Case Report
Volume 2 Issue 3 - 2019
A Case of Behcet's Disease Successfully Treated with Adalimumab
1Department of Ophthalmology, AIIMS, Bhopal, India
2Department of Pediatrics, AIIMS, Bhopal, India
3Department of Uveitis and Ocular Pathology, Sankara Nethralaya, Chennai, India
2Department of Pediatrics, AIIMS, Bhopal, India
3Department of Uveitis and Ocular Pathology, Sankara Nethralaya, Chennai, India
*Corresponding Author: Priyanka, Senior Resident, Department of Ophthalmology, AIIMS, Saket Nagar, Bhopal-462020, India.
Received: January 13, 2019; Published: March 25, 2019
Abstract
We are reporting a case of Behcet’s disease successfully treated with adalimumab, refractory to high dose steroids and multiple immunosuppressives. Remission was achieved in this case with infusions of infliximab and then successfully switched to adalimumab for maintenance therapy. Very limited data on the efficacy of switching amongst antiTNF inhibitors is available for patients transitioning from infliximab to adalimumab in India. This case report shows successful switch from infliximab to adalimumab and significant improvement in retinal vasculitis and visual acuity with no relapse on adalimumab.
Keywords: Adalimumab; Behcet’s disease; Fundus fluorescein angiography; Infliximab; Optical coherence tomography; Retinitis
Introduction
Behçet’s disease (BD) is a chronic inflammatory systemic disorder, characterized by a relapsing and remitting course. The diagnosis is based on International Criteria for BD (ICBD), which includes ocular lesions, oral aphthosis and genital aphthosis each to be assigned as 2 points, whereas skin lesions, central nervous system involvement, vascular manifestations and pathergy test (if done) are to be assigned 1 point each. A patient scoring ≥ 4 points is classified as having BD [1] Ocular disease is the most frequent cause of morbidity leading to blindness in 25% of those affected.[2-3] The various non-specific immunosuppressive drugs, used either alone or combinations, frequently fail to control inflammation or maintain remissions.[2-4] The aetiology of Behcet’s disease is unknown, however it is currently thought that a central pathogenetic role of tumour necrosis factor (TNF) in the inflammatory process is possible.[4] The main goal of therapy in patients with BD is to induce and maintain remission and improve patient’s quality of life. Selecting treatment is based on the organ involved and the assessment of the severity of the disease.
Case Report
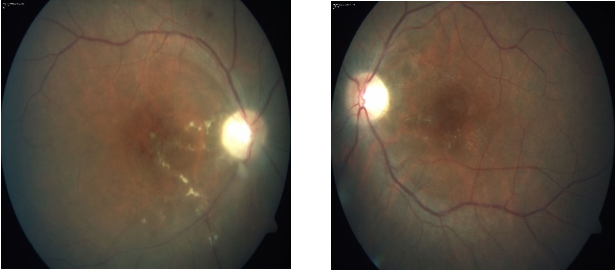
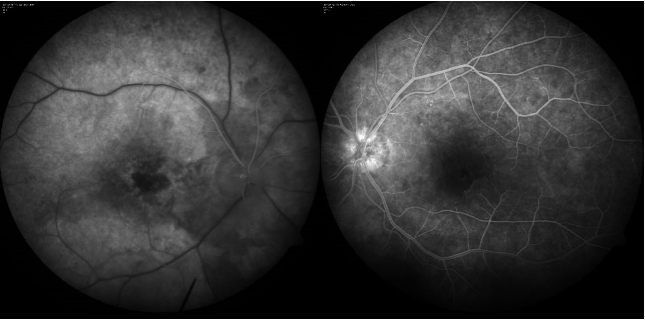
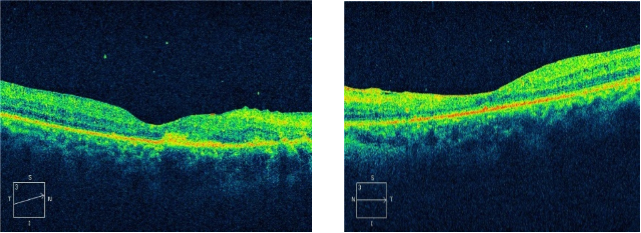
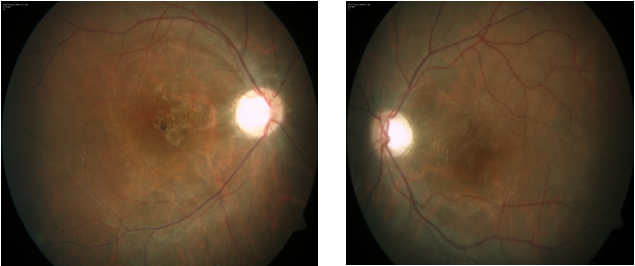
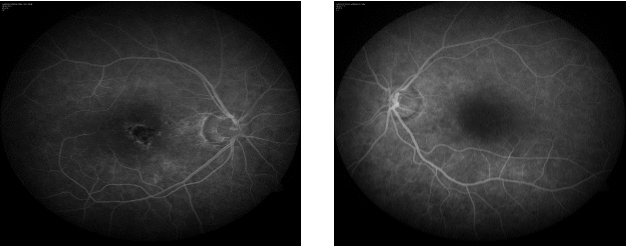
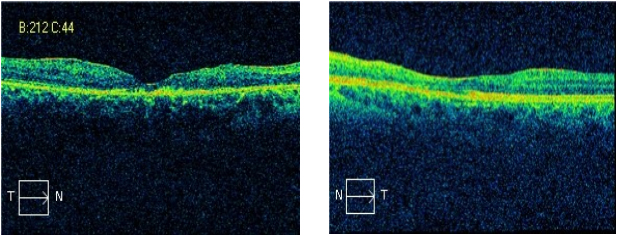
