Research Article
Volume 2 Issue 2 - 2018
The Utility of Ventricular Septal Rupture Size and Gradient Measured by Echocardiography in Assessing 14 Day Survival in Myocardial Infarction
1Department of Cardiology, Medical College Hospital, Trivandrum, KUHS University, India
2Department of Biostatistics, Regional Cancer Centre, Trivandrum, Kerala, India
2Department of Biostatistics, Regional Cancer Centre, Trivandrum, Kerala, India
*Corresponding Author: Prabha Nini Gupta, Department of Cardiology, Medical College Hospital, Trivandrum, KUHS University, India.
Received: June 19, 2018; Published: September 17, 2018
Abstract
Early surgery for ventricular septal rupture (VSR) has a higher mortality than delayed surgery. Analysis of factors to predict late survival would help predict which patients could wait for intervention.
Methods: A retrospective examination of admissions with STEMI from Jan 2008 to April 2014 fetched 29 cases of VSR. The patients presenting before 2013, were designated as Group 1 (15 patients). Of these 2 were successfully operated on. One is still alive, and one died one month after surgery. Two patients died within 12 hours of admission without echocardiograms. One patient presented to us in both 2004 and 2014.She may be the longest non surgically treated survivor till date. (2004 to 2014, 10 years) The data from the remaining 10 patients’ was included in a univariate and multivariate analysis. Group 2 was patients presenting after 2013. (14 patients) when the ACC recommended early surgery for patients with VSR. 3/14 patients died after open heart surgery. 11/14 died at various times after admission.
In all patients the age, sex, size of VSR, the gradient of the VSR and its position and the admission systolic blood pressure, admission ejection fraction, blood urea, serum creatinine, details of treatment like use of dobutamine, dopamine, nitroglycerine and heparin, IABP, Bipap ventilation, other ventilation, were recorded. The use of digoxin, Ace and beta-blockers were also recorded. The variables were tested comparing parameters associated with survival up to 72 hours and more than 72 hours till 14 days. The Student T test, Chi square test and Kaplan Meier survival curves were used in the analysis with Cox proportional hazards multiple regression.
Results: Patients in whom the size of the VSR remained static, and the gradient remained stable remained stable. A VSR gradient of more than 25 mm HG versus VSR gradient less than 25 mm Hg (p < .03) by X2 and log rank test (p < 0.01) predicted longer survival, (beyond 72 hours, up to 14 days). The unstable patients with constantly changing gradients (the gradients came down,) and the size of the VSR constantly increased (over the day) died early.
Conclusions: A VSR gradient of 25 mmHg or more and a smaller VSR predicts longer survival in a VSR patient. This data may be used to plan surgery or intervention.
Keywords: Ventricular Septal Rupture; Post-Myocardial Infarction Ventricular Septal Rupture; Complications of Stemi; Prognostic Indicators for Vsr; Echocardiography for Ventricular Septal Rupture;
Abbreviations: VSR: Ventricular Septal Rupture; STEMI: ST Elevation Myocardial Infarction; VSD: Ventricular Septal Defect;
Introduction
Ventricular septal rupture (VSR) is a dreaded complication of acute myocardial infarction. In most patients, post infarction VSR rapidly leads to worsening of the hemodynamic status and cardiogenic shock, intractable congestive heart failure (CHF), and fluid retention. Usually immediate surgery is indicated. The high surgical risk of early repair is accepted because of the even higher risk of death without surgery. It has even in the best hands almost 80% mortality. [1] Various techniques have been tried to salvage the patients with VSR.
Very early surgery usually ends in operative mortality as the edges of the VSR are friable and the sutures do not stay. If later surgery is planned an unstable patient may die before he can be taken for surgery. Hence a consensus where some patients are taken up as an emergency and others wait would be ideal. For this, knowledge of the indicators of more prolonged survival in VSR would aid decision making. Hirotani [2] has described a modified infarct Exclusion Technique which seems to have a better outcome. [2] He operated patients from 1 to 10 days after detection of the murmur and of these 9 patients, only one died of pneumonia at 50 days. This technique may reduce the mortality in these high risk patients.
In Kerala, India some patients refuse surgery when the chance of survival after surgery is poor. So we have a unique situation of having un-operated VSRs in whom we can attempt medical follow-up.
In this paper we do not attempt any device closure, we only attempt to show the clinical spectrum of VSR, its clinical stability or instability and the factors predicting early death. It is of necessity a small series as VSR is not as common as before.
