Research Article
Volume 1 Issue 1 - 2017
Hemodynamic Management of High Blood Pressure
1Critical care resident at Caracas University Hospital, European Society of Cardiology Council on Hypertension
2Pediatrics resident at Caracas University Hospital
3Nephrologist, Intensivist at Caracas University Hospital
2Pediatrics resident at Caracas University Hospital
3Nephrologist, Intensivist at Caracas University Hospital
*Corresponding Author: Chacón-Lozsán F, Critical care resident at Caracas University Hospital, European Society of Cardiology Council on Hypertension, Venezuela.
Received: July 02, 2017; Published: August 21, 2017
Abstract
Background: Hypertension is an important risk factor for cardiovascular events, stroke and kidney disease, optimal hypertension control still a controversial subject in medical literature, several studies proposed the hypertension control calculating hemodynamic parameters.
Materials and Methods: In the present study we recruited 84 patients’ males (34%) and females (49%) between 32 and 95 years of age with non-controlled hypertension taken 2 or more medications and measured heart rate (HR), systolic (SBP), diastolic (DBP) and mean (MAP) blood pressure, pulse pressure (PP), cardiac index (CI) using Liljestrand & Zander modified formula to calculate stroke volume (CI = [HR*(PP/MAP)]/Body surface area), central venous pressure (CVP) using inferior vena cava diameter (IVCD), systemic vascular resistance index (SVRi = MAP/CI*80) and divided in six hemodynamic groups Hyperdynamics (Hd) were those with CI > 3,5L/min/m2, High Resistance (Hr) group when SVRi > 2500 dynas, Fluid overload (FO) when CVP > 8 cm H2O or IVCD > 2 cm and mixed types, Hd + Hr, Hd + FO and Hr + FO, a basal values was measured after 1 week washout with captopril, after washout treatment was selected according hemodynamic groups with a 6 months follow up.
Results: We found a statistical significant reduction of all parameters at the first month after treatment and hypertension control according European of Society Cardiology guidelines in 100% of patients at 3th month of treatment with hemodynamic normalization, only Hd + FO at 6th month, with no symptomatic hypotension.
Conclusion: Hemodynamic guided treatment to control high blood pressure had good results in this study; however, bigger trials are needed to prove his efficacy.
Keywords: Hypertension; Hemodynamics; High blood pressure; Cardiac index; Vascular resistance
Introduction
Hypertension is related to high risk factor for cardiovascular, cerebrovascular and kidney diseases. The European Heart Association defines hypertension when systolic blood pressure (SBP) is > 140 mmHg, and or diastolic blood pressure (DBP) is > 90 mmHg and according the epidemiological studies hypertension control reduces mortality [1].
Blood pressure is the product of cardiac output and total peripheral vascular resistance, and cardiac output depends on stroke volume, heart rate and preload, this means that any change in one of these parameters will change blood pressure [2].
In 1996 Sramek., et al. [3] proposed the hypertension treatment using hemodynamic parameters compared with conventional therapy in 322 patients with non-controlled hypertension using 2 or more hypertensive drugs and they obtained a 75% of controlled patients at the 3RD week follow up. After their study a total of 1087 patients in 7 studies were enrolled to compare the hemodynamic protocol Vs conventional control of hypertension observing a rate mean success of 72,6% [4].
According to this protocol, patients were divided in a hyperdynamic group when cardiac index was high, a high systemic vascular resistance group and the group of patients with fluid overload and used a specific pharmacologic group to each hemodynamic pattern. Those patients with hyperdynamic pattern were treated with B-blockers or non-dihydroopyridine calcium channel blocker, patients with high systemic vascular resistance pattern are treated using angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, dihydropyridine calcium channel blocker or direct vasodilator and patients with fluid overload pattern were treated with thiazidique diuretics [5].
In the present article we studied the effect of the hemodynamic directed therapy in patients with non-controlled hypertension.
Materials and methods
Male and female patients between 18 and 95 years of ager were recruited with diagnosed hypertension currently receiving 2 or more antihypertensive medications with a systolic blood pressure > 140 mmHg, diastolic blood pressure > 90 mmHg, excluded all with ejection fraction < 40%, had abnormal laboratory findings, atrial fibrillation, severe valvular disease, severe renal disease, cirrhosis, pregnancy or neoplasic diseases. All patients provided a written informed consent and had study procedures consistent with Declaration of Helsinski and Venezuelan deontology code.
