Case Report
Volume 1 Issue 4 - 2017
North Carolina Macular Dystrophy: Clinical Images and Review of Literature
VMMC and Safdarjung Hospital, New Delhi, India
*Corresponding Author: Anurag Narula, VMMC and Safdarjung Hospital, New Delhi, India.
Received: October 24, 2017; Published: November 22, 2017
Abstract
To report a case of North Carolina Macular Dystrophy and to discuss the literature pertaining to it.
Clinical data including medical history, findings on physical examination and local examination were recorded for a 32 year old female, case of Fundus Flavimaculatus. No treatment was advised and patient was called for regular follow-up to cater for low vision aids if required in the future.
Best corrected Visual acuity of the patient remained constant at 20/40 for a period of one year with the patient being on 3monthly follow up.
No particular or specific treatment is available for this fundus dystrophy. Frequent follow-ups may help diagnose and manage associated CNVM at the earliest. The only modality available in the form of low vision aids for advanced disease.
Keywords: North Carolina; Macular Dystrophy
Introduction
A 32 year old female, presented to us with progressive vision deterioration since last 18 months to the present status of vision of vision being 20/40(best corrected in both eyes).
Case History
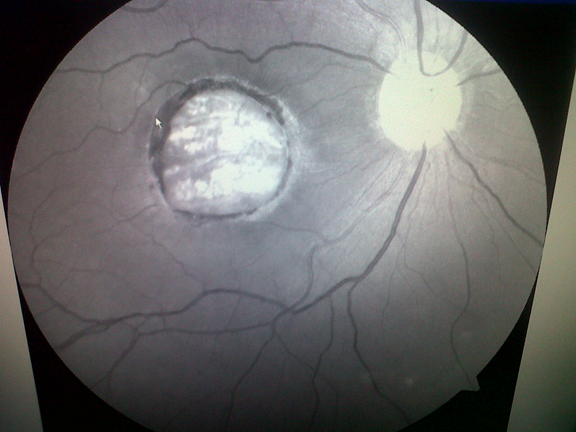
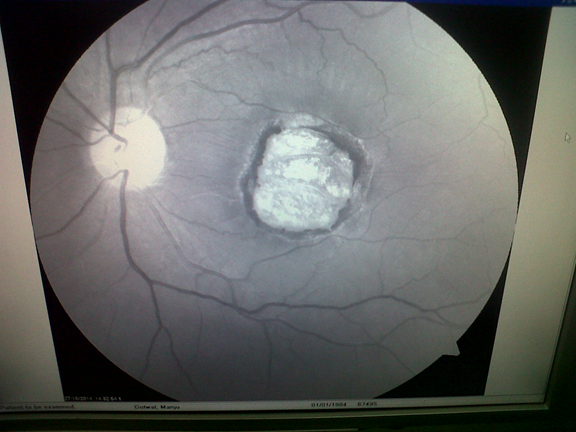
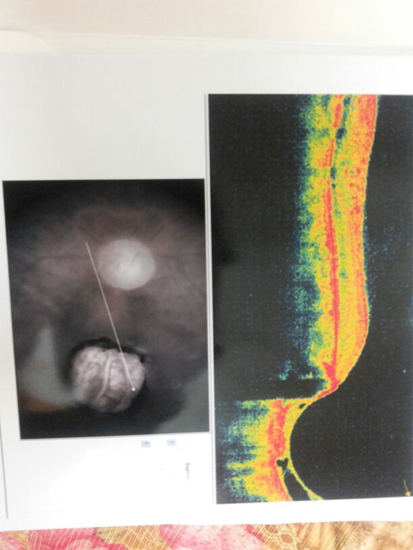
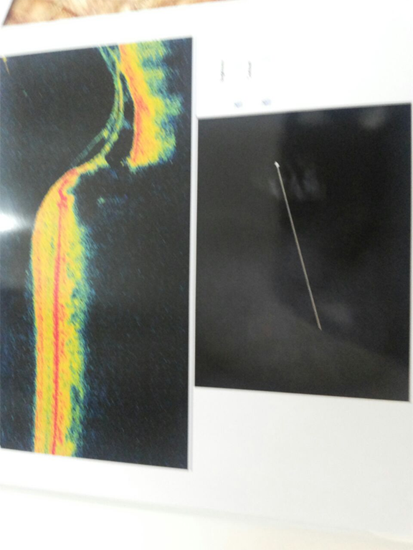
General physical examination and systemic examination was unremarkable. On examination best corrected visual acuity was 20/40 both eyes, with normal anterior segment examination. On fundus examination the posterior pole showed an area of well-delineated chorioretinal degeneration with hyperpigmentation at the border of the lesion. A central crater-like lesion affecting all retinal layers, as well as the deep choroidal tissue was seen (Figure 1 and 2). Fluorescein angiography revealed window defect seen as hyperfluorescence and loss of choroidal tissue seen as hypofluorescence-almost total absence of fluorescence.
