Research Article
Volume 1 Issue 2 - 2017
Changes in the Open Heart Surgery Protocol and Outcomes in a Nigerian National Cardiothoracic Center of Excellence over 42 Years
1Senior Lecturers and Honorary Consultant Cardiothoracic Surgeons, University of Nigeria, Enugu Campus
2Senior Lecturer and Honorary Consultant Paediatric Cardiologist, University of Nigeria, Enugu Campus
3Senior Lecturer and Honorary Consultant Cardiac Anaesthetist, University of Nigeria, Enugu Campus
4Deputy Director Pharmacist, i/c Intensive Care Unit, University of Nigeria, Ituku/Ozalla, Enugu
2Senior Lecturer and Honorary Consultant Paediatric Cardiologist, University of Nigeria, Enugu Campus
3Senior Lecturer and Honorary Consultant Cardiac Anaesthetist, University of Nigeria, Enugu Campus
4Deputy Director Pharmacist, i/c Intensive Care Unit, University of Nigeria, Ituku/Ozalla, Enugu
*Corresponding Author: Nwafor IA, Senior Lecturers and Honorary Consultant Cardiothoracic Surgeons, University of Nigeria, Enugu Campus, Nigeria.
Received: July 06, 2017; Published: September 18, 2017
Abstract
Background: Open heart surgery is one of the complex procedures physicians undertake in modern medicine. It requires high tech equipment, special infrastructure and highly skilled manpower, especially in the areas of cardiology, cardiac surgery, anaesthesiology and cardiac perfusion. Preoperative diagnosis must be accurate and patients’ safety determined in order that appropriate informed consent is given.
The objective of this study is to highlight our institutional changes in protocol including outcome and compare same with what is available in the literature.
Materials and Method: Our cardiothoracic center carried out infrequent Open Heart Surgery Programme for 42 years (1974-2016). During this period preoperative assessment especially investigations were done to confirm diagnosis, determine patients’ fitness and assess patients’ co-morbidities. In addition to helping the surgeons appropriately plan and execute the surgery, they helped in predicting postoperative support and maximize the chances of uneventful surgery. A retrospective study, using the hospital data base was performed to ascertain the outcomes of varied new investigative protocol over time.
Results: Of the total of 251 open heart operations carried out, there is a tremendous drop in the hospital mortality rate when the period of 1974-2000 was compared with that of 2013-2016.
Conclusion: The introduction of technologically driven investigative parameters in preoperative assessment of patients had a great bearing in the intra-operative and postoperative outcome of patients.
Keywords: Complex; Congenital; Diagnostic; Preoperative; Investigation
Introduction
Our open heart surgery program started in the year 1974, firstly as a cardiac mission model and later on as a complete local affair [1-4]. The intervention of military in governance of this country disrupted the program leading to collapse of infrastructure, brain drain and inter-professional conflict [5]. With the enthronement of democratic rule in 1999 [6], Nigerians in diaspora galvanized themselves and resuscitated the center initially through a cardiac mission model and now by combination of both local team and cardiac mission [7].
During the 42 years but interrupted period of open heart surgery in our center in a developing country, ravaged by military rule, unprecedented corruption, civil strife and nepotism [8] a total of 251 cases of open heart surgeries have been performed. From the beginning, the preoperative assessment hinged mainly on clinical history and physical examination with limited diagnostic investigations [9]. This was because, the available technology like B-mode and Doppler echocardiography, cardiac catheterization, CT scan and MRI were then not available. The maximum diagnostic investigations in the armamentarium of our center at that time, used to confirm clinical diagnosis were A-mode echocardiography, chest x-ray and electrocardiogram. This therefore affected accurate preoperative diagnosis. Mortality and morbidity were relatively high. Sometimes, different diagnoses were met intra-operatively, forcing the surgeon to abandon the procedure if could not be done. Others were made at autopsy. However, the fitness of the patients’ investigations for the operation was to a reasonable degree carried out. Such tests were Complete Blood Count (CBC), Kidney function test/serum electrolyte urea and creatinine(SEUC), Antistreptococcal Antigen(ASO) titre, coagulation profile(Partial Thromboplastin Time, PTT; Prothrombin Time, PT and International Normalized Ratio, INR), urinalysis, liver function test and Hepatitis-B surface Antigen(HBs-Ag) as well as Hepatitis-C Antigen(HC-Ag test). Others include the genotype of the patients and Fasting Blood Sugar (FBS). These scenarios were used in the late 1970s and throughout 1980s.
