Research Article
Volume 5 Issue 1 - 2024
Safety Evaluation of Long-term Intake of Fermented Barley GABA 90% –A Placebo-controlled, Double-blind, Randomized, Parallel-group Comparative Trial–
1Research & Development Laboratory, Sanwa Shurui Co., Ltd., Usa, Oita, Japan
2Miura Clinic, Medical Corporation Kanonkai, Osaka, Japan
*Corresponding Author: Dr. Eriko Uehara, , Research & Development Laboratory, Sanwa Shurui Co., Ltd., 2231-1 Yamamoto, Usa, Oita 879-0495, Japan.
Abstract
Fermented barley GABA 90% (FB-GABA, Sanwa Shurui Co., Ltd., Japan) is a powdered product of γ-aminobutyric acid (GABA) produced by Enterococcus malodoratus FC 301 cultured in a medium of fermented barley extract (FBE) generated in the manufacture of shochu, a Japanese distilled liquor. GABA accounts for more than 90% of FB-GABA. The approximately 10% remaining contains components produced by FC 301 and those derived from FBE used as a medium. Consuming 200mg of GABA per day is known to improve cognitive function without any health risks. To consume 200mg/day of GABA, it is necessary to consume 223mg/day of FB-GABA. The Japanese Consumer Affairs Agency requires confirmation of the safety of long-term consumption (12 weeks or more) of foods for specified health uses. The objective of this study was to investigate the safety of consuming 223mg/day or more of FB-GABA for 13 weeks. Forty-eight participants were randomly divided into two groups. Each group ingested test tablets containing 268.4mg of FB-GABA or placebo tablets containing 268.4mg of dextrin for 13 weeks. The evaluation parameters included body measurements, physical examinations, and blood and urine tests. Medical interviews were also conducted by the principal investigator. The principal investigator judged that there were no safety issues with the long-term intake of FB-GABA for 13 weeks based on the primary endpoints of body measurements, physical examinations, blood and urine tests, and adverse events. These findings suggest the safety of long-term FB-GABA intake for 13 weeks.
Keywords: γ-aminobutyric acid; GABA; Fermented barley GABA; Safety test; Long-term intake
Abbreviations: SCR: Screening; BMI: Body Mass Index; WBC: White Blood Cell Count; Ht: Hematocrit; MCV: Mean Corpuscular Volume; MCHC: Mean Corpuscular Hemoglobin Concentration; AST: Aspartate Aminotransferase; ALT: Alanine Aminotransferase; Cre: Creatinine; HbA1c: Hemoglobin A1c; IP: Inorganic Phosphorus
Introduction
Gamma-aminobutyric acid (GABA) is an intrinsically safe amino acid found in plants and produced in the human body (De Bie., et al. 2023) that primarily functions as an inhibitory neurotransmitter (Bloom and Iversen, 1971). GABA is sold as a dietary supplement in the United States. A long-term intake trial (120mg of GABA/day for 12 weeks) showed no serious adverse events related to GABA (Oketch-Rabah., et al. 2021). Ingesting GABA brings about various physiological functions, for example, consuming 200mg/day of GABA improves cognitive function (Yamatsu., et al. 2020).
Fermented barley GABA 90% (FB-GABA, Sanwa Shurui Co., Ltd., Oita, Japan) is a product that is prepared by concentrating and powdering γ-aminobutyric acid (GABA) produced by Enterococcus malodoratus FC 301. FC 301 is cultured in a medium of fermented barley extract (FBE) generated in the manufacturing process of shochu, a Japanese distilled liquor (Furuta., et al. 2010). GABA accounts for more than 90% of FB-GABA, while components produced by FC 301 and those derived from FBE used as a medium constitute the remaining approximately 10%, although the ingredients in this 10% remain unknown. Ingestion of FB-GABA (equivalent to 100mg of GABA) has been reported to improve sleep quality (Hokazono and Fukuda, 2018), increase positive emotions (Hokazono and Saito, 2016), and improve skin elasticity (Hokazono and Uehara, 2016).
The consumption of GABA has been proven safe. FB-GABA is a fermented food that makes effective use of resources by utilizing shochu manufacturing by-products as a culture medium. However, the safety of the components other than GABA (unidentified fermentation products) contained in FB-GABA still needs to be investigated. FB-GABA was launched in August 2006, and since then, approximately 200 million servings have been sold. No health damage caused by FB-GABA has been reported. A placebo-controlled, double-blind, randomized, parallel-group trial in which 1341.9mg/day of FB-GABA (five times the effective intake amount) was ingested for 4 weeks confirmed that there were no safety issues (Uehara., et al. 2024). The Consumer Affairs Agency of Japan requires confirmation of the safety of long-term consumption (12 weeks or more) of foods for specified health uses (The Vice-Commissioner of Consumer Affairs Agency in Japan, 2014). However, the safety of long-term FB-GABA intake in humans has not been proven. Therefore, the purpose of the present trial was to determine the safety of daily FB-GABA intake over a 13-week period. In this trial, we assumed that a GABA-containing food with the effect of improving brain function was manufactured using FB-GABA as a raw material, and investigated the safety of ingesting 268.4mg/day of FB-GABA (200mg/day as GABA) for 13 weeks.
Materials and Methods
1. Trial Design
This placebo-controlled, double-blind, randomized, parallel-group trial protocol was reviewed and approved in terms of safety, efficacy, and ethics by the ethics review committee at Miura Clinic, Medical Corporation Kanonkai on March 17, 2022 (approval No.: R2113). Written informed consent was obtained from all participants. The trial was conducted in accordance with the spirit of the Declaration of Helsinki (revised in October 2013) and in compliance with the Ethical Guidelines for Medical and Biological Research Involving Human Subjects (Ministry of Education, Culture, Sports, Science and Technology/Ministry of Health, Labour and Welfare, March 23, 2021). Before starting the trial, we registered with the University Hospital Medical Information Network (UMIN) Clinical Trials Registry operated by the UMIN Center (UMIN-ID: UMIN000047209).
2. Participants
After obtaining informed consent from the participants, the following demographics were reviewed or confirmed: sex, age, medical history, surgical history, history of present illness, allergy, drinking habit and amount, smoking habit and amount, status of lifestyle and exercise habits, use status for drugs and health foods, and status of participation in other clinical trials or studies. The selection was decided by the principal investigator according to the inclusion and exclusion criteria, based on a review of the results of a screening (SCR) test and demographic data.
The participants were required to meet all of the inclusion criteria and none of the exclusion criteria as follows:
Inclusion Criteria
- Healthy male and female participants aged 20–64 years; and
- Participants who were fully informed of the objective and details of the trial, were capable of giving consent, fully understood the trial, volunteered to participate in the trial, and gave written consent to participate in the trial.
Exclusion Criteria
- Individuals with heart, liver, or kidney disease (including complications of other diseases);
- Individuals with a history of cardiovascular disease;
- Individuals with diabetes mellitus;
- Individuals currently being treated for a disease;
- Individuals with a food or drug allergy;
- Individuals with anemia symptoms;
- Women who wished to become pregnant or were pregnant (including possibly pregnant) or lactating while participating in the trial;
- Individuals who regularly visited a hospital or were receiving treatment with a drug or Chinese herbal medicine for a certain disease (drugs on an as-needed basis were permitted);
- Individuals who engaged in strenuous sports or diets;
- Individuals with an extremely irregular diet;
- Individuals who could not discontinue the intake of health foods (including foods for specified health uses or with functional claims) or designated quasi-pharmaceutical products during the trial period;
- Individuals who drank over 60g/day of net alcohol on average;
- Individuals who smoked 21 or more cigarettes/day on average;
- Individuals who were participating or planning to participate in another clinical trial at the start of this trial;
- Individuals who had been vaccinated against influenza, the novel coronavirus, or other infectious diseases within 1 month before SCR; and
- Individuals who were judged by the principal investigator or sub-investigator to be ineligible to participate in the trial.
Target Sample Size and Rationale
The target sample size required to confirm the safety of the trial was determined to be 24 participants per group, for a total of 48 participants, taking changes in laboratory test values and adverse events into account.
3. Randomization
The allocation manager created a trial food allocation table in which the participants were randomly divided into a test food group and a placebo food group based on age group, sex, and body mass index (BMI). After completing the allocation, the allocation manager sealed the trial food allocation table in an envelope and wrote the trial title ID and sealing date on the envelope. To ensure blinding, the allocation manager then stored the sealed trial food allocation table in a strict manner until the end of the trial.
