Case Report
Volume 2 Issue 3 - 2019
Traction and Ischemic Sickle Cell Maculopathy – Case Report
1Department of Ophthalmology, Clínica de Olhos Leitão Guerra (Salvador, Brazil)
2Post-graduation course, Bahiana’s School of Medicine and Public Health (Salvador, Brazil)
3Department of Ophthalmology, Hospital São Rafael (Salvador, Brazil)
2Post-graduation course, Bahiana’s School of Medicine and Public Health (Salvador, Brazil)
3Department of Ophthalmology, Hospital São Rafael (Salvador, Brazil)
*Corresponding Author: Ricardo Luz Leitão Guerra, Rua Catarina Paraguaçu, n08 – Graça, Salvador (BA) – Brazil.
Received: February 02, 2019; Published: February 14, 2019
Introduction
Sickle cell disease (SCD) is a genetic hemoglobinopathy that occurs due to a mutation, turning the normal hemoglobin (HbA) to sickle hemoglobin (HbS). [1] There are different genotypes for the SCD and the more frequently are the homozygous form (HbSS), also known as Sickle Cell Anemia, and the heterozygous form called SC disease, characterized by the combination of HbS to another pathological hemoglobin, the HbC. [1]
Intraocular findings in sickle cell disease (SCD) are described in the literature since 1937 [2] and, in 1971, Goldberg’s proposed the first sickle cell retinopathy classification based on peripheral vascular alterations that is still used as the gold standard classification.[3,4]
Posterior pole alterations in sickle cell retinopathy (SCR) includes tractional causes, such as epiretinal membranes (ERM) [5], and ischemic maculopathy [6]. The development of Spectral-Domain Optical Coherence Tomography (SD-OCT) enhanced the knowledge about several macular diseases [7] and, after the first description of SD-OCT findings in SCD patients [8], it has renewed the interest of studying sickle cell ischemic maculopathy (SCIM). [9-12]
We aim to describe a case of SCR presenting tractional maculopathy in one eye and ischemic maculopathy in the fellow eye. A retrospective case report was performed by reviewing medical records and imaging exams of one patient. The study protocol was approved by the Institutional Ethics Review Board of the Hospital São Rafael (CAAE: 14929313.4.0000.0048) and conducted by the Retina and Vitreous Service of the same institution in conjunction with the postgraduate course of the Bahiana’s Scholl of Medicine and Public Health.
Case Report
A 46-year-old man presented with a long standing history of decreasing visual acuity was referred for a vitreoretinal specialist evaluation. Medical history was positive for sickle cell anemia (HbSS). He denied any previous ocular treatment.
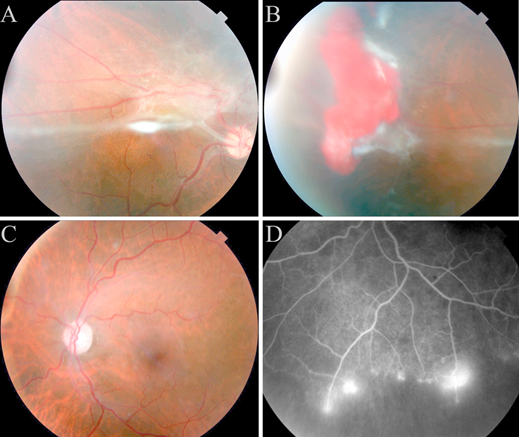
Best corrected visual acuity (BCVA) on presentation was counting fingers in the right eye (OD) and 20/200 in the left eye (OS). Anterior segment biomicroscopy and tonometry revealed no pathologic alterations. Funduscopic examinations of the OD revealed a thick epiretinal membrane (ERM) from the posterior pole to the temporal periphery (Figure 1A), peripheral ischemia and a solitary red mass in the retinal periphery suggestive of a hemorrhagic proliferative lesion (hemorrhagic sea fan) (Figure 1B). Funduscopic examination of the OS presented abnormal macular reflex, peripheral ischemia, but no sign of proliferative retinopathy was noticed (Figure 1C).