In the early 1990s, there was the availability of B mode and Doppler echocardiography in the center, made personally available by one Dr Okereke Okezika, who then returned from Texas Heart Institute, Houston, USA, to join the local team [1]. Indeed, the combination of echocardiography, electrocardiogram and chest x-ray improved the accuracy of the preoperative diagnostic investigations, which in turn impacted positively on the outcome.
With the combined effort of the Federal Government of Nigeria, Tertiary Education Trust Fund(TETFUND), from University of Nigeria/Federal Ministry of Education and Nigerians in diaspora, the center now has both 2D- and 3D-echocardiography, Cardiac catherisation instruments, static and mobile chest x-ray machines, ABG analyzer, 4 i-stat machines among other state-of-the-art equipment to make accurate preoperative diagnosis [5]. While efforts were being made in providing the desired equipment, training and retraining of staff are also ongoing. With the equipment and local staff available at our center, preoperative investigative protocol was formulated and this guarded the successful management of both adult cardiac and pediatric cardiac diseases, including complex ones [7].
Materials and Method
National Cardiothoracic Center of Excellence, UNTH, Enugu, Nigeria, was born in 1984, following the unification and designation of the combined units of cardiology (adult and paediatric) and cardiothoracic surgery as the National Cardiothoracic Center of Excellence. The center performed about 251 cases of open heart surgeries between 1974 and 2016 (42 years). A retrospective study of the preoperative investigations done for these patients and the outcome of these tests on patients’ morbidity and mortality was done. The hospital database was reviewed. These investigations were divided into diagnostic and patients’ fitness assessment. The diagnostic types were subdivided into radiologic and non-radiologic. Also, the fitness assessment investigations were also divided into co-morbidities assessment and complications emanating from cardiac diseases. Inclusion criteria were those that had open heart surgery within the specified period and those investigations done before the operation. Exclusion criteria were those that had extra-cardiac operations and the postoperative investigations. The protocol was modified over time as equipment and expertise became available.
Data were analyzed using SPSS version 16 (Chicago). Rates and proportions were calculated using arithmetic percentage.
Results
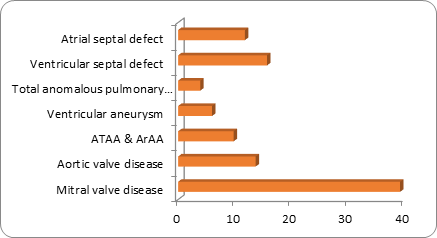
The cardiac operations included congenital heart defects and acquired heart diseases. The types of diagnostic investigations are listed according to the number of patients that benefited and the period of the surgery.
| S. No | Indications for surgery | Percentage (%) | Number |
| 1 | Mitral valve disease | 39.2 | 40 |
| 2 | Aortic valve disease | 13.7 | 14 |
| 3 | ATAA & ArAA | 9.8 | 10 |
| 4 | Ventricular aneurysm | 5.99 | 6 |
| 5 | Total anomalous pulmonary V/drainage | 3.9 | 4 |
| 6 | Ventricular septal defect | 15.7 | 16 |
| 7 | Atrial septal defect | 11.8 | 12 |
| Total | 100 | 102 |
Table 1: Table showing the cases done during the period of 1974-2000.
| S. No | Age range (years) | Female | Male | Total | Percentage (%) |
| 1 | 0-10 | 20 | 25 | 45 | 37.82 |
| 2 | 11-20 | 5 | 9 | 14 | 11.77 |
| 3 | 21-30 | 4 | 1 | 7 | 5.88 |
| 4 | 31-40 | 8 | 7 | 15 | 12.61 |
| 5 | 41-50 | 7 | 10 | 17 | 14.29 |
| 6 | 51-60 | 4 | 7 | 11 | 9.24 |
| 7 | 61-70 | 2 | 3 | 5 | 4.20 |
Table 2: Age range of patients.