Hemodynamic evaluation: we measured heart rate by electrocardiography, systolic (SBP), diastolic (DBP) and mean (MBP) blood pressure using oscillometric multi parameter monitor according American Heart Association Guidelines [6],
Pulse pressure (PP) was calculated PP = SBP-DBP,
Stroke volume (SV) was calculated using modified Liljestrand & Zander formula [7] SV = PP/MAP, Cardiac index (CI) CI = SV* HR/Body surface area, central venous pressure was estimated using Inferior Vena Cava diameter (IVCD) according Nagdev A., et al. correlations [8],
Systemic Vascular Resistance index (SVRi) SVRi = MAP-CVP/CI *80.
Stroke volume (SV) was calculated using modified Liljestrand & Zander formula [7] SV = PP/MAP, Cardiac index (CI) CI = SV* HR/Body surface area, central venous pressure was estimated using Inferior Vena Cava diameter (IVCD) according Nagdev A., et al. correlations [8],
Systemic Vascular Resistance index (SVRi) SVRi = MAP-CVP/CI *80.
Procedure: After study explanation and informed consent obtained a basal hemodynamic parameters were measured and classified in 6 hemodynamic groups.
- Hyperdynamic group: patients with diagnosed hypertension only with cardiac index > 3,5 L/min/m2.
- High resistance group: patients with diagnosed hypertension with only SVRi > 2500 dynes/sec/m2/cm-5.
- Fluid overload group: patients with hypertension only with CVP > 8 cm H2O or IVCD >2 cm.
- Hyperdynamic with High resistance group: patients with diagnosed hypertension with cardiac index > 3,5L/min/m2, and SVRi > 2500 dynes.
- Hyperdynamic with fluid overload group: patients with diagnosed hypertension with cardiac index > 3,5L/min/m2, and CVP > 8 cm H2O or IVCD > 2 cm.
- High resistance with fluid overload: patients with diagnosed hypertension with SVRi > 2500 dynes and CVP > 8 cm H2O or IVCD > 2 cm.
- All patients had a drugs washout with captopril for 1 week before start guided treatment adjusted to each group with control at 1st month, 3rd month and 6th month.
- Hyperdynamic group: beta blocker or non-dihydroopyridine calcium channel blocker.
- High resistance group: angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, dihydropyridine calcium channel blocker or direct vasodilator.
- Fluid overload group: diuretic.
- Hyperdynamic with High resistance group: beta blocker or non-dihydroopyridine calcium channel blocker + angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, dihydropyridine calcium channel blocker or direct vasodilator.
- Fluid overload group: diuretic.
- Hyperdynamic with fluid overload group: beta blocker or non-dihydroopyridine calcium channel blocker + diuretic.
- High resistance with fluid overload: angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, dihydropyridine calcium channel blocker or direct vasodilator + diuretic.
All results were analyzed in GraphPad PRISM 6.0 for windows using ANOVA Non-parametric statistical analysis with a confidence interval of 90% taking as significant a P < 0,001, results were presented in tables and graphics.