4. Trial Foods
The test food contained 134.19mg (120.7mg as GABA) of FB-GABA per tablet. The placebo food contained dextrin instead of FB-GABA. The recommended intake for FB-GABA is set at 13.7–223mg (GABA equivalent: 12.3–200mg). We selected 268.4mg/day in consideration of an overage of approximately 20%. We set the intake term for 13 weeks in accordance with Attachment 2 “Points to consider in preparing application forms for foods for specified health uses” for the labeling permission of foods for specified health uses (Food Labeling Division Notification No. 259).10)
5. Blinding
As this was a double-blind trial, both the participants and investigators were blinded to the treatment. The test and placebo tablets were visually indistinguishable from one another. The package bags were numbered by the manufacturer and neither the investigators nor the participants knew what number belonged to the test or placebo food.
6. Interventions
After the pre-dose Week 0 examination, the participants ate their assigned trial food for 13 weeks. At 4, 8 and 13 weeks after the start of intake, predetermined interviews and examinations were carried out.
The participants consumed two trial food tablets per day with water or warm water. Carryover to the next day was prohibited in the case a participant was unable to consume the trial food on that day. On the examination day (Weeks 4 and 8), the participants consumed the trial food after testing was complete.
From 1 week before the start of intake until the day of examination at Week 13, the participants were instructed to record the intake status of the trial food along with their physical condition, intake of drugs, drinking status, and exercise status in a daily life diary (on the Web or paper).
The following instructions were provided to the participants.
During the Trial Period
- Do not make significant changes to your lifestyle, such as diet, alcohol intake, exercise, bedtime, and smoking habit, before or during the trial period.
- Avoid excessive exercise or temperance in eating and overeating that deviate from the normal range in your daily life.
- In principle, the ingestion of medicinal products (including over-the-counter and prescription drugs), designated quasi-pharmaceutical products, and health foods (including foods for specified health uses and foods with functional claims) is prohibited. For medicinal products, the use of topical agents is also prohibited, in principle. If using such products is unavoidable because of a poor physical condition or other reasons, please consult with the contract research organization in advance.
- Alcohol consumption and excessive exercise are prohibited from the day before the examination to the completion of the examination on that day.
- On the day before the examination, eating and drinking should be completed by 22:00, and fasting should be continued until the examination is completed (the intake of water or lukewarm water is permitted).
- On the day of the examination, please visit the trial site without taking the trial food.
- Immediately notify the person in charge of the trial if receiving a vaccination. If a symptom such as heaviness of the body, headache, chills, fever, joint pain, nausea, vomiting, or diarrhea occurs, the principal investigator will determine whether to continue dosing after checking your symptoms. If dosing is continued, whether the symptom is attributable to the test article will be verified through a comparison with the placebo group.
- Immediately notify the person in charge of the trial if you test positive for the novel coronavirus.
Test Items and Timing
In this trial, body measurements (body weight and BMI), physical examinations, and laboratory tests (blood and urine tests) at SCR, pre-dose Week 0, Week 4, Week 8 and Week 13 were conducted under direction of the principal investigator or subinvestigator. Height was measured only at the time of SCR, and was taken as the value measured at Week 0. The blood tests items were hematology (white blood cell count [WBC], red blood cell count, hemoglobin, hematocrit [Ht], mean corpuscular volume [MCV], mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration [MCHC] and platelet count) and blood biochemistry (uric acid, urea nitrogen, aspartate aminotransferase/glutamic oxaloacetic transaminase [AST/GOT], alanine aminotransferase/glutamic pyruvic transaminase [ALT/GPT], gamma-glutamyl transpeptidase, alkaline phosphatase, lactate dehydrogenase, total bilirubin, total protein, albumin, creatinine [Cre], creatine kinase, serum amylase, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglyceride, blood glucose, hemoglobin A1c [HbA1c], Sodium [Na], Chloride [Cl], potassium, magnesium [Mg], calcium, iron [Fe], and inorganic phosphorus [IP]).
Urine test items were protein qualitative, glucose qualitative, urobilinogen qualitative, bilirubin qualitative, occult blood reaction qualitative, ketone body qualitative, specific gravity and pH. In various qualitative tests, the presence of the desired component was indicated as positive (+), and the more (+) there were, the higher the content of the component. False-positive cases were expressed as (±), and numbers represented the number of applicable people. On SCR, pre-dose Week 0, Week 4, Week 8, and Week 13, the principal investigator, sub-investigator, or nurse under the direction of the principal investigator performed medical interviews and recorded the results (significant figures: in accordance with the reference range of each test value). When adverse events occurred during the period from the start of intake to the end of the trial, a list of symptoms, date of onset and resolution, severity of symptoms, seriousness (need for emergency response), treatment, outcome, causal relationship with the trial food, and principal investigator’s comments was recorded. In principle, follow-up was to be performed as necessary until the abnormal findings of the adverse event resolved or showed a recovering trend.
Recruitment and Trial Period
Recruitment began on March 17, 2022, and the trial period ended on July 31, 2022.
Analysis Set and Statistical Analysis Methods
- Data Lock: After completion of the final examination, data lock was performed after all data and their handling were fixed and after the analysis set was confirmed.
- Opening of the trial food allocation table: The allocation manager opened the trial food allocation table under the instruction of the principal investigator after determining the handling for tabulation and analysis and confirming that the data were locked.
- Software used for tabulation and analysis: IBM SPSS Statistics (version 28; IBM Japan Ltd., Tokyo, Japan), JMP 12 (Institute Japan Ltd., Tokyo, Japan), and R (version 3; R Development Core Team, Auckland, New Zealand) were used for the data tabulation and analysis.
- Participant Demographics Summary statistics (mean ± standard deviation [SD]) were calculated and tabulated for the participant demographics (age, sex, height, body weight, systolic and diastolic blood pressure, and pulse). Between-group and between-sex comparisons were performed using a two-sample t-test and the chi-square test, respectively.
- Test Values Summary statistics (mean ± SD) were calculated for body measurements, physical examinations, and laboratory tests (hematology and blood biochemistry, and urinalysis). Measured values at Weeks 4, 8, and 13 were compared with those at pre-dose Week 0 using a Bonferroni-corrected paired t-test for evaluation. Body measurement, physical examination, and laboratory test values at each measurement time point were compared between the test and placebo food groups using an unpaired t-test. The testing was two-sided, with a significance level of 5%. For qualitative parameters of urinalysis, cross-tabulation tables were prepared for evaluation.
- Adverse events, subjective symptoms/objective findings, intake status of drugs/health foods, and trial food intake rate.
Adverse events, subjective symptoms/objective findings (medical interviews), intake status of drugs/health foods, and trial food intake rate were tabulated and evaluated. The intake rate was calculated by dividing the number of intakes by the number of intakes that should have been taken.
Results
1. Changes in Participants
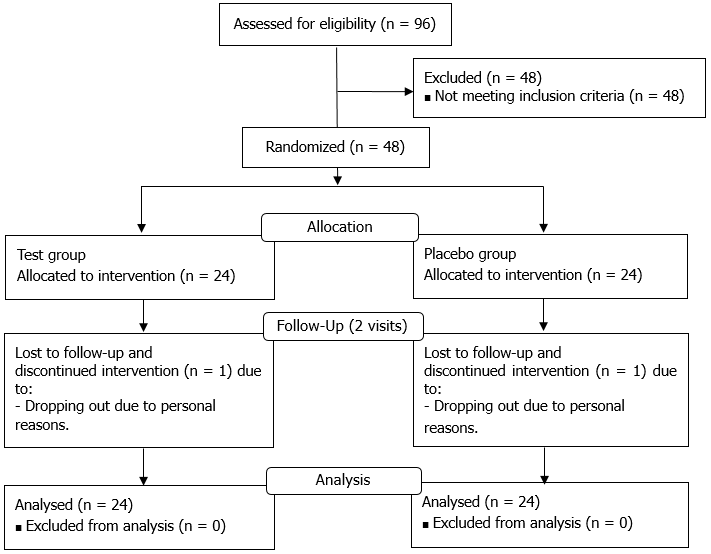
Of 96 participants who provided written informed consent, 48 were excluded on SCR, leaving 48 participants who met the inclusion criteria. Among these participants, two (ID13057 and ID13069) dropped out of the trial for personal reasons after randomization. No deviation or discontinuation occurred in any other participant (Figure 1).