In 2003, ICF/KHF did 11 cases of Open Heart surgeries, comprising 6 paediatric and 5 adults
In 2003, ICF/KHF did 11 cases of Open Heart surgeries, comprising 6 paediatric and 5 adults
| S. No | Types of Cases managed | Number | Percentage (%) |
| 1 | Aortic valve disease | 19 | 13.77 |
| 2 | Mitral valve disease | 43 | 31.16 |
| 3 | Tricuspid valve disease | 12 | 8.70 |
| 4 | Tetraology of Fallot | 9 | 6.52 |
| 5 | Ventricular septal defect | 17 | 12.32 |
| 6 | Atrial septal defect | 10 | 7.25 |
| 7 | Atrial myxoma | 3 | 2.17 |
| 8 | Ruptured aneurysm of Vasalva | 2 | 1.45 |
| 9 | Double outlet ventricle | 4 | 2.90 |
| 10 | Subaortic membrane | 4 | 2.90 |
| 11 | Coronary artery disease | 3 | 2.17 |
| 12 | Cotriatrium | 2 | 1.45 |
| 13 | Truncus arteriosus, type 1 | 2 | 1.45 |
| 14 | Mitral atresia | 1 | 0.73 |
| 15 | Atrioventricular defect/endocardial cushion | 3 | 2.17 |
| 16 | Pulmonary atresia with MAPCAS | 1 | 0.73 |
| 17 | Congenital absence of anterior and posterior leaflets of tricuspid valve | 1 | 0.73 |
| Total | 138 | 100 |
Table 3: Number of cases managed during the period of 2013-2016.
| Period | No of patients | Mortality | Mortality rate (%) |
| 1974-2000 | 102 | 50 | 49 |
| 2003 | 9 | 6 | 66 |
| 2013-2017 | 140 | 15 | 11 |
| 251 | 71 | 28.3 |
Table 4: Showing mortality rate of patients in relation to period of Open Heart Surgery.
The preoperative investigations done at the formative years are listed against the outcome of the operations performed then. The provision of the state-of-the-art equipment revolutionized preoperative assessment of patients and imparted positively on the morbidity and mortality of patients.
| S.no | Diagnostic tests | Functional capacity tests | Fitness of patients’ tests |
| 1 | Chest x-ray | Lung function test | APTT, PT, INR |
| 2 | Electrocardiogram | Liver function test Serum electrolyte, urea and creatinine |
Full Blood Count(Hb, WBC, Platelets) |
| 3 | Echocardiography | Fasting Blood Sugar | Urinalysis |
| 4 | Coronary angiography | Retroviral Screening | Serum protein(total and differential) |
| 5 | Cardiac catheterization | HBsAg, Hcv Ab | |
| 6 | C-reactive protein | ||
| 7 | Antistreptococcal(ASO) titre | ||
| 8 | Erythrocyte Sedimentation Rate(ESR) |
Table 5: Showing the Institutional Protocol for preoperative investigations of Open Heart Surgery patients.
| Radiologic | Non radiologic |
| Chest x-ray | Electrocariogram (ECG) |
| Echocardiography | Antistreptococcal titre (ASO) |
| Coronary angiography | Erythrocyte Sedimentaion Rate(ESR) |
| Cardiac Catheterization | C-reactive protein |
| CT angiography | Blood culture for infective endocarditis |
Table 6: Diagnostic investigations.
Discussion
Open heart surgical patients are one of the most extremely investigated groups of patients that cardiothoracic surgeons and cardiac anesthesiologists encounter [9-10]. In our protocol, preoperative investigations are usually considered in 3 categories, namely: 1. Diagnostic investigations – these are done to confirm the clinical diagnosis as dictated by the pathology and medical history, 2. Investigations done to rule out or determine the extent of co-morbidities and 3., the investigations to assess patients’ fitness for the intended surgery.
At varying period in our center, open heart procedures were done, see table 4. A total of 251 cases have so far been done, with 28.3% mortality. However, the mortality rate for the period of 1974-2000 was 49% and for 2003, the mortality rate was 66% while the mortality rate for the period of 2013 to 2017, was 11%. From the diagnostic armamentarium, the progressive reduction in the rate of mortality is thought to be the acquisition of the state-of-the art equipment over time to make accurate diagnosis and rule out co-morbidities before surgery.
Through the efforts of Nigerians in diaspora, the Tertiary Educational Trust Fund (TETFUND), and Non-governmental Organizations, our institution acquired the- state-of-the art equipment, which enabled the safe cardiac operations within the period of March, 2013 to February, 2017. The adoption of cardiac mission model by our institution coupled with oversea training of some our staff [11-12], led to the successful creation of a preoperative investigative protocol for patients undergoing open heart surgeries in our institution, table 5. The protocol divides the investigations into 3 parts: 1. Diagnostic tests, 2. Functional capacity tests and patients’ fitness tests. The diagnostic tests are subdivided into radiologic and non-radiologic, table 6.