The ACC guidelines 2013 recommend early surgery for ventricular septal rupture, (VSR). [3] But early surgery has a 50% mortality compared to a 20% mortality when patients are taken up after 3 weeks. So this paper attempts to assess which patients can wait and which patients need to be taken up early.
Materials and Methods
Aretrospective examination of admissions with STEMIfrom Jan 2008 to April 2014 fetched29 cases of VSR. The patients presenting before 2013, were designated as Group 1 (15 patients). Of these 2 were successfully operated on. One is still alive,and one died one month after surgery.Two patients died within 12 hours of admission withoutechocardiograms. One patient presented to us in both 2004 and 2014. She may be the longest non surgically treated survivor till date. (2004 to 2014,10 years) The data from the remaining 10 patients’ was included in a univariate and multivariate analysis. Group 2 was patients presenting after 2013. (14 patients)when the ACC recommended early surgery for patients with VSR. 3/14 patientsdied after open heart surgery. 11/14 died at various times after admission.
In all patients the age, sex, size of VSR, the gradient of the VSR and its position and the admission systolic blood pressure, admission ejection fraction, blood urea, serum creatinine, details of treatment like use of dobutamine, dopamine, nitroglycerine and heparin, IABP, Bipap ventilation, other ventilation, were recorded. The use of digoxin, Ace and beta-blockers were also recorded. The variables were tested comparing parameters associated with survival up to 72 hours and more than 72 hourstill 14 days.The Student T test, Chi square test and Kaplan Meier survival curves were used in theanalysis withCox proportional hazards multiple regression.
Results
The findings in 10 patients on univariate and multivariate analysis are described in Tables 1 and 2 (Group 1). One patient survived 25 days in the hospital and then went home. She is still alive in 2018. (Total survival now 4 years and 3 months) (Group 2)
| Variable | Group | Statistical significance P < 0.05 |
| Age | < 60yrs | 0.083 |
| Sex | Male | 0.1379 |
| Gradient across the VSR | > 25 mmHg | 0.0143 |
| Size of the VSR. | < 1 cm | 0.0833 |
| Systolic BP | > 80mmHg | 0.0039 |
| EF | > 50mmHg | 0.0143 |
| Blood urea | < 45 mg% | 0.0896 |
| S Creatinine | < 1.4 mg% | 0.0455 |
Table 1: Univariate Survival analysis by variables at the time of admission (Kaplan Meier Survival Curves compared by the log rank test).
| Drug used | Statistical significance |
| Heparin | 0.0213 |
| NTG | 0.0833 |
| Dopamine | 0.0896 |
| Carvedilol | 0.0833 |
| Dobutamine | 0.0833 |
| Aldactone/Eplerenone | 0.2253 |
| ACE inhibitor | 0.0455 |
Table 2: Drugs and the survival of VSR patients when the drugs were used as opposed to not used (Kaplan-Meier compared by log rank test).
We also present here 4 illustrative cases of ventricular septal rupture that we believe will throw light on what type of VSR would survive longer. We also show the follow up echo pictures of a patient who survived 51 months after a VSR and improved on Ramipril, carvedilol and diuretics. (From Group 2) We also report a long survivor who survived for 10 years since 2004. (Group 1)
Patient number one: was a 60 year old female patient who presented to the hospital in 2014, March, with acute anterior wall myocardial infarction. She had continuing pain and was shifted to the ICCU. She was not thrombolysed as on examination she had a heart rate of 92/minute, a blood pressure of 110/80 and mild cardiomegaly. She had a systolic thrill felt along her left sternal border. Her first heart sound was normal, her second heart sound was normally spit and her pulmonary component was loud. She has a grade 4/6 pansystolic murmur along the left lower sternal border. She was subjected to an echocardiogram: This showed an apical (Figures 1, 2, 3) ventricular septal rupture, the size was 0.8 cms and the gradient across this was 70 mm of Hg. Her other echocardiographic findings were: LVIDD/S-3.4/2.0, her ejection fraction was 71% she had RWMA in the anterior territory. Her initial blood urea was 40 mg which later rose to 84 mg/dl.