2. Participant Demographics
Table 1 shows the participants’ demographics. No statistically significant differences were observed between the two groups.
| Group | n | Pretrial | ||||
| Age | (years) | Test | 24 | 44.1 | ± | 10.9 |
| Placebo | 24 | 43.4 | ± | 10.4 | ||
| Male | Test | 12 | ||||
| Placebo | 12 | |||||
| Female | Test | 12 | ||||
| Placebo | 12 | |||||
| Height | (cm) | Test | 24 | 166.87 | ± | 6.44 |
| Placebo | 24 | 164.91 | ± | 8.24 | ||
| Body weight | (kg) | Test | 24 | 61.44 | ± | 8.37 |
| Placebo | 24 | 60.37 | ± | 7.40 | ||
| Body mass index | (kg/m2) | Test | 24 | 21.99 | ± | 2.04 |
| Placebo | 24 | 22.14 | ± | 1.41 | ||
| Systolic blood pressure | (mmHg) | Test | 24 | 117.6 | ± | 10.8 |
| Placebo | 24 | 113.8 | ± | 10.5 | ||
| Diastolic blood pressure | (mmHg) | Test | 24 | 75.4 | ± | 8.6 |
| Placebo | 24 | 72.6 | ± | 8.7 | ||
| Pulse rate | (beats/min) | Test | 24 | 71.8 | ± | 9.8 |
| Placebo | 24 | 73.8 | ± | 9.4 | ||
Values are expressed as mean ± standard deviation (excluding the number of participants and sex). “N” refers to the number of applicable participants. Between-group comparisons were performed using a two-sample t-test, and between- sex comparisons were performed using the chi-square test. No significant differences between groups were found for any items.
Table 1: Participant demographics
3. Participants Analyzed
No participants met the exclusion criteria for analysis; therefore, all participants were included in the analysis.
4. Trial Food Intake Rate
The mean± SD intake rate for the trial food was 99.3% ± 1.4% in the placebo food group and 97.8% ± 3.7% in the test food group.
5. Body Measurements and Physical Examinations
Table 2 shows the results of body measurements and physical examinations. A comparison with pre-dose Week 0 showed significant trends in body weight and BMI at Week 13 in the placebo food group. Between-group comparisons showed a significant trend in systolic blood pressure at Week 4. No other significant differences or trends were observed for the other items.
| P-value (intragroup) | P-value (between-group) |
||||||||||||||||||||||
| Group | Week 0 | Week 4 | Week 8 | Week 13 | Week 4 | Week 8 | Week 13 | Week 0 | Week 4 | Week 2 | Week 13 | ||||||||||||
| Height | (cm) | Test | 166.87 | ± | 6.44 | - | - | - | - | - | - | 0.36 | - | - | - | ||||||||
| Placebo | 164.91 | ± | 8.24 | - | - | - | - | - | - | ||||||||||||||
| Body weight | (kg) | Test | 61.16 | ± | 8.43 | 61.51 | ± | 8.44 | 61.50 | ± | 8.58 | 61.10 | ± | 8.66 | 0.18 | 0.84 | 1.00 | 0.62 | 0.56 | 0.45 | 0.50 | ||
| Placebo | 60.01 | ± | 7.35 | 60.13 | ± | 7.57 | 59.72 | ± | 7.43 | 59.46 | ± | 7.42 | 1.00 | 0.19 | 0.07 | † | |||||||
| Body mass index | (kg/m2) | Test | 21.89 | ± | 2.12 | 22.02 | ± | 2.15 | 22.01 | ± | 2.19 | 21.85 | ± | 2.16 | 0.17 | 0.86 | 1.00 | 0.83 | 0.95 | 0.75 | 0.84 | ||
| Placebo | 22.00 | ± | 1.37 | 21.98 | ± | 1.54 | 21.83 | ± | 1.49 | 21.74 | ± | 1.48 | 1.00 | 0.23 | 0.09 | † | |||||||
| Systolic blood pressure | (mmHg) | Test | 116.2 | ± | 12.0 | 120.1 | ± | 12.0 | 119.8 | ± | 13.0 | 117.9 | ± | 11.8 | 0.25 | 0.45 | 1.00 | 0.83 | 0.08 | † | 0.13 | 0.45 | |
| Placebo | 115.4 | ± | 11.9 | 114.2 | ± | 10.6 | 113.7 | ± | 14.2 | 115.1 | ± | 13.1 | 1.00 | 0.63 | 1.00 | ||||||||
| Diastolic blood pressure | (mmHg) | Test | 71.6 | ± | 9.2 | 72.6 | ± | 10.5 | 72.5 | ± | 11.1 | 74.0 | ± | 9.1 | 1.00 | 1.00 | 0.30 | 0.83 | 0.42 | 0.21 | 0.27 | ||
| Placebo | 71.1 | ± | 8.7 | 70.4 | ± | 7.6 | 68.9 | ± | 8.2 | 71.2 | ± | 8.2 | 1.00 | 0.45 | 1.00 | ||||||||
| Pulse rate | (beats/min) | Test | 75.2 | ± | 13.1 | 74.4 | ± | 10.5 | 76.0 | ± | 11.3 | 76.0 | ± | 12.0 | 1.00 | 1.00 | 1.00 | 0.91 | 0.82 | 0.59 | 0.61 | ||
| Placebo | 75.6 | ± | 14.6 | 75.1 | ± | 12.2 | 74.3 | ± | 10.5 | 74.2 | ± | 11.7 | 1.00 | 1.00 | 1.00 | ||||||||
Values are expressed as mean ± standard deviation. Significant trends in a Bonferroni-corrected paired t-test of intragroup changes are expressed as †p < 0.10. The number of participants analyzed for each measurement item was 24.
Table 2: Results of body measurement and physical examination
6. Laboratory Tests
Tables 3–5 present the laboratory test results. Table 6 shows the p-values between the groups. A comparison with pre-dose Week 0 showed significant differences in MCV and MCHC at Week 4, Ht, MCV, MCHC, and Mg at Week 8, and Ht, MCV, MCHC, albumin, HbA1c, and Mg at Week 13, and significant trends in Ht, Cre, and HbA1c at Week 4 and in Cre at Week 13 in the test food group. No other significant differences or trends were observed for the other items. In the placebo food group, on the other hand, significant differences in MCV, HbA1c, Cl, and Mg were observed at Week 4, MCV and MCHC at Week 8, and MCV, MCHC, AST, HbA1c, Na, and Mg at Week 13; significant trends were noted in MCHC and ALT at Week 4, Na and Mg at Week 8, and Cre at Week 13. No other significant differences or trends were observed for the other items.