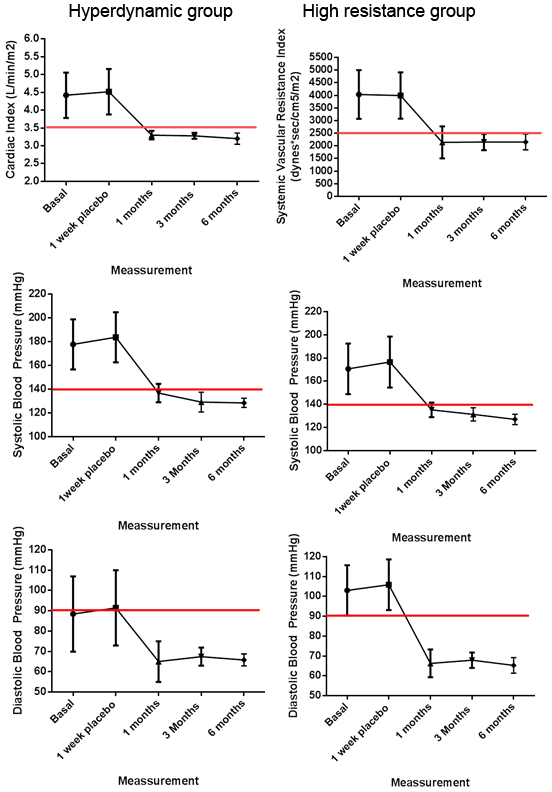
A total of 84 patients were recruited, detailed data on table 1, 34 males and 49 females with age of 62,3 ± 14,7 years old all patients with SBP > 140 mmHg, DBP > 90 mmHg, after washout patients were divided in groups. In the Hyperdynamic group with a total of 5 patients with CI > 3,5 and rest of parameters in normal range, everyone was treated using only Bisoprolol and blood pressure control goals according ESC guidelines were obtained at the 3rd month and hemodynamic goal (CI < 3,5) at first month, no clinical hypotension was reported [Figure 1].
The High resistance group enrolling 22 patients with SVRi > 2500, and rest of parameters in normal range, every patient was treated using only Amlodipine and we obtained blood pressure control goals according ESC guidelines at the 3rd month of treatment and hemodynamic goal (SVRi < 2500) also at 3rd month with no clinical hypotension reported [Figure 1].
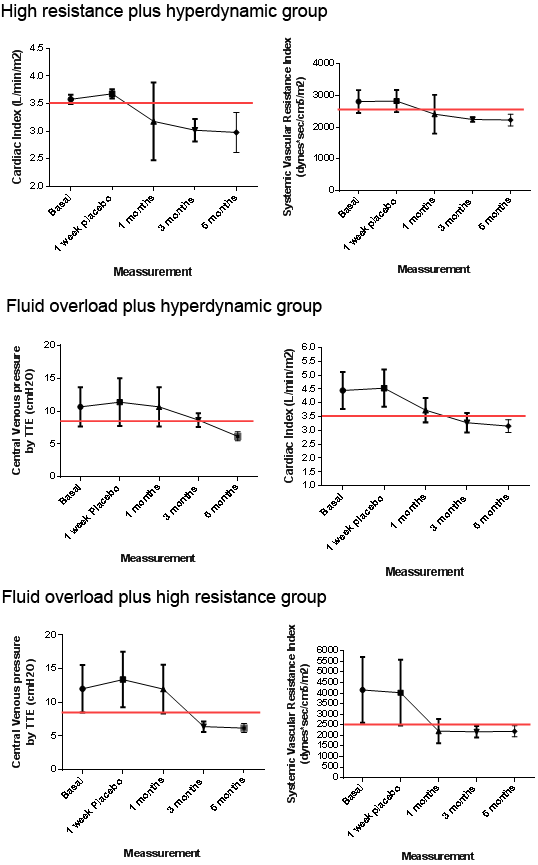
In the Hyperdynamic with High resistance group a total of 5 patients were recruited with CI > 3,5 and SVRi > 2500, with the rest of the parameters in normal range, all patients were treated using only Bisoprolol plus Amlodipine and blood pressure control goals according ESC guidelines and hemodynamic goals (CI < 3,5 and SVRi < 2500) were obtained at the 3rd month of treatment with no clinical hypotension reported [Figure 2].
Hyperdynamic with fluid overload group was represented in 15 patients with CI > 3,5 and CVP > 8 with the rest of the parameters in normal range, everyone was treated using only Bisoprolol plus hydrochlorothiazide observing blood pressure control goals according ESC guidelines at the 3rd month after treatment and hemodynamic goal (CI < 3,5 and CVP < 8) at 6th month with no clinical hypotension reported [Figure 2].