Her serum creatinine was .9 mg/dl that rose to 1.2 mg/dl. Her liver functions were mildly deranged SGOT was 142 IU /dl and SGPT was 137 iu/dl. She was initially put on intravenous nitroglycerine, but this had to be stopped on day two and she was put on intravenous dobutamine and dopamine. She was unstable so had be given intravenous furosemide (low doses 20 mg twice a day). She remained in the ICCU for 25 days, and since she seemed stable she was slowly put on carvedilol (initially 3.125 mg half a tablet alternate days, then Ramipril 1.25 mg, and aldactone 25 mg, and digoxin 0.25 mg half a tablet, five days by 7. Her relatives did not want surgery and thought she may die, so voluntarily took her home after 30 days of hospital admission. A repeat echocardiogram showed that even at 20 days her VSR size was still .8 cms and her gradient was 70 mm hg. (Figures 1,2,3,4) This patient (as shown in the figure) survived 25 days in the hospital and then went home. She is still alive. (June 2018) (From Group 2)
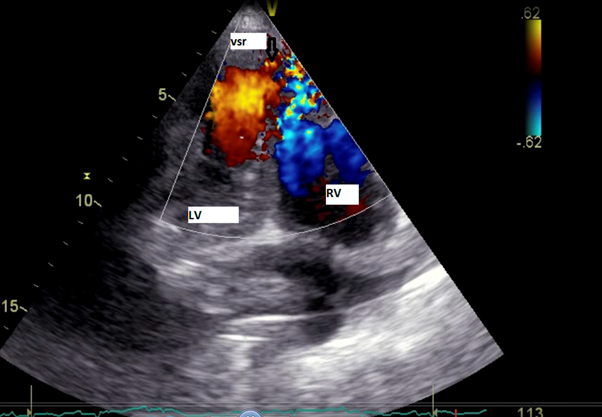
Figure 1: The color Doppler image of a patient who survived more than 3 weeks without surgery and is still alive. The color flow denotes the ventricular septal rupture.

Figure 2: The .8 cm VSR seen at the apex in the long survivor who presented in March 2014. She is still alive in June 2018. (4 years 3 months).
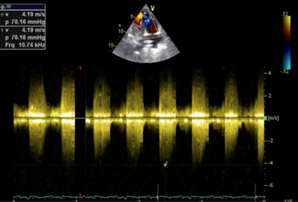
Figure 3: The gradient on day 1 on the same patient with ventricular septal rupture. She had the same gradient after 21 days and was then discharged.

Figure 4: A 2014 echo picture of the patient in figures 1 and 2 taken after 8 months of the index infarction. She has now lived 4 years, 3 months on carvedilol, Ramipril and digoxin. She was earlier in the ICCU for 25 days.
Case 2: was a male of 49 years who presented on day one with a large acute inferior wall myocardial infarction. His heart rate was 126/min, his blood pressure was initially 130/80 mm hg, He had mild cardiomegaly, His first heart sound was normal, his second heart sound was normally split, and his pulmonary second sound was loud. He had a loud third heart sound. His echocardiogram revealed a large ventricular septal rupture, size of 2-3 cms in the inferior septum and mid interventricular septum. His initial gradient was around 40 mm hg but this gradually fell to 20 mm hg, his VSR seemed to increase by the hour, and since he was unstable he was sent for surgery but he died in-spite of surgery 48 hours after surgery. His coronary angiogram showed that his LPDA (left posterior descending coronary artery) was blocked but his left anterior descending coronary artery was patent. His echocardiogram other findings were-LVIDD/S 3.71/1.54, his ejection fraction was 88%) (See the figures 5, 6, 7) (From Group 1)
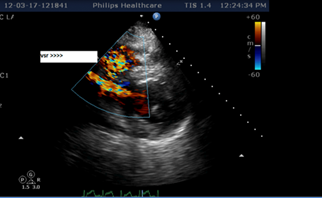
Figure 5: The color Doppler of the large VSR. This patient was unstable and his VSR was constantly enlarging.
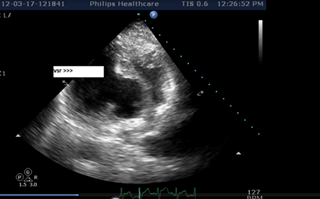
Figure 6: The echo picture of a large VSR, the patient deteriorated very fast his VSR was continuously enlarging and his gradient came down rapidly. He had an inferior wall MI. This type of patient is unstable.
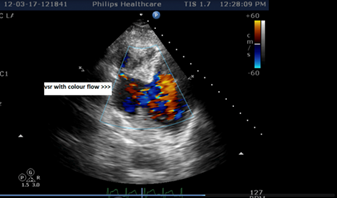
Figure 7: One of the patients with a large VSR. This patient was unstable. He died in-spite of surgery within 72 hours. He is the same patient as in figures 5 and 6.
