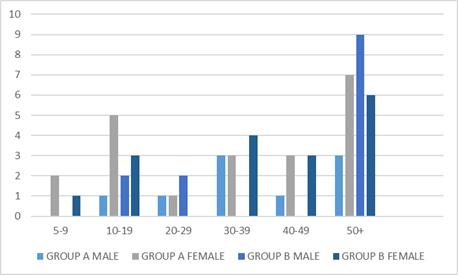
Out of the 60 participants, majority 38 (63.33%) were females. The females dominated both Groups A 21 (70.0%) and B 17 (56.67%). Overall, the age group 51+ had the highest frequency 25 (41.67%). This age group was dominant in both Groups A and B. The demographic characteristics are illustrated in table 1 and figure 1.
| Age | Sex (group a) | Sex (group b) | ||
| Male | Female | Male | Female | |
| 5-9 | 0 | 2 | 0 | 1 |
| 10-19 | 1 | 5 | 2 | 3 |
| 20-29 | 1 | 1 | 2 | 0 |
| 30-39 | 3 | 3 | 0 | 4 |
| 40-49 | 1 | 3 | 0 | 3 |
| 50+ | 3 | 7 | 9 | 6 |
| Total | 9 | 21 | 13 | 17 |
Table 1: Age and sex distribution of participants.
Majority of the participants in Group A (80.0%) had fully dilated pupils at the end of the one hour after closing eyes for five minutes. 20.0% of the participants had semi-dilated pupils. None of the participants in this group had undilated pupils at the end of the five minutes. This is illustrated in table 2.
| Degree of dilation | Frequency (%) |
| Fully dilated | 24 (80.0) |
| Semi-dilated | 6 (20.0) |
| Total | 30 (100.0) |
Table 2: Degree of dilation in Group A.
For participants in Group B, majority (40.0%) had slightly dilated pupils followed by 30.0% with semi-dilated pupils, then 23.33% achieving full pupil dilation. 6.67% of the participants in Group B had undilated pupils at the end of the one hour after twenty minutes of eye closure. This is highlighted in table 3.
| Degree of dilation | Frequency (%) |
| Fully dilated | 7 (23.33) |
| Semi-dilated | 9 (30.0) |
| Slightly dilated | 12 (40.0) |
| Undilated | 2 (6.67) |
| Total | 30 (100.0) |
Table 3: Degree of dilation in Group B.
There was a significant difference between Groups A and B in terms of degree of pupil dilation (p ≤ 0.05). Participants in Group A achieved better pupil dilation than those in Group B. Full pupil dilation was achieved in 80.0% of participants in Group A as compared to 23.33% of those in Group B, despite the longer period of eye closure in Group B.
| Duration of eye closure | Degree of pupil dilation | |||
| Fully dilated (%) | Semi-dilated (%) | Slightly dilated (%) | Undilated (%) | |
| 5 minutes | 24 (80.0) | 6 (20.0) | 0 (0) | 0 (0) |
| 20 minutes | 7 (23.33) | 9 (30.0) | 12 (40.0) | 2 (6.67) |
Table 4: Comparison of the degree of dilation between Group A and Group B.
Discussion
A combination of cyclopentolate 1% and phenylephrine 2.5% induces mydriasis that is greater than that of either drug alone at its respective concentration. Mydriasis occurs within 10-20 minutes after single instillation of phenylephrine 2.5%. Cyclopentolate 1% has rapid onset with mydriasis reached within 10-30 minutes. A combination of these two drugs helps to achieve mydriasis within a shorter time.
Majority of the participants in Group A (80.0%) achieved maximal pupil dilation at the end of one hour after 5 minutes of eye closure. This is in contrast with what was observed in Group B, with 23.33% of respondents achieving maximal pupil dilation after 20 minutes of eye closure. The idea of eye closure is to prolong the contact time of the drug with the external eye thereby maximising the contact of the drug with the periocular tissues increasing absorption through the cornea. Also, eye closure is believed to avoid light interaction, as the largest change in pupil diameter is caused by light changes that elicit the pupil light reflex.
The significant difference observed between the two groups could indicate that longer periods of eye closure during therapeutic pupil dilation could lead to a reverse action as longer periods of eye closure may simulate sleep or cause clients to fall into temporal state of sleep. Form, extent, and duration of pupillary reflexes are influenced by the degree of tiredness, wakefulness, or excitement of the subject. Miosis during drowsiness and sleep relies on reduced inhibition of the oculomotor nucleus and, even more, on reduced sympathetic tone. For whatever reason a lack of sympathetic tone occurs, a poor response to anticholinergic mydriatics thus becomes the consequence. The pupil shrinks during deep sleep even after atropine. If the conditions of deep sleep, sedation or general anaesthesia are present and mydriasis needs to be maintained, an additional administration of a sympathomimetic compound is mandatory.
Another reason that could explain the smaller degree of pupil dilation in Group B is the probability that majority of participants in this group may have heavy pigmented irides (dark brown to black eyes). There is binding of the drug molecules to the pigment cells, which occurs in greater density in dark irides. This results in fewer drug molecules available to cause mydriasis. Heavily pigmented irides may therefore require more doses than lightly pigmented irides in order to achieve maximal pupil dilation.
Conclusion
It can be concluded from this study that, shorter duration of eye closure during therapeutic pupil dilation is ideal in achieving maximal dilation. The long periods of eye closure that clients are subjected to in eye clinics needs to be avoided. This would help relieve clients of the discomfort they have to endure.
In order to obtain greater degree of mydriasis, additional drop may be required or perhaps a higher percentage of the drug could be used. However, care should be taken not to exceed the recommended daily dosage. Eye colour needs to be considered in therapeutic pupil dilation as eyes with heavily pigmented irides may require extra dose.
References
- Craig EW and PG Griffiths. “Effect on mydriasis of modifying the volume of phenylephrine drops”. British Journal of Ophthalmology75.4 (1991): 222-223.
- Elton M. “Use of mydriatic-cycloplegic drugs”. The Pharmaceutical Journal(2000):
- Laeng B., et al.“Pupillometry: A Window to the Preconscious?” Perspectives on Psychological Science 7.1 (2012): 18-27.
- Loewenfeld IE and Lowenstein O. “The pupil: anatomy physiology and clinical applications”. Wayne State University Press, Detroit (1993):
- Nagataki S and S Mishima. “Pharmacokinetics of instilled drugs in the human eye”. International Ophthalmology Clinics20.3 (1980): 33-48.
- Pamplona VF., et al.“Photorealistic models for pupil light reflex and iridal pattern deformation”. ACM Transactions on Graphics 28.4 (2009): 1-12.
- Sirois S and Brisson J. “Pupillometry”. WIREs Cognitive Science5.6 (2014): 679-692.
- Watson AB and Yellott JI. “A unified formula for light-adapted pupil size”. Journal of Vision 12.10 (2012): 12.
- Wilson WS. “Mydriatic-cycloplegic drugs”. The Pharmaceutical Journal (2000):
- Wyatt HJ. “The form of the human pupil”. Vision Research 35.14 (1995): 2021-2036.
Citation:
Felix Agyemang-Mireku and Alphonsus Walaman-Iba Kuuso. “Effect of the Duration of Eye Closure on Therapeutic Mydriasis”.
Ophthalmology and Vision Science 1.4 (2017): 158-162.
Copyright: © 2017 Felix Agyemang-Mireku and Alphonsus Walaman-Iba Kuuso. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.