Patients with High resistance with fluid overload were 37 with SVRi > 2500 and CVP > 8, and rest of hemodynamic parameters in normal range, everyone was treated using only Amlodipine plus hydrochlorothiazide archiving blood pressure control goals according ESC guidelines and hemodynamic goals (CVP < 8 and SVRi < 2500) at the 3rd month of treatment, no clinical hypotension was reported [Figure 2]. No patients were recruited with fluid overload pattern alone.
| Variable | All | Hd | Hr | Hd + Hr | Hd + FO | Hr + FO |
| n | 84 | 5 | 22 | 5 | 15 | 37 |
| Age years (mean ± SD) |
62,3 ± 14,7 | 51,2 ± 10,9 | 63,2 ± 14,1 | 58,4 ± 15,2 | 64,4 ± 16,5 | 63 ± 13,9 |
| Male (n/%) |
34/41 | 0/0 | 5/22,8 | 2/40 | 7/47 | 18/49 |
| Female (n/%) |
49/59 | 5/100 | 17/77,2 | 3/60 | 8/53 | 19/51 |
| BMI (mean ± SD) |
25,4 ± 4,8 | 24,1 ± 3,6 | 25,5 ± 4,1 | 25,8 ± 4,6 | 23,1 ± 2,9 | 26,9 ± 5,3 |
| BSA (mean ± SD) |
1,7 ± 0,2 | 1,5 ± 0,08 | 1,7 ± 0,2 | 1,6 ± 0,08 | 1,5 ± 0,1 | 1,7 ± 0,2 |
| Basal HR (mean ± SD) |
83,2 ± 16,4 | 94,4 ± 24,3 | 81,2 ± 12,4 | 93,8 ± 12,2 | 92,8 ± 18 | 78,5 ± 14,7 |
| Final HR (mean ± SD) |
73 ± 6,8 | 73,6 ± 5,5 | 73,8 ± 6,2 | 75,6 ± 4,8 | 73,9 ± 7,9 | 71,4 ± 7 |
| Basal SBP (mean ± SD) |
178,6 ± 23,5 | 177,6 ± 21,1 | 170,6 ± 21,8 | 186,8 ± 23 | 178,9 ± 14,5 | 183,6 ± 27 |
| Final SBP (mean ± SD) |
127,5 ± 4,8 | 128,4 ± 3,8 | 127 ± 4,4 | 125,2 ± 5,3 | 126,9 ± 5,1 | 128,4 ± 5 |
| Basal DBP (mean ± SD) |
99,9 ± 16,4 | 88,4 ± 18,5 | 103 ± 12,6 | 102,6 ± 14,2 | 67,7 ± 8,6 | 106,2 ± 16 |
| Final DBP (mean ± SD) |
66,4 ± 4,6 | 65,8 ± 2,9 | 65,2 ± 3,9 | 68 ± 2,1 | 67,6 ± 5,1 | 65,2 ± 5,3 |
| Basal MAP (mean ± SD) |
126,2 ± 16,7 | 118,2 ± 18,1 | 125,5 ± 14,4 | 130,6 ± 17,1 | 118,1 ± 7,9 | 131 ± 17,3 |
| Final MAP (mean ± SD) |
86,7 ± 3,9 | 86,8 ± 2,3 | 85,9 ± 3,3 | 87,2 ± 2,3 | 87,4 ± 4,5 | 86,2 ± 4,6 |
| Basal CI (mean ± SD) |
3,09 ± 1,07 | 4,4 ± 0,6 | 2,5 ± 0,5 | 3,5 ± 0,08 | 4,4 ± 0,6 | 2,5 ± 0,2 |
| Final CI (mean ± SD) |
3,02 ± 0,41 | 3,2 ± 0,15 | 3 ± 0,4 | 2,9 ± 0,3 | 3,1 ± 0,2 | 2,9 ± 0,3 |
| Basal SVRi (mean ± SD) |
3543 ± 1553 | 2079 ± 297,7 | 4029 ± 962,4 | 2814 ± 361,6 | 2020 ± 305,9 | 4160 ± 1558 |
| Final SVRi (mean ± SD) |
2191 ± 325,6 | 1969 ± 240,3 | 2153 ± 313,9 | 2231 ± 185,1 | 2080 ± 209,5 | 2200 ± 260,1 |
| Basal CVP (mean ± SD) |
9,3 ± 4,0 | 5,6 ± 1,3 | 5,7 ± 1 | 6,2 ± 0,8 | 10,6 ± 2,9 | 12 ± 3,5 |
| Final CVP (mean ± SD) |
7,2 ± 1,2 | 6 ± 1 | 6,1 ± 0,9 | 6,4 ± 0,8 | 6,2 ± 0,6 | 6,2 ± 0,6 |
Legend: Hyperdynamic: Hd, High Resistance: Hr, Standard Deviation: SD, Body mass index: BMI, Body surface area: BSA, Heart rate: HR (beats per minute), Systolic blood pressure: SBP (mmHg), Diastolic blood pressure: DBP (mmHg), Mean Arterial pressure: MAP (mmHg), Cardiac index: CI (L/min/m2), Systemic vascular resistance index: SVRi (dynes/sec/m2/cm-5), Central venous pressure: CVP (cmH2O).