One of the foremost radiologic-diagnostic investigations is chest radiograph. This test can reveal boot-shaped heart of Tetraology of Fallot (prominent pulmonary bay and up-turnement of left ventricle apex) and egg on stick appearance of Transposition of Great Arteries [13]. In addition, chest x-rays provides information on enlarged cardiac silhouette/cardiomegaly, congestive cardiac failure with pulmonary oedema, pleural or pericardial effusions [14]. Other radiologic tests like Echocardiography, whether Transthoracic/Transesophageal, provides information of cardiac anatomy, ventricular and valvular functions as well as global and septal wall motions including presence or absence of intra-atrial clots in patients with chronic atrial fibrillation [15].
In both congenital and acquired heart diseases, left heart catheterization may indicate coronary angiography, aortography, left ventriculography and manometry. This provides information about sites and severity of coronary artery disease, mitral and aortic valve functions, left ventricle morphology and function. Likewise, right heart catheterization permits measurement of pulmonary artery pressure and cardiac output, calculation of transpulmonary gradient and vascular resistance. In cases of shunts between systemic and pulmonary systems, serial blood sampling allows computation of shunt fraction [16-18]. With this, congenital cardiac defects like Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD) and Atrioventricular Canal defect (AVCD are diagnosed. Computerized (Ct) scan and magnetic resonance (MR) angiography are employed in our protocol aids in making accurate diagnosis of ascending aortic aneurysm including aortic dissection.
In sub-Saharan African countries like Nigeria, rheumatic heart diseases and infective endocarditis are the commonest indications of intra-cardiac operations in adults [19]. To this extent, estimation of Antistreptococcal O antigen (ASO titre), Erythrocyte Sedimentation Rate(ESR) and C-Reactive Protein(CRP) is employed in our protocol while evaluating patients with valvular heart diseases and infective endocarditis preparatory for open heart surgery. Positive titres indicate active disease at that point in time and subsequently patient is denied surgery until appropriate treatment is done.
Complete blood count (CBC), is used in estimating presence or absence of anaemia including the quantitative platelet and white blood cell abnormality [20-21]. Baseline coagulation panel (prothrombine time(PT); International Normalized Ratio(INR) and Activated Partial thromboplatin Time (APTT) is estimated and recorded because of the use of anticoagulants both intra-and postoperatively. Any abnormality detected is treated before surgery. Furthermore, patients on anticoagulants like warfarin will have their medications stopped about a week before surgery and switched over to fractionated heparin [22-23]. The same applies to those on aspirin.
Chronic diuretic therapy decreases serum sodium, potassium and urea. Hypokalaemia is a common finding in cardiac patients and hypokalaemia is infrequently associated with hypomagnesemia [24]. In view of this, preoperative estimation of serum electrolytes including urea and creatinine in our protocol is justified.
Other appropriate preoperative investigations that may lead to successful intra-operative and postoperative outcome as may be detected by co-morbid diseases include respiratory function test, arterial blood gas (ABG) estimation, carotid artery ultrasound and angiography. These tests among the others enumerated above constitute our institutional preoperative protocol for patients undergoing open heart surgery.
On the basis of the above investigations, an accurate diagnosis is made and patient’s operative risk assessment is determined using the established criteria, New York Heart association[19], Canadian Cardiovascular score [20] and Duke [21].
The adoption of the protocol has worked out well because judging from the outcome of 2013-2016 data, table 3, mortality rate appears to be on the decline.
Conclusion
Preoperative assessment in cardiac surgery is a veritable way of aiding clinical evaluation in making accurate diagnosis, determining preoperative risks which usually have great bearing in the operative and postoperative events. The adoption of ASO titre, ESR and CRP as well as blood culture with regard to rheumatic heart disease and infective endocarditis has imparted positively on the outcome of our procedures.
References
- Adebonojo SA. “Development of Open Heart Surgery in West Africa. Historical Perspective; Guest Lecture, 48th Annual Scientific Conference, West African College of Surgeons, Freetown, Sierra Leone, February, 2008”. Sharp-Prints Publishing Press (2012):
- Gene Bukham. “Cardiovascular Disease in the Developing World; Global Health Education Consortium”. The New England Journal of Medicine 3 (2006): 1-59.