A 28 year old, Asian Indian normotensive and non-diabetic man presented with one year history of gradual diminution of vision and floaters in both eyes. The diagnosis was based on The diagnosis was based on International Criteria for BD (ICBD), which include the presence of recurrent oro-genital ulceration plus ocular lesions (ocular lesions, oral aphthosis and genital aphthosis were assigned as 2 points each). [1] HLA B51 was found to be negative in this case. His visual acuity was 10/200 in the right eye and 20/80 in the left eye. Slit lamp examination showed quiet anterior chamber with vitreous cells 2+ in right eye and 1+ in left eye. Fundus photo and FFA showed active vasculitis in both eyes (Figure 1-2).Optical coherence tomography in the right eye showed subfoveal scar just superonasal to the fovea with epiretinal membrane. The left eye had altered foveal contour with epiretinal membrane. Hard exudates and schitic spaces seen inferotemporal to the fovea. Foveal thickness was 134 microns in the right eye and 136 microns in the left eye (Figure 3). He was started on mycophenolate mofetil 1000 mg twice daily with prednisolone. At 2 month follow-up, his visual acuity was 10/200 in the right eye and 20/100 in the left eye. Slit lamp revealed quiet anterior chamber and vitreous cells 1+ in both eyes. Right eye fundus revealed no abnormality and left eye had active retinitis just above the inferotemporal arcade close to the fovea. OCT right eye showed same old findings and left eye had altered foveal contour with small traces of subretinal fluid seen inferior to the fovea along with active retinitis on FFA. This time ciclosporine 150 mg twice daily with prednisolone tried, changed to azathioprine on subsequent follow-up with low dose steroids, but showed no improvement in vision with persistent active retinitis. Treatment with infliximab infusion (5 mg/kg) every 6 weeks initiated after ruling out latent tuberculosis infection, hepatitis B and C. He became asymptomatic at 2 month follow-up with static vision (20/100 right eye: 20/40 left eye), quiet anterior chamber on slit lamp examination and no evidence of retinal vasculitis on fundus examination (Figure 4). FFA also showed no active vasculitis (Figure 5). OCT showed foveal thinning with few cystic spaces in both eyes (Figure 6). His vision remained quite stable on infliximab infusion. In view of no active retinitis infliximab infusions was discontinued after 6 month. At next follow up FFA revealed relapse with retinitis in the right eye, but remission was achieved again on reinitiating therapy with infliximab. As the disease is by nature recurrent he was switched to adalimumab 40 mg subcutaneous at every 2 weeks with patient’s consent, as it was less costly with ease of administration. Immunosuppressive was effectively tapered and stopped during second follow-up. Thereafter, the patient experienced neither ocular attacks nor adverse effect for more than 2 year. The disease has remained in complete remission with no active retinitis or vasculitis for more than 2 years during which the patient was continued to take adalimumab.