Patient 3: Was a woman of 76 years age who had an CAD Anterior wall myocardial infarction, she was thrombolysed with intravenous streptokinase and she presented with a 0.6 mm apical VSR on day 1 of the myocardial infarction. Her admitting blood pressure was 80/60 mm hg and heart rate was 100/minute. She was not willing for any treatment but agreed to hospitalization for 2 weeks. Following discharge she died 10 days later. She did tolerate aldactone. No other drugs could be given. (Group 1)
Patient 4: Briefly: One patient, a 58 year old female, has survived on medical management for the last 10 years. She had presented in 2004 to the first author. Since she came for a repeat attack of congestive heart failure during the study period she was included in the study but not in the survival analysis. (Group 1)
Total survival: One patient has survived on medical management for the last 10 years. She presented to our hospital late and since she had a myocardial infarction, she was also included in the study. She had presented in 2004 to the first author. 4 patients with small ventricular septal defects (less than 0.9 cms) survived more than 2 weeks on medical therapy and two are still alive only on medical management. One surgical survivor is still alive.
Multivariate analysis: On multivariate analysis: on cox proportional hazards multiple regression the ventricular septal rupture gradient was the main predictor of survival.
A few more results: Patients with deranged liver function tests had a higher mortality.
The use of IABP: IABP was used in three patients but all expired. (Two patients in group 1 and 1 patient in group 2) The patient in Group 2 was willing for surgery but died suddenly waiting for the same.
Patients requiring Bipap ventilation and invasive ventilation has significantly higher mortality. (p < .01 and .004 respectively). The ventricular septal rupture was in the apical location in 81.5%. The VSR occurred in anterior wall myocardial infarctions in 72%.
Discussion
Various experts in the field have commented on the management of VSR. [1] They have commented that in the life of a cardiac surgeon, the incidence and the chance to operate a VSR occurs relatively infrequently. Even if the surgical expertise is good the over- all surgical outcome of operated cases is poor. (47% survival, in the Gusto 1 trial) [1,2]. In the SHOCK trial the operative mortality was 81%. [1] A later series has slightly better survival. [4]
Moore., et al. studied 25 ventricular septal ruptures over a 5.5 year period. [5] They found that most of the ventricular septal ruptures occurred between day 1 to day 7. Of the 25 patients in this series 14 died. (56%) This study was published in 1986. They found the predictors of early death were: more patients with inferior wall myocardial infarction died. Further if the patient had a cardiac index of less than 1.75 ml/m2/min they had more death. Non survivors had impaired RV function, more cardiogenic shock and higher right atrial pressures (more than 12 mm hg.) On echocardiography they had more wall motion abnormality of the interventricular septum. Again, echocardiography alone was helpful in demarcating the higher risk patients. We did a univariate analysis to analyze which factors were associated with a better survival. (Table 1)
Echocardiography and Survival
We found that a smaller size of ventricular septal rupture, less than 1 cm predicted a survival longer than 14 days. Further as soon as the urea and S creatinine started rising the patient would die. Further gradients of more than 25 mm across the VSR were good predictors of survival. We found that repeated echocardiograms were helpful in predicting survival. If the size of the VSR was stable and the gradient remained above 25 mm hg on repeated echocardiography the patient would be stable. But if the patient ‘s VSR continuously enlarged, in-spite of all measures (including cardiac surgery), the patient would die. (Table 2)
We found that a smaller size of ventricular septal rupture, less than 1 cm predicted a survival longer than 14 days. Further as soon as the urea and S creatinine started rising the patient would die. Further gradients of more than 25 mm across the VSR were good predictors of survival. We found that repeated echocardiograms were helpful in predicting survival. If the size of the VSR was stable and the gradient remained above 25 mm hg on repeated echocardiography the patient would be stable. But if the patient ‘s VSR continuously enlarged, in-spite of all measures (including cardiac surgery), the patient would die. (Table 2)
The other prognostic factor was the presence of a thrill. This also appeared to be a good prognostic sign. Both our long survivor and one of our surgical patients who survived had a thrill. Our patient illustrated here (Figures 1 and 2, 3, 4) had the same gradients even after 20 days. Our patients who had a rise in urea and S creatinine died soon after this started.