Provisional Diagnosis of North Carolina Macular Dystrophy was made.
No treatment was advised and patient was called for regular follow-up to cater for low vision aids if required in the future and for earlier diagnosis and management of CNVM if associated.
Best corrected Visual acuity of the patient remained constant at 20/40 for a period of one year with the patient being on 3monthly follow up.
Discussion
North Carolina macular dystrophy is characterized by central macular defects that are present at birth but rarely progress. The fundus findings are highly variable and are usually more dramatic than expected from the visual acuity, which ranges from 20/40 to 20/200, with an average around 20/50. The clinical findings have been classified into different grades: In Grade I, fine drusen-like lesions at the level of the retinal pigmented epithelium are found in the central macular area. Grade II exhibits central confluent drusen with or without pigmentary changes, retinal pigment epithelium atrophy, disciform scar formation or neovascularization. Grade III is characterized by a well-delineated chorioretinal degeneration with hyperpigmentation at the border of the lesion. A central crater-like lesion that affects all retinal layers, as well as the deep choroidal tissue, is a typical finding. It is surrounded by an elevated ridge, which is 3-4 disc diameter is diameter. Color vision and electrophysiological testing are usually normal. [1,2]
Although first described in a 4 generation North Carolina family, it has since been found in a variety of ethnic groups and geographic locations. [3]
No general systemic manifestations are associated with North Carolina macular dystrophy. [3]
North Carolina macular dystrophy is an autosomal dominant disorder with high penetration. The genetic locus for the disorder is designated MCDR1, for macular degeneration locus 1, and has been mapped to 6q14-q16.2. Candidate genes in this region have been screened for disease causing mutations, but none have been identified so far. The disorder was initially described in a family of Irish descent in North Carolina, and affected individuals have been identified in European, Asian and South American families as well. [4]
For patients with Grade II disease with choroidal neovascularization, standard treatment for neovascularization may be used. Low vision aids can be useful for other forms of the disorder with decreased visual acuity.
References
- Khurana RN., et al. “A reappraisal of the clinical spectrum of North Carolina macular dystrophy”. Ophthalmology 116.10 (2009): 1976-1983.
- Yang Z., et al. “Clinical characterization and genetic mapping of North Carolina macular dystrophy”. Vision Research. 48.3 (2008): 470-477.
- Small KW. “North Carolina macular dystrophy, revisited”. Ophthalmology 96.12 (1989): 1747-1754.
- Lefler WH., et al.“Hereditary macular dystrophy and amino-aciduria”. American Journal of Ophthalmology 71.2 (1971): 224-230.
Citation:
Anurag Narula., et al. “North Carolina Macular Dystrophy: Clinical Images and Review of Literature”. Ophthalmology and Vision
Science 1.4 (2017): 163-166.
Copyright: © 2017 Anurag Narula., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.