Figure 2: Fundus fluorescein angiography showing delayed arm to retina time and parafoveal small vessel staining. Foveal avascular zone looks distorted.
Figure 3: Right eye OCT revealing subfoveal scar and epiretinal membrane with foveal thickness of 134 microns. Left eye OCT revealing altered retinal contour with epiretinal membrane and foveal thickness of 136 microns.
Figure 5: Fundus fluorescein angiogram revealing macular scar in right eye and left eye showing no active vasculitis.
Figure 6: Right eye OCT showing gross foveal thinning (82 microns) with minimal retinal thickening with epiretinal membrane. Left eye revealing thinning of inner retinal layer (foveal thickness 140 microns) with thin epiretinal membrane.
Discussion and Conclusion
Several effective anti-inflammatory and immunosuppressive regimens for BD currently exist, but none results in disease cure. [2-3, 6-7] The use of ciclosporin as immunosuppressive agent in should be limited considering its potential involvement in the genesis of neurological complications of the disease (neuro-Behçet). [8] Anti-TNF agents has promising results with key safety considerations include infections, demyelinating disease, malignancies and congestive heart failure. [9] An ideal therapy should be tailored according to the extent and severity of BD. [5] In our case infliximab therapy successfully suppressed the Behcet’s eye disease within 2 month of start of infliximab and remained stable on regular infliximab infusion, but disease recurred on discontinuing infliximab. Adalimumab as considered to be equal potential safe option and more convenient as self-administered subcutaneous injection and offers more continuous drug delivery over time, thus providing an appropriate and long-term control of ocular inflammation, was added in our case of infliximab dependent Behcet’s disease. In addition, formation of autoantibodies to infliximab when restarted was also considered in our case. Adalimumab, a completely humanized IgG1 monoclonal anti-TNF-α antibody, showed promising result in our case with no recurrence. Very limited data on the efficacy of switching amongst anti-TNF inhibitors is available for patients transitioning from infliximab to adalimumab in India. It is unknown how long anti‐TNFα treatment must be given, but anti‐TNFα treatment should be continued until there is a settled response. Our patient at more than 2 year follow-up did not suffer from any side effect of adalimumab. Larger controlled studies are needed to corroborate these recent observations and confirm the efficacy and safety of adalimumab, which provide a valuable addition to therapeutic armamentarium in refractory BD.
References
- Davatchi F., et al. “The International Criteria for Behçet's Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria”. Journal of the European Academy of Dermatology and Venereology 28.3 (2014): 338-347.
- Kaklamani VG., et al. “Behçet's Disease”. Semin Arthritis Rheum 27.4 (1998): 197-217.
- Yazici H. “Behçet's syndrome: where do we stand?” The American Journal of Medicine 112.1 (2002): 75-76. Sfikakis PP. “Behcet's disease: a new target for anti-tumour necrosis factor treatment”. Annals of the Rheumatic Diseases (2002): 61.
- G Hatemi., et al. “Management of Behcet disease: A systematic literature review for Against Rheumatism evidence-based recommendations for the management of Behcet disease”. Annals of the Rheumatic Diseases 68.10 (2009): 1528-1534.
- Sakane T., et al. “Behcet's disease”. The New England Journal of Medicine 341.17 (1999): 1284-1291.
- Kaklamani VG and Kaklamanis PG. “Treatment of Behçet's disease-an update”. Semin Arthritis Rheum 30.5 (2001): 299-312.
- Bouomrani S., et al. “Ciclosporin-associated cerebral tumor-like location of Behçet's disease”. Revue Neurologique 166.10 (2010): 849-854.
- Furst D E., et al. “Updated consensus statement on biological agents for the treatment of rheumatic diseases”. Annals of the Rheumatic Diseases(2013): 200465.
Citation: Priyanka., et al. “A Case of Behcet's Disease Successfully Treated with Adalimumab”. Ophthalmology and Vision Science 2.3 (2019): 294-298.
Copyright: © 2019 Priyanka., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.