These findings have also been found in the SHOCK trial. Multiorgan failure was the predictor of death. [7] Venu Menon studied VSR as early as 2000. He reports the findings of the Shock Trial registry. Some case reports of delayed presentation and delayed closure of the VSR by surgery have been successful. [8]
Risseeuw comments on the advantage of having a greater time before either surgical or device closure. [9] The necrotic septum then stabilizes and gets scarred that may better hold sutures or devices. He has also classified the patients as before 14 days (Acute phase occlusion) versus after 14 days (chronic phase occlusion). The mortality in the acute phase was-42-100%. The mortality in the chronic phase was -20-38%. So like surgery it might be better to defer device closure, and so again it becomes crucial to know who would live longer.
VSR Localization and Per Cutaneous Closure
Risseeuw has also commented on which VSRs may not be not amenable for device closure. Those in the apical location or perivalvular locations may not be suitable for device closure. As in previous reports, he also comments that the mortality of VSRs associated with inferior wall myocardial infarction was higher than those associated with anterior wall MI. These VSRs have irregular margins, may have multiple channels and may be either simple or complex. [9]
Risseeuw has also commented on which VSRs may not be not amenable for device closure. Those in the apical location or perivalvular locations may not be suitable for device closure. As in previous reports, he also comments that the mortality of VSRs associated with inferior wall myocardial infarction was higher than those associated with anterior wall MI. These VSRs have irregular margins, may have multiple channels and may be either simple or complex. [9]
Yet another recent report seems to show that revascularization with device closure may the answer. [10] They found the factors associated with death were female sex, NYHA class IV, cardiogenic shock, elevated S creatinine levels, defect size, the use of inotropes, and the absence of revascularization for myocardial infarction were all associated with an increased risk of death. Post closure reduction in the shunt size and prior surgery for VSR were good prognostic factors for device closure.
Conclusions
- Post myocardial infarction ventricular septal ruptures seem relatively stable if their VSR size remains stable over time, or if their gradient remains stable and above 25 mm Hg.
- If the VSR keeps expanding in size, the patient will be unstable and should be taken up for surgery as early as possible.
- Inferior wall myocardial infarction VSRs have a worse prognosis compared to anterior wall VSRs.
- Once the patient starts having multiorgan damage like a rise in S creatinine or blood urea it is a rapid downhill course and the patient dies.
- Echocardiography, especially in the ICCU, is the only investigation that can be repeatedly be performed without risk to the patient and has a prognostic role in the outcomes of a ventricular septal rupture. It also helps rule out other mechanical complications of myocardial infarction.
References
- Murday A. “Optimal Management of Acute Ventricular Septal Rupture”. Heart 89.12 (2003): 1462-1466.
- Hirotani T and Nakamichi T. “A Modified Infarct Exclusion Technique for a Post-infarction Ventricular Septal Defect”. Ann Thorac Cardiovasc Surgery 8.5 (2002): 281-285.
- O’Gara TP., et al. “2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction”. Journal of the American College of Cardiology 61.4 (2013): 78-140.
- Pang P YK., et al. “Outcome and survival analysis of surgical repair of post-infarction ventricular septal rupture”. Journal of Cardiothoracic Surgery 8 (2013): 44.
- Moore CA., et al. “Post infarction ventricular septal rupture: the importance of location of infarction and right ventricular function in determining survival”. Circulation 74.1 (1986): 45-55.
- Assenza GE., et al. “Transcatheter Closure of Post-myocardial Infarction Ventricular Septal Rupture”. Circulation: Cardiovascular Interventions 6 (2013): 59-67.
- Menon V., et al. “Outcome and Profile of Ventricular Septal Rupture With Cardiogenic Shock After Myocardial Infarction: A Report from the SHOCK Trial Registry”. Journal of the American College of Cardiology 36 (2000): 1110-1116.
- Cho J H., et al. “Delayed ventricular septal rupture complicating acute inferior wall myocardial infarction”. BMC Research Notes 6 (2013): 124.
- Risseeuw F., et al.“Percutaneous occlusion of post-myocardial infarction ventricular septum rupture”. Netherlands Heart Journal 22 (2014): 47-51.
- Calvert PA., et al. “Percutaneous Closure of Post infarction Ventricular Septal Defect”. Circulation 129 (2014):
Citation:
Prabha Nini Gupta., et al. “The Utility of Ventricular Septal Rupture Size and Gradient Measured by Echocardiography in
Assessing 14 Day Survival in Myocardial Infarction”. Therapeutic Advances in Cardiology 2.2 (2018): 236-243.
Copyright: © 2018 Prabha Nini Gupta., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.