| P-value (intragroup) | ||||||||||||||||||||||
| Hematology | Reference range | Group | Week 0 | Week 4 | Week 8 | Week 13 | Week 4 | Week 8 | Week 13 | |||||||||||||
| White blood cell count | 3300 - 9000 | /μL | Test | 5387.5 | ± | 1001.0 | 5937.5 | ± | 1179.8 | 5608.3 | ± | 1003.9 | 5408.7 | ± | 1321.8 | 0.11 | 0.25 | 1.00 | ||||
| Placebo | 5054.2 | ± | 965.0 | 5204.3 | ± | 885.0 | 5226.1 | ± | 1158.1 | 5382.6 | ± | 1256.9 | 0.20 | 0.96 | 0.39 | |||||||
| Red blood cell count | Male | 430-570 | ×104/μL | Test | 461.9 | ± | 49.1 | 459.9 | ± | 50.6 | 461.4 | ± | 50.5 | 460.9 | ± | 49.9 | 1.00 | 1.00 | 1.00 | |||
| cell count | Female | 380-500 | Placebo | 471.7 | ± | 39.8 | 468.2 | ± | 43.2 | 471.5 | ± | 43.5 | 467.0 | ± | 38.9 | 0.94 | 1.00 | 0.51 | ||||
| Hemoglobin | Male | 13.5-17.5 | g/dL | Test | 14.08 | ± | 1.46 | 14.00 | ± | 1.51 | 14.05 | ± | 1.46 | 14.13 | ± | 1.48 | 1.00 | 1.00 | 1.00 | |||
| Female | 11.5-15.0 | Placebo | 14.29 | ± | 1.29 | 14.17 | ± | 1.41 | 14.22 | ± | 1.33 | 14.18 | ± | 1.17 | 1.00 | 1.00 | 1.00 | |||||
| Hematocrit | Male | 39.7-52.4 | % | Test | 43.56 | ± | 3.91 | 44.35 | ± | 4.30 | 44.57 | ± | 4.12 | 44.91 | ± | 4.35 | 0.07 | † | 0.010 | * | 0.02 | * |
| Female | 34.8-45.0 | Placebo | 44.32 | ± | 3.80 | 44.45 | ± | 3.72 | 45.20 | ± | 3.80 | 44.93 | ± | 3.34 | 1.00 | 0.15 | 0.43 | |||||
| MCV | 85 - 102 | fL | Test | 94.4 | ± | 3.7 | 96.5 | ± | 3.2 | 96.7 | ± | 3.3 | 97.6 | ± | 3.5 | <0.0001 | * | <0.0001 | * | <0.0001 | * | |
| Placebo | 94.0 | ± | 4.3 | 95.2 | ± | 4.3 | 96.1 | ± | 4.0 | 96.3 | ± | 4.2 | 0.007 | * | <0.0001 | * | <0.0001 | * | ||||
| MCH | 28.0-34.0 | pg | Test | 30.51 | ± | 1.24 | 30.48 | ± | 1.25 | 30.48 | ± | 1.28 | 30.70 | ± | 1.21 | 1.00 | 1.00 | 0.30 | ||||
| Placebo | 30.33 | ± | 1.60 | 30.30 | ± | 1.58 | 30.20 | ± | 1.57 | 30.40 | ± | 1.39 | 1.00 | 1.00 | 1.00 | |||||||
| MCHC | 30.2-35.1 | % | Test | 32.28 | ± | 0.87 | 31.55 | ± | 0.84 | 31.50 | ± | 0.86 | 31.46 | ± | 0.75 | 0.0003 | * | <0.0001 | * | 0.001 | * | |
| Placebo | 32.25 | ± | 0.79 | 31.85 | ± | 0.90 | 31.46 | ± | 0.90 | 31.54 | ± | 0.69 | 0.055 | † | 0.0001 | * | 0.003 | * | ||||
| Platelet count | 14.0-34.0 | ×104/μL | Test | 28.08 | ± | 4.59 | 28.22 | ± | 4.56 | 27.91 | ± | 4.05 | 28.30 | ± | 5.17 | 1.00 | 1.00 | 1.00 | ||||
| Placebo | 25.53 | ± | 6.50 | 25.61 | ± | 6.13 | 24.71 | ± | 5.99 | 25.40 | ± | 6.60 | 1.00 | 0.22 | 1.00 | |||||||
Values are expressed as mean ± standard deviation. Parameters separated by sex are indicated by results for each sex only. MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration. Significant differences in a Bonferroni-corrected paired t-test of intragroup changes are expressed as *p < 0.05 and †p < 0.10. The number of participants analyzed for each measurement item was 24.
Table 3: Laboratory test results
| Blood biochemistry | Reference range | Group | Week 0 | Week 4 | Week 8 | Week 13 | Week 4 | Week 8 | Week 13 | |||||||||||||
| Uric acid | Male | 3.8 - 7.0 | mg/dL | Test | 5.08 | ± | 1.24 | 5.16 | ± | 1.21 | 5.30 | ± | 1.40 | 5.27 | ± | 1.29 | 1.00 | 0.37 | 0.22 | |||
| Female | 2.5 - 7.0 | Placebo | 5.01 | ± | 1.19 | 5.16 | ± | 1.23 | 4.96 | ± | 1.21 | 5.11 | ± | 1.14 | 1.00 | 0.68 | 1.00 | |||||
| Urea nitrogen | 8.0 - 20.0 | mg/dL | Test | 13.28 | ± | 3.35 | 12.80 | ± | 3.16 | 12.97 | ± | 2.88 | 12.34 | ± | 2.67 | 1.00 | 1.00 | 0.84 | ||||
| Placebo | 13.47 | ± | 4.35 | 12.93 | ± | 3.93 | 12.90 | ± | 4.29 | 13.50 | ± | 4.96 | 0.40 | 0.34 | 1.00 | |||||||
| AST | 10 - 40 | U/L | Test | 19.6 | ± | 4.1 | 19.8 | ± | 4.7 | 19.5 | ± | 5.0 | 18.6 | ± | 4.6 | 1.00 | 1.00 | 0.23 | ||||
| Placebo | 18.3 | ± | 4.8 | 19.2 | ± | 4.1 | 18.0 | ± | 3.6 | 17.0 | ± | 3.5 | 0.85 | 0.79 | 0.03 | * | ||||||
| ALT | 5 - 45 | U/L | Test | 15.7 | ± | 5.8 | 15.6 | ± | 6.7 | 16.7 | ± | 8.1 | 15.5 | ± | 7.7 | 1.00 | 1.00 | 1.00 | ||||
| Placebo | 14.2 | ± | 8.5 | 16.5 | ± | 9.5 | 14.4 | ± | 7.7 | 14.6 | ± | 8.2 | 0.10 | † | 1.00 | 1.00 | ||||||
| γ-GT | Male | ≤80 | U/L | Test | 21.9 | ± | 9.9 | 22.5 | ± | 11.0 | 21.9 | ± | 12.1 | 21.3 | ± | 11.0 | 1.00 | 1.00 | 1.00 | |||
| Female | ≤30 | Placebo | 22.1 | ± | 13.1 | 24.3 | ± | 12.8 | 21.3 | ± | 12.8 | 20.7 | ± | 10.2 | 0.26 | 0.72 | 0.32 | |||||
| ALP | 38 - 113 | U/L | Test | 67.8 | ± | 18.9 | 69.1 | ± | 18.7 | 68.6 | ± | 18.7 | 67.7 | ± | 19.7 | 0.79 | 1.00 | 1.00 | ||||
| Placebo | 64.4 | ± | 17.1 | 67.2 | ± | 18.3 | 66.7 | ± | 19.0 | 66.4 | ± | 23.0 | 0.50 | 1.00 | 1.00 | |||||||
| LDH | 124 - 222 | U/L | Test | 183.5 | ± | 30.1 | 181.7 | ± | 27.5 | 184.8 | ± | 31.5 | 186.1 | ± | 30.5 | 1.00 | 1.00 | 0.77 | ||||
| Placebo | 180.0 | ± | 24.6 | 178.8 | ± | 19.2 | 179.7 | ± | 25.4 | 178.7 | ± | 21.1 | 0.78 | 1.00 | 0.66 | |||||||
| Total bilirubin | 0.2 - 1.2 | mg/dL | Test | 0.85 | ± | 0.29 | 0.80 | ± | 0.30 | 0.84 | ± | 0.27 | 0.93 | ± | 0.40 | 1.00 | 1.00 | 1.00 | ||||
| Placebo | 0.93 | ± | 0.29 | 0.92 | ± | 0.29 | 0.86 | ± | 0.23 | 0.98 | ± | 0.33 | 1.00 | 0.28 | 1.00 | |||||||
| Total protein | 6.7 - 8.3 | g/dL | Test | 7.18 | ± | 0.31 | 7.29 | ± | 0.35 | 7.22 | ± | 0.31 | 7.23 | ± | 0.37 | 0.32 | 0.78 | 1.00 | ||||
| Placebo | 7.18 | ± | 0.44 | 7.18 | ± | 0.44 | 7.05 | ± | 0.45 | 7.06 | ± | 0.40 | 1.00 | 0.32 | 0.15 | |||||||