Table 1: Patient’s data.
Table 1: Patient’s data.
Discussion
According to Tarazi [9], hypertension can be explained by different hemodynamic alterations in cardiac output, intravascular volume or increase in vascular resistance, according to his analysis, Sramet., et al. [3] investigate for first time in 1996 an hemodynamic approach of hypertension selecting drugs according the hemodynamic parameter obtained measuring cardiac index, systemic vascular resistance and a preload parameter, they found a 75% of blood pressure control in 3 weeks follow up in 322 patients.
Until now seven trials were found testing hemodynamic assessment of hypertension with a total of 1087 patients treated summarizing all studies with an observed 72,6% effectivity compared with standard method [4], in this order of ideas we observed similar results with 100% of blood pressure control according to European Guidelines at the 3rd month of treatment and 100% of control in hemodynamic goal with no reported side effects, we observed that hardest pattern to archive hemodynamic control was the hyperdynamic with fluid overload pattern needing 6 months to obtain hemodynamic control.
The newest clinical trial was developed by Krazesinsky., et al. in 2016 [5], enrolling 272 patients observing 87,7% of blood pressure control, compared with 69,1% off the standard blood pressure therapy. In the same way of those researches, we found that hemodynamic approach is a safe and efficient method to archive blood pressure and hemodynamic goals in short time with low side effects, so according to these results, the hemodynamic hypothesis in the assessment of high blood pressure control can me more pathophysiological accurate to guide antihypertensive therapy.
However, our small sample and poor resources to measure target organ damage may be a limitation to observe more effects of this method in patients with high blood pressure. More researches are needed with large samples and methods to measure organ damage and survival of these patients.
References
- Mancia G., et al. “2013 ESH/ESC Guidelines for the management of arterial hypertension”. Journal of Hypertension 31.7 (2013): 1281-1357.
- Egan B., et al. “The importance of hemodynamic considerations in essential hypertension”. American Heart Journal 116.2 (1988): 594-599.
- Sramek B., et al.“Normohemodynamic goal-oriented antihypertensive therapy improves the outcome”. The American Society of Hypertension 9 (1996): 141.
- Chacón-Lozsán F. “Non-invasive hemodynamic analyses to guide pharmacotherapy of high blood pressure: mini-review”. Journal of Cardiology & Cardiovascular Therapy 3.3 (2017): 1-3.
- Krzesinski P., et al. “Who benefits more from hemodynamically guided hypotensive therapy? The experience from two randomized, prospective and controlled trials”. Therapeutic Advances in Cardiovascular Disease 10.1 (2015): 21-29.
- Pickering T., et al. “Recommendations for blood pressure measurement in humans and experimental animals: a statement for professionals from subcommittee of professional and public education of the American heart association council of high blood pressure research”. Circulation 111.5 (2005): 142-161.
- Sun J., et al. “Estimating cardiac output from arterial blood pressure using blood pressure waveforms: a critical evaluation using MIMI II Database”. Computers in cardiology (2005): 295-298.
- Nagdev A., et al. “Emergency department bedside ultrasonographic mesasurement of caval index for noninvasive determination of low central venous pressure”. Annals of Emergency Medicine 55.3 (2010): 290-295.
- Tarazi R. “The hemodynamics of hypertension. Hypertension: physiopathology and treatment. 2nd ed. New York”. McGraw-Hill Book Company (1983): 14-42.
Citation:
Chacón-Lozsán F., et al. “Hemodynamic Management of High Blood Pressure”. Therapeutic Advances in Cardiology 1.1 (2017):
69-75.
Copyright: © 2017 Chacón-Lozsán F., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.