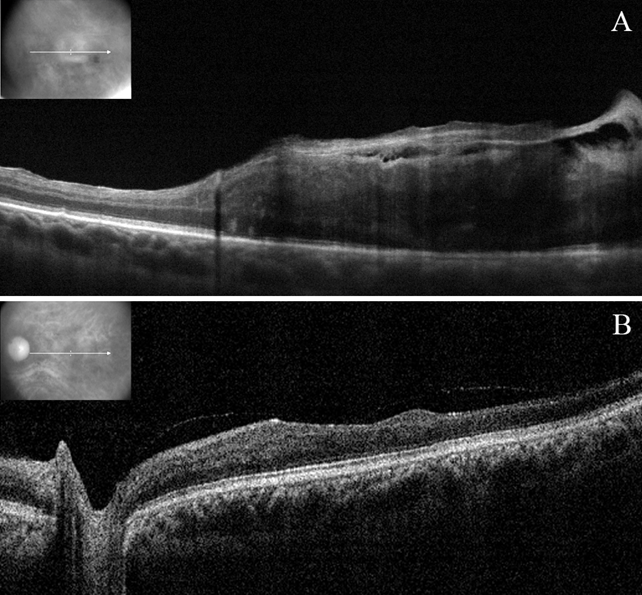
Fluorescein angiography (FA) was performed and revealed a small area of vascular proliferation on the inferior retina of the OS (Figure 1D). Spectral-domain optical coherence tomography (SD-OCT) showed a thick ERM causing a traction maculopathy in the OD (Figure 2A) and an important retinal thinning, mainly in the temporal area of the macula (Figure 2B).
The patient was referred for peripheral laser photocoagulation in both eyes and to vitreoretinal surgery (23 gauge sutureless vitrectomy) in the OD for treating the ERM.
Figure 1: A: Posterior pole of the right eye presenting a thick epiretinal membrane causing severe distortion of the anatomy. B: Temporal periphery of the right eye presenting a solitary red mass suggestive of an hemorrhagic proliferative lesion (hemorrhagic sea fan). C: Fundus photography of the posterior pole of the left eye. D: Fluorescein angiography of the left eye presenting peripheral neovascularization and ischemia.
Figure 2: A: Spectral-domain Optical Coherence Tomography (SD-OCT) of the right eye presenting macular distortion due to a thick epiretinal membrane. B: SD-OCT of the left eye showing a partially detached posterior hyaloid membrane and a diffuse decreased retinal thickness and a disorganization of the inner retinal structures, mainly in the temporal area.
Discussion
We presented a case of Sickle Cell Traction Maculopathy (SCTM) in one eye and SCIM in the fellow eye, documented by fundus photography, fluorescein angiography and SD-OCT. Both eyes presented proliferative SCR (stage 3 of Goldberg’s classification).
Both traction and ischemic macular involvement in SCD are longstanding described in the literature. [5,6] Despite the macular microangiopathy, visual acuity (VA) might not be affected and can remain 20/20 until extensive central involvement. [13] Color vision test [14], contrast sensitivity [15] and visual field are more sensitive tests than VA for macular function evaluation in sickle cell disease patients. In the presented case, the visual acuity was severe affected in both eye.
Since Goldberg’s classification it has been the gold standard for staging and guiding treatment of peripheral retinal disease. [3,4] Peripheral laser photocoagulation should be considered to prevent visual loss and vitreous hemorrhage, however the treatment does not stop the disease progression nor prevents new proliferations to occur. [16] Peripheral laser photocoagulation was indicated for both eyes of the presented patient.
ERM is an important cause of maculopathy in SCD patients, often related to proliferative SCR. [5] Surgical treatment was not recommended in the past due to possible surgical complications [5], however the evolution of the vitreoretinal surgery and the introduction of the small gauge vitrectomy had improved both functional and anatomical outcome in selected cases of SCR. [17] In the presented case, the severe decreased VA and the macular anatomical distortion were considered to decide for the surgery indication.
FA is the gold standard test for evaluating retinal vascular diseases and its application in SCR is longstanding described. [3] FA has been proved superior than clinical evaluation for detecting proliferative SCR. [18] Vascular tortuosity, non-perfusion areas and vascular proliferation can be found in the peripheral retina and, foveal avascular zone (FAZ) enlargement and irregularity can be found in the posterior pole. [3,18,19] In the presented case, the FA was able to detect a small vascular proliferation that was not detected during the clinical examination.