| Albumin | 3.8-5.2 | g/dL | Test | 4.54 | ± | 0.22 | 4.59 | ± | 0.27 | 4.62 | ± | 0.24 | 4.63 | ± | 0.23 | 0.92 | 0.14 | 0.04 | * | |||
| Placebo | 4.55 | ± | 0.31 | 4.56 | ± | 0.30 | 4.58 | ± | 0.31 | 4.55 | ± | 0.29 | 1.00 | 1.00 | 1.00 | |||||||
| Cre | Male | 0.61-1.04 | mg/dL | Test | 0.751 | ± | 0.163 | 0.776 | ± | 0.166 | 0.762 | ± | 0.167 | 0.786 | ± | 0.182 | 0.08 | † | 0.94 | 0.09 | † | |
| Female | 0.47-0.79 | Placebo | 0.770 | ± | 0.168 | 0.789 | ± | 0.161 | 0.781 | ± | 0.154 | 0.806 | ± | 0.189 | 1.00 | 1.00 | 0.09 | † | ||||
| CK | Male | 60-270 | U/L | Test | 107.8 | ± | 40.5 | 124.8 | ± | 79.5 | 116.7 | ± | 50.2 | 123.7 | ± | 47.2 | 0.59 | 0.69 | 0.13 | |||
| Female | 40-150 | Placebo | 127.8 | ± | 91.0 | 120.0 | ± | 60.1 | 125.2 | ± | 82.9 | 110.6 | ± | 54.7 | 1.00 | 1.00 | 0.39 | |||||
| Serum amylase | 40-122 | U/L | Test | 79.5 | ± | 22.9 | 79.3 | ± | 22.0 | 78.8 | ± | 24.1 | 74.6 | ± | 19.0 | 1.00 | 1.00 | 0.33 | ||||
| Placebo | 78.1 | ± | 21.0 | 77.8 | ± | 19.7 | 79.3 | ± | 19.2 | 78.2 | ± | 21.4 | 1.00 | 1.00 | 1.00 | |||||||
| Total-Cho | 120-219 | mg/dL | Test | 208.5 | ± | 25.7 | 213.0 | ± | 27.1 | 212.3 | ± | 26.0 | 205.6 | ± | 27.6 | 0.87 | 0.94 | 1.00 | ||||
| Placebo | 202.9 | ± | 25.2 | 208.3 | ± | 25.1 | 203.4 | ± | 26.7 | 201.9 | ± | 29.2 | 0.77 | 1.00 | 1.00 | |||||||
| HDL-Cho | Male | 40-85 | mg/dL | Test | 68.8 | ± | 15.4 | 70.2 | ± | 14.1 | 69.1 | ± | 15.8 | 68.7 | ± | 17.5 | 1.00 | 1.00 | 1.00 | |||
| Female | 40-95 | Placebo | 67.7 | ± | 14.1 | 67.5 | ± | 14.6 | 66.7 | ± | 11.8 | 66.6 | ± | 12.4 | 1.00 | 0.75 | 0.38 | |||||
| LDL-Cho | 65-139 | mg/dL | Test | 120.5 | ± | 21.3 | 124.0 | ± | 27.2 | 121.8 | ± | 24.7 | 119.2 | ± | 25.4 | 0.89 | 1.00 | 1.00 | ||||
| Placebo | 119.0 | ± | 25.2 | 123.4 | ± | 25.2 | 118.2 | ± | 24.0 | 117.2 | ± | 26.2 | 0.44 | 1.00 | 1.00 | |||||||
| Triglyceride | 30-149 | mg/dL | Test | 89.7 | ± | 56.5 | 86.0 | ± | 43.7 | 118.8 | ± | 159.7 | 81.5 | ± | 50.0 | 1.00 | 1.00 | 0.39 | ||||
| Placebo | 80.7 | ± | 45.3 | 93.1 | ± | 52.6 | 83.9 | ± | 45.0 | 85.0 | ± | 34.9 | 0.42 | 1.00 | 1.00 | |||||||
| Blood glucose | 70-109 | mg/dL | Test | 88.9 | ± | 8.8 | 87.8 | ± | 9.7 | 87.2 | ± | 7.7 | 88.0 | ± | 10.8 | 0.79 | 0.49 | 1.00 | ||||
| Placebo | 87.5 | ± | 6.7 | 86.4 | ± | 7.5 | 86.9 | ± | 6.9 | 88.6 | ± | 9.5 | 1.00 | 1.00 | 1.00 | |||||||
| HbA1c | 4.6-6.2 | % | Test | 5.33 | ± | 0.27 | 5.28 | ± | 0.30 | 5.34 | ± | 0.25 | 5.13 | ± | 0.29 | 0.09 | † | 1.00 | <0.0001 | * | ||
| Placebo | 5.39 | ± | 0.24 | 5.33 | ± | 0.20 | 5.41 | ± | 0.19 | 5.19 | ± | 0.18 | 0.015 | * | 1.00 | <0.0001 | * | |||||
| Na | 137-147 | mEq/L | Test | 140.9 | ± | 1.7 | 141.0 | ± | 1.6 | 141.0 | ± | 1.3 | 140.1 | ± | 1.4 | 1.00 | 1.00 | 0.11 | ||||
| Placebo | 141.0 | ± | 1.8 | 141.1 | ± | 1.9 | 141.6 | ± | 1.9 | 140.0 | ± | 1.6 | 1.00 | 0.08 | † | 0.003 | * | |||||
| Cl | 98-108 | mEq/L | Test | 104.2 | ± | 2.0 | 104.1 | ± | 2.1 | 103.9 | ± | 1.8 | 103.9 | ± | 1.9 | 1.00 | 1.00 | 1.00 | ||||
| Placebo | 104.2 | ± | 2.3 | 104.7 | ± | 1.9 | 104.5 | ± | 1.8 | 104.1 | ± | 2.2 | 0.03 | * | 1.00 | 1.00 | ||||||
| K | 3.5-5.0 | mEq/L | Test | 4.20 | ± | 0.22 | 4.21 | ± | 0.24 | 4.14 | ± | 0.22 | 4.19 | ± | 0.26 | 1.00 | 0.95 | 1.00 | ||||
| Placebo | 4.11 | ± | 0.18 | 4.17 | ± | 0.16 | 4.15 | ± | 0.24 | 4.07 | ± | 0.23 | 0.91 | 1.00 | 0.58 | |||||||
| Mg | 1.9-2.5 | mg/dL | Test | 2.02 | ± | 0.12 | 2.05 | ± | 0.15 | 2.11 | ± | 0.17 | 2.15 | ± | 0.12 | 0.49 | 0.008 | * | <0.0001 | * | ||
| Placebo | 2.04 | ± | 0.11 | 2.11 | ± | 0.12 | 2.10 | ± | 0.12 | 2.12 | ± | 0.13 | 0.006 | * | 0.07 | † | 0.006 | * | ||||
| Ca | 8.4-10.4 | mg/dL | Test | 9.27 | ± | 0.38 | 9.35 | ± | 0.43 | 9.31 | ± | 0.36 | 9.41 | ± | 0.30 | 0.72 | 1.00 | 0.29 | ||||
| Placebo | 9.30 | ± | 0.34 | 9.27 | ± | 0.29 | 9.28 | ± | 0.34 | 9.36 | ± | 0.28 | 1.00 | 1.00 | 0.85 | |||||||
| Fe | Male | 50-200 | μg/dL | Test | 102.4 | ± | 46.6 | 89.2 | ± | 25.9 | 103.0 | ± | 31.8 | 99.4 | ± | 31.6 | 0.35 | 1.00 | 1.00 | |||
| Female | 40-180 | Placebo | 124.5 | ± | 54.6 | 112.5 | ± | 45.8 | 116.1 | ± | 39.5 | 107.1 | ± | 46.0 | 0.70 | 1.00 | 0.53 | |||||
| IP | 2.5-4.5 | mg/dL | Test | 3.59 | ± | 0.36 | 3.72 | ± | 0.53 | 3.63 | ± | 0.47 | 3.50 | ± | 0.48 | 0.38 | 1.00 | 0.33 | ||||
| Placebo | 3.35 | ± | 0.39 | 3.48 | ± | 0.36 | 3.43 | ± | 0.40 | 3.51 | ± | 0.45 | 0.21 | 0.51 | 0.11 | |||||||
Values are expressed as mean ± standard deviation. Parameters separated by sex are indicated by results for each sex only. AST/GOT, aspartate aminotransferase; ALT, alanine aminotransferase; γ-GT, gamma-glutamyl transpeptidase; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; Cre, creatinine; CK, creatine kinase; Total-Cho, total cholesterol; HDL-Cho, high-density lipoprotein cholesterol; LDL-Cho, low-density lipoprotein cholesterol; HbA1c, hemoglobin A1c; Na, sodium; Cl, chloride; K, potassium; Mg, magnesium; Ca, calcium; Fe, iron; IP, inorganic phosphorus. Significant differences in a Bonferroni-corrected paired t-test of intragroup changes are expressed as *p < 0.05 and †p < 0.10. The number of participants analyzed for each measurement item was 24.