- Edwin F., et al. “The Development of Cardiac Surgery in West Africa- the Case of Ghana”. The Pan African Medical Journal9 (2011): 15.
- Eze JC and Ezemba N. “Open Heart Surgery in Nigeria: Indications and Challenges”. Texas Heart Institute Journal 34.1 (2007): 8-10.
- Orjiako AB. “Interprofessional conflict resolution in the health sector”. Nigerian Medical Journal 5 (1996): 28-31.
- Ebgefo OD. “Fifteen Years of Democracy, 1999-2014: Reflections on Nigerian’s Quest for National Integration”. African Research Review 9.2 (2015): 37.
- Nwafor IA., et al. “Management of complex CHD at the National Cardiothoracic Center of Excellence, University of Nigeria Teaching Hospital, Enugu: the role of foreign cardiac missions in 3.5 years”. Cardiology in the Young 27.6 (2017): 1174-1179.
- Iyaniwura Wole. “Corruption and Military Rule in Nigeria: An Overview, 1966-1999”. Global Journal of Human-Social Science & Political Science 14.2 (2014): 1-7.
- Whittle J and Kelleher A. “Preoperative Assessment for Cardiac Surgery”. Anaesthesia & Intensive Care Medicine16.10 (2015): 484-490.
- Scott IA., et al. “Perioperative Cardiac Evaluation and Management of patients undergoing non-Cardiac Surgery”. Medical Journal of Australia 199.10 (2013): 667-673.
- Johc C Eze., et al. “Pattern and Outcome of congenital heart defects managed over a year period at Innova Children Heart hospital, Hyderabad, India as a skill acquisition center”. A Journal on Surgery 30.1 (2017): 1-5.
- Nwafor IA., et al. “The Scope of Cardiac Surgery at a National Cardiothoracic Center of Excellence: A 3-year review”. Journal of Vascular Medicine & Surgery 5.2 (2017): 1-7.
- Satpathy M and Mishra BR. “Clinical Diagnosis of Congenital Heart Disease. First Edition: 2008”. Ajanta Offset and Packagings LTD (2008):
- Kannan BRJ and Kumar R Krishma. “Imaging /IAP Specialty Series in Pediatric Cardiolog. First Edition 2008”. Japee Brothers medical Publishers (2008):
- Gutherez C and Blanchard DG. “Atrial Fibrillation: Diagnosis and Treatment”. American Family Physician 83.1 (2011): 61-68.
- Col Kumar CB., et al. “Diagnostic Pediatric cardiac catheterization: Experience of a tertiary care pediatric cardiac center”. Medical Journal Armed Forces India 70.1 (2014): 10-16.
- Oldroyd KG., et al. “Cardiac catheterization by the Judkins technique as an outpatient procedure”. British Medical Journal298 (1989): 875-876.
- “Certificate of Need (CON) Review Standards for Cardiac Catherisation Services”. Michigan Department of Community Health (2015): 1-13.
- Zulhke L., et al. “Congenital heart disease and rheumatic heart disease in Africa: recent advances and current priorities”. Cardiology in Africa review series 99.21 (2013): 1554-1561.
- Munoz M., et al. “Preoperative haematological assessment scheduled for major surgery”. Anaesthesia 71.S1 (2016): 19-28.
- Barnard MA., et al. “Preoperative patient assessment: a review of the literature and recommendations”. Annals of the Royal College of Surgeons of England 76 (1994): 293-297.
- Kumar P., et al. “Preoperative International Normalized Ratio (INR) and Bleeding during Open-Heart Procedure”. Indian Journal of Thoracic and Cardiovascular Surgery 20.3 (2004): 132-134.
- Nwafor IA., et al. “Open Heart Surgery: Management of Nonsurgical Bleeding in the Perioperative Period; 3.5 Years Institutional Experience”. International Journal of Vascular Surgery and Medicine 3.1 (2017):
- Mowat IR and Keller AA. “Preoperative Assessment for Cardiac Surgery”. Anaesthesia and Intensive Care Medicine 13.10 (2012): 469-474.
Citation:
Nwafor IA., et al. “Changes in the Open Heart Surgery Protocol and Outcomes in a Nigerian National Cardiothoracic Center of
Excellence over 42 Years”. Therapeutic Advances in Cardiology 1.2 (2017): 97-104.
Copyright: © 2017 Nwafor IA., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.