SD-OCT has been an important device in the current ophthalmology practice and helped understanding unknown features about macular alterations in SCD patients. [8,9,20] Temporal macular thinning of the inner retinal layers is the main SD-OCT finding in SCD and has been found even in asymptomatic patients. [9,20] Functional correlation of the thinned area and negative scotoma has been described, however the authors suggested that the macular thinning might occur before the onset of the functional impairment. [9]
Development of Optical Coherence Tomography (OCT)-based tests such as the previously mentioned SD-OCT and others such as OCT angiography and doppler OCT have been revolutionizing the ophthalmology practice and enhancing the knowledge about sickle cell retinopathy. New data from further studies are needed and might be able to determine risk factors and associations with a great potential to be applied as a biomarker for severe stages of retinopathy.
References
- Feroze KB and Azevedo AM. “Retinopathy, Hemoglobinopathies”. StatPearls Publishing (2018):
- Harden as. “Sickle cell anemia”. The American Journal of Diseases of Children54.5 (1937): 1045.
- Goldberg MF. “Classification and Pathogenesis of Proliferative Sickle Retinopathy”. American Journal of Ophthalmology 71.3 (1971): 649-665.
- Leitão Guerra RL and Salles C. “Sickle cell retinopathy diagnosis criteria and classification”. Journal of American Association for Pediatric Ophthalmology and Strabismus (2018):
- Carney MD and Jampol LM. “Epiretinal Membranes in Sickle Cell Retinopathy”. JAMA Ophthalmology 105.2 (1987): 214-217.
- Knapp JW. “Isolated macular infarction in sickle cell (SS) disease”. American Journal of Ophthalmology 73.6 (1972): 857-859.
- Kashani AH., et al. “Optical coherence tomography angiography: A comprehensive review of current methods and clinical applications”. Progress in Retinal and Eye Research 60 (2017): 66-100.
- Witkin AJ., et al. “Optical Coherence Tomography Demonstration of Macular Infarction in Sickle Cell Retinopathy”. JAMA Ophthalmology 124.5 (2006):746.
- Chow CC, et al.“Structural and functional correlation in sickle cell retinopathy using spectral-domain optical coherence tomography and scanning laser ophthalmoscope microperimetry”. American Journal of Ophthalmology 152.4 (2011): 704-711.
- Lim JI and Cao D. “Analysis of Retinal Thinning Using Spectral-domain Optical Coherence Tomography Imaging of Sickle Cell Retinopathy Eyes Compared to Age- and Race-Matched Control Eyes”. American Journal of Ophthalmology 192 (2018): 229-238.
- Lim WS., et al.“Retinal thickness measurements in sickle cell patients with HbSS and HbSC genotype”. Canadian Journal of Ophthalmology 53.4 (2018): 420-424.
- Lim WS., et al. “Comparing macula thickness between sickle cell patients of HbSS and HbSC genotype using spectral domain optical coherence tomography”. (2017):
- Ryan SJ. “Occlusion of the macular capillaries in sickle cell hemoglobin C disease”. American Journal of Ophthalmology 77.4 (1974): 459-461.
- Roy MS., et al. “Color Vision Defects in Sickle Cell Anemia”. Archives of Ophthalmology 105.12 (1987): 1676-1678.
- Marsh RJ., et al.“Macular vasculature, visual acuity, and irreversibly sickled cells in homozygous sickle cell disease”. British Journal of Ophthalmology 66.3 (1982): 155-160.
- Myint KT., et al. “Laser therapy for retinopathy in sickle cell disease”. Cochrane Database of Systematic Reviews 10 (2015):
- Ho J., et al.“A comparison of 23-gauge and 20-gauge vitrectomy for proliferative sickle cell retinopathy – clinical outcomes and surgical management”. Eye 32.9 (2018): 1449-1454.
- Cho M and Kiss S. “Detection and monitoring of sickle cell retinopathy using ultra wide-field color photography and fluorescein angiography”. Retina 31.4 (2011): 738-747.
- Newcomb N., et al. “Intravenous fluorescein photography of the ocular fundus in sickle-cell anemia”. Medical and Biological Illustration17.2 (1967): 95-98.
- Dell’Arti L., et al. “Sickle cell maculopathy: Identification of systemic risk factors, and microstructural analysis of individual retinal layers of the macula”. PLoS One 13.3 (2018): e0193582.
Citation: Ricardo Luz Leitão Guerra., et al. “Traction and Ischemic Sickle Cell Maculopathy – Case Report”. Ophthalmology and Vision Science 2.3 (2019): 285-288.
Copyright: © 2019 Ricardo Luz Leitão Guerra., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.