Table 4: Laboratory test results (2)
| Urinalysis (quantitative parameters) | Reference range | Group | Week 0 | Week 4 | Week 8 | Week 13 | P-value (intragroup) | ||||||||||
| Week 4 | Week 8 | Week 13 | |||||||||||||||
| Urine specific gravity | 1.006-1.030 | Test | 1.0173 | ± | 0.0086 | 1.0172 | ± | 0.0091 | 1.0184 | ± | 0.0073 | 1.0182 | ± | 0.0088 | 1.00 | 1.00 | 1.00 |
| Placebo | 1.0180 | ± | 0.0099 | 1.0195 | ± | 0.0078 | 1.0179 | ± | 0.0074 | 1.0192 | ± | 0.0100 | 0.40 | 1.00 | 1.00 | ||
| Urine pH | 5.0 - 7.5 | Test | 6.10 | ± | 0.51 | 6.04 | ± | 0.64 | 6.00 | ± | 0.66 | 6.22 | ± | 0.58 | 1.00 | 1.00 | 1.00 |
| Placebo | 6.15 | ± | 0.80 | 6.13 | ± | 0.66 | 5.96 | ± | 0.75 | 6.02 | ± | 0.70 | 1.00 | 0.74 | 1.00 | ||
Values are expressed as mean ± standard deviation. Intragroup comparisons were analyzed using a Bonferroni-corrected paired t-test. The number of participants analyzed for each measurement item was 24.
Table 5: Laboratory test results 3
| P-value (between-group) | ||||||||
| Week 0 | Week 4 | Week 8 | Week 13 | |||||
| Hematology | White blood cell count | 0.25 | 5252 | 0.02 | * | 0.23 | 0.95 | |
| Red blood cell count | 0.45 | 0.55 | 0.47 | 0.64 | ||||
| Hemoglobin | 0.60 | 0.70 | 0.67 | 0.90 | ||||
| Hematocrit | 0.50 | 0.93 | 0.58 | 0.98 | ||||
| MCV | 0.75 | 0.22 | 0.59 | 0.27 | ||||
| MCH | 0.65 | 0.65 | 0.51 | 0.45 | ||||
| MCHC | 0.88 | 0.25 | 0.88 | 0.71 | ||||
| Platelet count | 0.12 | 0.11 | 0.04 | * | 0.10 | |||
| Blood biochemistry | Uric acid | 0.85 | 1.00 | 0.37 | 0.67 | |||
| Urea nitrogen | 0.87 | 0.90 | 0.95 | 0.33 | ||||
| AST | 0.29 | 0.68 | 0.22 | 0.19 | ||||
| ALT | 0.48 | 0.71 | 0.34 | 0.70 | ||||
| γ-GT | 0.94 | 0.62 | 0.89 | 0.87 | ||||
| ALP | 0.51 | 0.73 | 0.73 | 0.84 | ||||
| LDH | 0.67 | 0.68 | 0.54 | 0.34 | ||||
| Total bilirubin | 0.38 | 0.18 | 0.84 | 0.60 | ||||
| Total protein | 0.97 | 0.38 | 0.13 | 0.13 | ||||
| Albumin | 0.92 | 0.71 | 0.68 | 0.34 | ||||
| Cre | 0.68 | 0.79 | 0.68 | 0.72 | ||||
| CK | 0.33 | 0.81 | 0.67 | 0.39 | ||||
| Serum amylase | 0.83 | 0.80 | 0.94 | 0.55 | ||||
| Total-Cho | 0.45 | 0.54 | 0.26 | 0.66 | ||||
| HDL-Cho | 0.80 | 0.52 | 0.55 | 0.65 | ||||
| LDL-Cho | 0.82 | 0.95 | 0.61 | 0.79 | ||||
| Triglyceride | 0.55 | 0.61 | 0.31 | 0.78 | ||||
| Blood glucose | 0.54 | 0.58 | 0.87 | 0.84 | ||||
| HbA1c | 0.40 | 0.42 | 0.25 | 0.40 | ||||
| Na | 0.94 | 0.80 | 0.22 | 0.92 | ||||
| Cl | 1.00 | 0.30 | 0.25 | 0.73 | ||||
| K | 0.15 | 0.48 | 0.93 | 0.11 | ||||
| Mg | 0.53 | 0.15 | 0.77 | 0.35 | ||||
| Ca | 0.78 | 0.43 | 0.74 | 0.58 | ||||
| Fe | 0.14 | 0.04 | * | 0.22 | 0.51 | |||
| IP | 0.03 | * | 0.08 | † | 0.13 | 0.92 | ||
| Urinalysis (quantitative parameters) | Urine specific gravity | 0.77 | 0.35 | 0.80 | 0.72 | |||
| Urine pH | 0.83 | 0.64 | 0.83 | 0.31 | ||||
Values indicate the p-value for each measurement item. MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; AST/GOT, aspartate aminotransferase; ALT, alanine aminotransferase; γ-GT, gamma-glutamyl transpeptidase; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; Cre, creatinine; CK, creatine kinase; Total-Cho, total cholesterol; HDL-Cho, high-density lipoprotein cholesterol; LDL-Cho, low-density lipoprotein cholesterol; HbA1c, hemoglobin A1c; Na, sodium; Cl, chloride; K, potassium; Mg, magnesium; Ca, calcium; Fe, iron; IP, inorganic phosphorus. Between-group comparisons were performed using an unpaired t-test. Significant differences in between groups are expressed as *p < 0.05 and †p < 0.10.
Table 6: P-values for between-group comparisons of laboratory test values
Regarding the urine qualitative parameters, qualitative urinary protein was noted with (+) in one participant at Week 8, urinary occult blood reaction was observed with (+++) in one participant at Week 4 and (++) in one participant at Week 13, and urinary ketone bodies were noted with (+) in one participant at Week 13 in the test food group (Appendix 1). In the placebo food group, qualitative urinary protein was observed with (++) in one participant at Week 4 and (+) in one participant at Week 13, urobilinogen was noted with (+) in one participant at Week 4, and urinary occult blood reaction was observed with (+++) in two participants at Week 4, (+) in one participant at Week 8, and (+) and (++) in one participant each at Week 13 (Appendix 2).
| Week 2 | Week 8 | Week 13 | ||||||||||||||
| Parameter | Week 0 | (-) | (±) | (+) | (++) | (+++) | (-) | (±) | (+) | (++) | (+++) | (-) | (±) | (+) | (++) | (+++) |
| Urine protein, qualitative | (-) | 23 | 0 | 0 | 0 | 0 | 22 | 0 | 1 | 0 | 0 | 19 | 3 | 0 | 0 | 0 |
| (±) | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urine glucose, qualitative | (-) | 24 | 0 | 0 | 0 | 0 | 23 | 1 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urobilinogen, qualitative | (-) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (±) | 0 | 24 | 0 | 0 | 0 | 0 | 24 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urine bilirubin, qualitative | (-) | 24 | 0 | 0 | 0 | 0 | 24 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urinary occult blood reaction, qualitative | (-) | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 | 21 | 0 | 0 | 1 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urine ketone body, qualitative | (-) | 24 | 0 | 0 | 0 | 0 | 24 | 0 | 0 | 0 | 0 | 22 | 0 | 1 | 0 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
The presence of the desired component is indicated as positive (+), and the more (+) there are, the higher the content of the component. False-positive cases are expressed as (±). Numbers represent the number of applicable participants.
Appendix 1: Cross-tabulation table for urinalysis values [test food group (n = 24)]
| Week 4 | Week 8 | Week 13 | ||||||||||||||
| Parameter | Week 0 | (-) | (±) | (+) | (++) | (+++) | (-) | (±) | (+) | (++) | (+++) | (-) | (±) | (+) | (++) | (+++) |
| Urine protein, qualitative | (-) | 20 | 1 | 0 | 1 | 0 | 21 | 1 | 0 | 0 | 0 | 19 | 2 | 1 | 0 | 0 |
| (±) | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urine glucose, qualitative | (-) | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urobilinogen, qualitative | (-) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (±) | 0 | 22 | 1 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urine bilirubin, qualitative | (-) | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urinary occult blood reaction, qualitative | (-) | 21 | 0 | 0 | 0 | 2 | 22 | 0 | 1 | 0 | 0 | 20 | 1 | 1 | 1 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Urine ketone body, qualitative | (-) | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 |
| (±) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| (+++) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
The presence of the desired component is indicated as positive (+), and the more (+) there are, the higher the content of the component. False-positive cases are expressed as (±). Numbers represent the number of applicable participants.
Appendix 2: Cross-tabulation table for urinalysis values [placebo food group (n = 24)]
7. Adverse Events
Table 7 lists the adverse events observed during the trial period. Before intake of the trial food, three adverse events were reported in the test food group and two in the placebo food group. During the period of intake of the trial food, six adverse events were reported in the test food group and 22 in the placebo food group. All 33 events were considered to be “not related” to the trial food. There were no drugs or health foods taken during the trial period that were considered to have affected the results.
| ID | Sex | Age | Group | Period | Name (symptoms) |
Date of onset | Date of resolution (Date of outcome confirmation) |
Severity of symptoms | Seriousness | Treatment | Outcome | Causal relationship with the trial food | Comments |
| 13004 | Female | 22 | Test food |
During the intake period | Cough and hoarseness | 5/3/2022 | 5/4/2022 | Moderate | No | Yes: Take medicine (May 3 and 4) | Recovered /Resolved |
No | The events were considered not related to the trial food because the symptoms were due to dryness. |
| 13017 | Male | 49 | Test food |
During the intake period | Abdominal pain | 5/11/2022 | 5/11/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was caused by excessive drinking of cold water. |
| 13025 | Male | 46 | Placebo food |
During the intake period | Pharyngeal pain and pyrexia | 7/17/2022 | 7/19/2022 | Moderate | No | Yes: Take medicine (July 17 to 19) | Recovered /Resolved |
No | The events were considered not related to the trial food because the symptoms were caused by coronavirus infection. |
| 13031 | Female | 40 | Test food |
Before intake | Malaise Abdominal pain |
4/15/2022 | 4/15/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptoms had occurred before the intake of the trial food. |
| 13040 | Female | 32 | Placebo food |
Before intake | Pyrexia | 4/22/2022 | 4/22/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom had occurred before the intake of the trial food. |
| 13042 | Male | 41 | Test food |
Before intake | Headache Pyrexia Rhinorrhea Pharyngeal pain |
4/19/2022 | 4/21/2022 | Mild | No | No | Recovered /Resolved |
No | The events were considered not related to the trial food because the symptoms had occurred before the intake of the trial food. |
| 13047 | Female | 28 | Placebo food |
During the intake period | Vomiting and diarrhea | 5/6/2022 | 5/6/2022 | Mild | No | No | Recovered /Resolved |
No | The events were considered not related to the trial food because the symptoms were due to oily diet. |
| During the intake period | Queasy stomach and abdominal pain | 6/3/2022 | 6/3/2022 | Moderate | No | Yes: Take medicine (June 3) | Recovered /Resolved |
No | The events were considered not related to the trial food because the symptoms were transient. | ||||
| During the intake period | Itching | 6/28/2022 | 6/28/2022 | Moderate | No | Yes: Take medicine, topical agent (June 28) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to atopy. | ||||
| 13050 | Female | 46 | Placebo food |
During the intake period | Pharyngeal pain | 5/2/2022 | 5/5/2022 | Moderate | No | Yes: Take medicine (May 2 to 5) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was transient cold-like symptom. |
| During the intake period | Headache | 6/27/2022 | 6/27/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to mountain climbing. | ||||
| 13059 | Female | 34 | Placebo food |
Before intake | Anemia | 4/15/2022 | 4/15/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom had occurred before the intake of the trial food. |
| 13065 | Female | 36 | Placebo food |
During the intake period | Diarrhea | 5/18/2022 | 5/18/2022 | Moderate | No | Yes: Take medicine (May 18) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to cold. |
| During the intake period | Diarrhea | 6/21/2022 | 6/21/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to cold. | ||||
| During the intake period | Menstrual pain | 7/8/2022 | 7/8/2022 | Moderate | No | Yes: Take medicine (July 8) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to menstruation. | ||||
| 13067 | Male | 32 | Test food |
During the intake period | Migraine | 4/23/2022 | 4/23/2022 | Moderate | No | Yes: Take medicine (April 23) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to fatigue. |
| During the intake period | Migraine | 5/5/2022 | 5/5/2022 | Moderate | No | Yes: Take medicine (May 5) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to fatigue. | ||||
| 13072 | Female | 54 | Test food |
During the intake period | Stomach heaviness | 6/9/2022 | 6/9/2022 | Moderate | No | Yes: Take medicine (June 9) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to overeating. |
| 13075 | Female | 54 | Placebo food |
During the intake period | Diarrhea | 6/17/2022 | 6/17/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to meals. |
| During the intake period | Heat illness | 7/1/2022 | 7/1/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to walking under the blazing sun. | ||||
| 13078 | Male | 26 | Placebo food |
During the intake period | Headache | 4/27/2022 | 4/27/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was caused by changes in atmospheric pressure. |
| During the intake period | Diarrhea | 5/1/2022 | 5/1/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to cold. | ||||
| During the intake period | Itching | 5/2/2022 | 5/2/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was caused by changes in temperature. | ||||
| During the intake period | Neck pain | 5/8/2022 | 5/8/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was caused by the change in chills caught in sleep. | ||||
| During the intake period | Flank pain | 5/11/2022 | 5/11/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was transient. | ||||
| During the intake period | Pharyngeal pain | 5/19/2022 | 5/19/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was transient. | ||||
| 13095 | Male | 59 | Test food |
During the intake period | Abdominal distension | 5/8/2022 | 5/8/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to constipation. |
| 13100 | Female | 42 | Placebo food |
During the intake period | Stomatitis | 4/23/2022 | 4/24/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was transient. |
| During the intake period | Diarrhea and throat pain | 6/9/2022 | 6/10/2022 | Moderate | No | Yes: Take medicine (June 9 and 10) | Recovered /Resolved |
No | The events were considered not related to the trial food because the symptoms were transient cold-like symptom. | ||||
| During the intake period | Migraine | 6/27/2022 | 6/27/2022 | Moderate | No | Yes: Take medicine (June 27) | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was transient. | ||||
| During the intake period | Abdominal pain | 7/3/2022 | 7/3/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was due to overeating. | ||||
| During the intake period | Stomatitis | 7/11/2022 | 7/12/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom was transient. | ||||
| 13102 | Female | 31 | Test food |
Before intake | Nausea Abdominal pain |
4/20/2022 | 4/20/2022 | Mild | No | No | Recovered /Resolved |
No | The event was considered not related to the trial food because the symptom had occurred before the intake of the trial food. |
Table 7: List of adverse events
Discussion
The aim of the present parallel-group comparative trial using a placebo food of dextrin 268.4mg/day in healthy male and female adults aged 20–64 years was to confirm the safety of a test food (two tablets [268.4mg] per day of FB-GABA- containing food) given for a long term of 13 weeks.
At all time points of predose Week 0, Week 4, Week 8, and Week 13, no significant intragroup changes were observed in any body measurement or physical examination value and no significant between-group differences were found. Based on these findings, the investigator concluded that long-term dosing of the test food caused no problems in body measurements or physical examinations.
In the intergroup comparison between the test and placebo food groups, IP levels at pre-dose Week 0 were significantly higher in the test food group, but the levels were within the reference range in all participants. At Week 4, significantly lower Fe and significantly higher WBC were observed in the test food group. However, these levels were within the reference ranges in all participants. The platelet count was significantly higher in the test food group at Week 8. The level above the reference range at Week 8 occurred in one participant and the level in this participant had exceeded the reference range since SCR. Despite the high test value, no particular adverse events occurred. Therefore, the difference was not considered to be clinically significant by the investigator. The other parameters indicated no significant differences in values at pre-dose Week 0, Week 4, Week 8, or Week 13.
In the test food group, intragroup comparisons in each test from the start of intake to post-intake showed a significant increase in albumin at Week 13. Ht and Mg significantly increased at Weeks 8 and 13, and MCV significantly increased at Weeks 4, 8, and 13. On the other hand, HbA1c significantly decreased at Week 13, and MCHC significantly decreased at Weeks 4, 8, and 13. In the placebo food group, Cl levels significantly increased at Week 4, and Mg levels significantly increased at Weeks 4 and 13. In addition, MCV significantly increased at Weeks 4, 8, and 13. On the other hand, AST and Na levels significantly decreased at Week 13. In addition, HbA1c significantly decreased at Weeks 4 and 13, and MCHC significantly decreased at Weeks 8 and 13.
Of the parameters showing intragroup changes in the test food group, albumin significantly increased at Week 13. However, no participants had a level above the reference range at Week 13; therefore, it was judged that there would be no problem with safety.
Ht levels significantly increased at Weeks 8 and 13 in the test food group, but the levels were not above the reference range in any participants at Week 8. The level above the reference range at Week 13 occurred in one participant. Despite the high test value, no particular adverse events occurred. Therefore, the change was not considered to be clinically problematic by the investigator.
Mg significantly increased at Weeks 8 and 13 in the test food group and at Weeks 4 and 13 in the placebo food group. However, the levels did not exceed the reference range in any participant. The investigator, therefore, determined that there would be no safety problem.
MCV significantly increased at Weeks 4, 8, and 13 in the test food group, but the levels were not above the reference range in any of the participants at Weeks 4 or 8. The level above the reference range at Week 13 occurred in two participants. Despite the high test value, no particular adverse events occurred. Therefore, the change was not considered to be clinically problematic by the investigator. In the placebo food group as well, MCV significantly increased at Weeks 4, 8, and 13. In one of two participants who continued to have levels above the reference range from Weeks 4 to 13, the level exceeded the reference range from pre-dose Week 0, but no particular adverse event occurred. The other one participant also had no particular adverse event despite the high test value. Therefore, the change was not considered to be clinically problematic by the investigator.
HbA1c significantly decreased at Week 13 in the test food group and at Weeks 4 and 13 in the placebo food group, but the levels were not below the lower limit of the reference range in any of the participants. Therefore, the change was not considered to be clinically problematic by the investigator.
MCHC significantly decreased in the test food group at Weeks 4, 8, and 13. The level below the lower limit of the reference range at Weeks 4 and 8 occurred in the same participant and returned to the reference range at Week 13. No participants had a level below the reference range at Week 13. Therefore, the change was not considered to be clinically problematic by the investigator. In the placebo food group, MCHC significantly decreased at Weeks 8 and 13. The level below the lower limit of the reference range at Week 8 occurred in one participant and returned to the reference range at Week 13. No participants had a level below the reference range at Week 13. Therefore, the change was not considered to be clinically problematic by the investigator.
Of the parameters showing intragroup changes in the placebo food group, a significant increase in Cl was observed at Week 4, and significant decreases in AST and Na were noted at Week 13. However, none of the participants had a level beyond the upper or lower limit of the reference range, no between-group differences were observed, and the changes were slight. Therefore, the changes were not considered to be clinically problematic by the investigator.
Other parameters sporadically deviated from the reference range after the start of intake in multiple participants, but all deviations were within the range of physiological variations. Therefore, the investigator did not consider these deviations to be clinically problematic.
Qualitative tests for urinary protein showed positive results as follows: (++) for ID13078 (placebo food group) at Week 4, (+) for ID13032 (test food group) at Week 8, and (+) for ID13078 (placebo food group) at Week 13. However, these were considered to be incidental symptoms because none of the participants had any abnormalities in related parameters. Therefore, the results were not determined to be clinically problematic. Urobilinogen was positive (+) in participant ID13059 (placebo food group) at Week 4. However, no abnormalities were observed in any related parameters, and the value returned to the reference range at Week 8 or later. Therefore, the result was judged to be an incidental symptom with no clinical problems. Qualitative tests for urinary occult blood reaction showed positive results as follows: (+++) for ID13103 (test food group), (+++) for ID13100 (placebo food group), and (+++) for ID13021 (placebo food group) at Week 4, and (+) for ID13021 (placebo food group) at Week 8. After Week 13, (++) was noted for ID13102 (test food group), (+) for ID13059 (placebo food group), and (++) for ID13050 (placebo food group). For five participants (ID13050, ID13059, ID13100, ID13102, and ID13103), the results were attributable to menstruation and not considered to be clinically problematic. Participant ID13021 was confirmed to have reached menopause shortly before the study began. In the period shortly after menopause, bleeding may occur because of detachment of the endometrium due to vaginitis or decreased hormone secretion. These changes are likely to have affected the result. The result returned to the reference value at Week 8, and no abnormalities were seen in related parameters. Therefore, the result was judged to have no clinical problems. Participant ID13005 (test food group) was positive (+) for urine ketone bodies at Week 13, but this was deemed to be an influence of fasting and therefore not clinically problematic.
A total of 33 adverse events occurred in this trial, all of which had mild to moderate symptoms that occurred before intake of the trial food, had a definite cause, or were transient. Therefore, the causal relationship with the trial food was determined to be “not related.”
Based on the above, the investigator concluded that there was no problem regarding the safety of long-term dosing of the trial food for 13 weeks from the viewpoints of the primary end points, that is, body measurements, physical examinations, laboratory tests, and adverse events. To our knowledge, no preceding trial has been conducted on the safety of long-term intake (13 weeks) of foods that contain FB-GABA in healthy adult male and female participants. The results of this trial can be applied to all foods containing FB-GABA. Confirmation of safety in this trial will enable the appropriate provision of information to consumers and is expected to be of academic significance.
Conclusion
From the results of this trial, we concluded that consuming 268.4mg of FB-GABA daily for 13 weeks is safe from the viewpoints of body measurements, physical examinations, laboratory tests, and adverse events.
Funding
Trial funding was provided by Sanwa Shurui Co., Ltd. Uehara and Hokazono are employees of Sanwa Shurui Co., Ltd. The other author has no conflicts of interest to disclose.
Conflict of Interest
Sanwa Shurui Co., Ltd. concluded an outsourcing contract with Oneness Support Co., Ltd. (Osaka, Japan) to outsource the trial. Oneness Support Co., Ltd., concluded an operating agreement with Miura Clinic, Medical Corporation Kanonkai (trial site, Osaka, Japan) and LSI Medience Corporation (laboratory, Tokyo, Japan) and conducted the trial. Compensation based on these operating agreements was a legitimate business compensation for the implementation of the trial and did not affect the trial results.
References
- Bloom EF and Iversen LL. “Localizing 3H-GABA in nerve terminals of rat cerebral cortex by electron microscopic autoradiography”. Nature 229.5287 (1971): 628-630.
- Tessa H de Bie., et al. “Effects of γ-aminobutyric acid supplementation on glucose control in adults with prediabetes: A double-blind, randomized, placebo-controlled trial”. The American Journal of Clinical Nutrition 118.3 (2023): 708-719.
- Furuta Y., et al. “Novel Conversion Processes with Lactic Acid Bacteria from Shochu Kasu into Valuable Materials”. Seibutsu-kogaku Kaishi (in Japanese) 88.3 (2010): 114–120.
- Hokazono H and Fukuda R. “Effects of oral intake of GABA on sleep in healthy adults - a randomized, double-blind, placebo-controlled, crossover study”. Japanese Pharmacology & Therapeutics 46(2018) :757-770.
- Hokazono H and Saito J. “Effects of γ-aminobutyric acid (GABA)-containing food on mood status and sleepquality in workers - A double-blind randomized controlled trial”. Japanese Pharmacology & Therapeutics 44 (2016):1445-1454.
- Hokazono H and Uehara E. “Dermal effects of oral administration of GABA in humans”. Nippon Shokuhin Kagaku Kogaku Kaishi, 63.7 (2016):306-311.
- Hellen A Oketch-Rabah., et al. “United States Pharmacopeia (USP) safety review of gamma-aminobutyric acid (GABA)”. Nutrients 13.8 (2021): 2742.
- The Vice-Commissioner of Consumer Affairs Agency in Japan. Attachment 2 “Points to consider in preparing application forms for foods for specified health uses” for the labeling permission of foods for specified health uses (Food Labeling Division Notification No. 259) issued on October 30, 2014 (in Japanese).
- Uehara E., et al. “Safety evaluation of overdose intake of fermented barley GABA 90% - a placebo-controlled, double-blind, randomized, parallel-group comparative trial-”. Nutrition and Food Toxicology 5.1 (2024): 1-21.
- Yamatsu A., et al. “Intake of 200 mg/day of γ-Aminobutyric Acid (GABA) improves a wide range of cognitive functions: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial”. Japanese Pharmacology & Therapeutics 48 (2020) :461-474.
Citation:
Eriko Uehara., et al. “Safety Evaluation of Long-term Intake of Fermented Barley GABA 90% –A Placebo-controlled, Double-blind, Randomized, Parallel-group Comparative Trial–”. Nutrition and Food Toxicology 5.1 (2024): 22-42.
Copyright: © 2024 Eriko Uehara., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.




































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.